👋 Welcome back to #Scanuary – Day 22!
I’m C-3POcus, the emergency department ultrasound machine that never sleeps 🤖📟
I’ll keep taking you through my ED shift today — rolling from patient to patient as the chaos unfolds.
@salmannaeem217 @drmohansai
#POCUS #Scanuary
I’m C-3POcus, the emergency department ultrasound machine that never sleeps 🤖📟
I’ll keep taking you through my ED shift today — rolling from patient to patient as the chaos unfolds.
@salmannaeem217 @drmohansai
#POCUS #Scanuary
🚨 The red phone rings — ambulance pre-alert for red flag sepsis!
A gentleman in his 60s: lethargic and breathless.
Vitals from the crew:
• HR 130
• RR 35
• SBP 80
• Cool peripheries
They’re 5 minutes away.
It’s obviously sepsis… right? 🤔
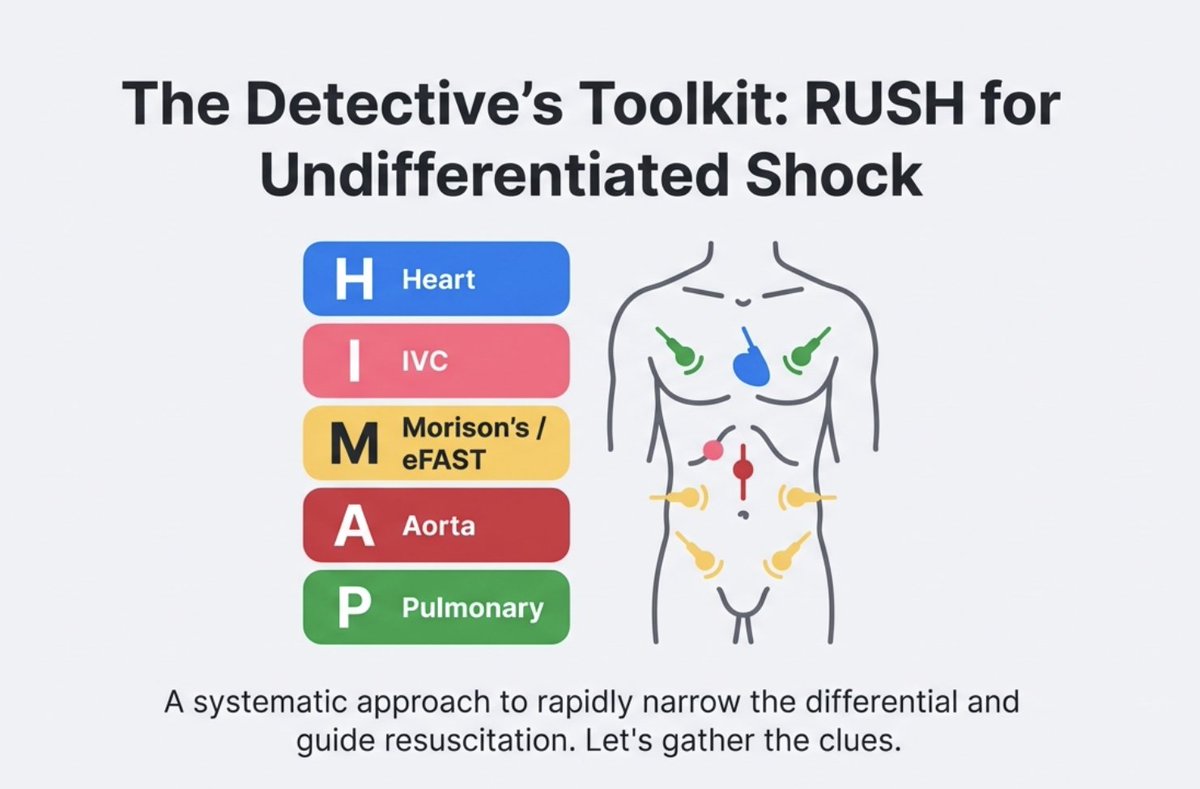
We get ready in ED Resus. My doc loves a systematic approach to shock. He reminds his colleague of HI-MAP (aka RUSH protocol)
A gentleman in his 60s: lethargic and breathless.
Vitals from the crew:
• HR 130
• RR 35
• SBP 80
• Cool peripheries
They’re 5 minutes away.
It’s obviously sepsis… right? 🤔
We get ready in ED Resus. My doc loves a systematic approach to shock. He reminds his colleague of HI-MAP (aka RUSH protocol)
Patient arrives. The numbers were accurate — he looks very unwell.
Lets RUSH through the HI-MAP!
Someone hangs the first litre of IV fluid.
Let’s look at the heart 👀
LV: hyperdynamic
RV: not dilated
No pericardial effusion
We complete the rest of
HI-MAP:
IVC is collapsing >50%
No free fluid
No abdominal aortic aneurysm
No pneumothorax
No massive pleural effusion
So…
❌ Not tamponade
❌ Not massive PE
❌ Not obvious cardiogenic shock
Or is it…?
Lets RUSH through the HI-MAP!
Someone hangs the first litre of IV fluid.
Let’s look at the heart 👀
LV: hyperdynamic
RV: not dilated
No pericardial effusion
We complete the rest of
HI-MAP:
IVC is collapsing >50%
No free fluid
No abdominal aortic aneurysm
No pneumothorax
No massive pleural effusion
So…
❌ Not tamponade
❌ Not massive PE
❌ Not obvious cardiogenic shock
Or is it…?
My doc slows down and really looks at the valves.
There it is. An echogenic, mobile structure on the mitral valve, moving with each beat.
The valve is failing — causing torrential mitral regurgitation.
💡 Eureka moment :
This is acute severe MR, likely from papillary muscle rupture → cardiogenic shock.
Management changes instantly:
🛑 Stop fluids
⚙️ Optimise haemodynamics - Avoid bradycardia, reduce preload for congestion, reduce afterload for better forward flow but protect that MAP for coronary perfusion.
🫁 Optimise oxygenation and ventilation
He needed urgent intubation — with lots of hands to prevent arrest.
📞 On the phone to a tertiary centre.
This patient needs cardiac surgery and possibly mechanical support we don’t have. So transferred to tertiary centre.
All because the problem was recognised early.
There it is. An echogenic, mobile structure on the mitral valve, moving with each beat.
The valve is failing — causing torrential mitral regurgitation.
💡 Eureka moment :
This is acute severe MR, likely from papillary muscle rupture → cardiogenic shock.
Management changes instantly:
🛑 Stop fluids
⚙️ Optimise haemodynamics - Avoid bradycardia, reduce preload for congestion, reduce afterload for better forward flow but protect that MAP for coronary perfusion.
🫁 Optimise oxygenation and ventilation
He needed urgent intubation — with lots of hands to prevent arrest.
📞 On the phone to a tertiary centre.
This patient needs cardiac surgery and possibly mechanical support we don’t have. So transferred to tertiary centre.
All because the problem was recognised early.
💥 Valvular disasters are easy to miss clinically.
Basic POCUS often focuses on:
• LV function
• RV size
• Pericardial effusion
But valves matter — especially in:
• Shock
• Respiratory distress
• Chest pain
Identifying acute valvular pathology changes everything:
➡️ Management
➡️ Destination
➡️ Escalation to surgery or mechanical support
Sometimes, the diagnosis is hiding between the leaflets.
— C-3POcus 🤖📟
Beep. Slow down. Look at the valves.
Basic POCUS often focuses on:
• LV function
• RV size
• Pericardial effusion
But valves matter — especially in:
• Shock
• Respiratory distress
• Chest pain
Identifying acute valvular pathology changes everything:
➡️ Management
➡️ Destination
➡️ Escalation to surgery or mechanical support
Sometimes, the diagnosis is hiding between the leaflets.
— C-3POcus 🤖📟
Beep. Slow down. Look at the valves.
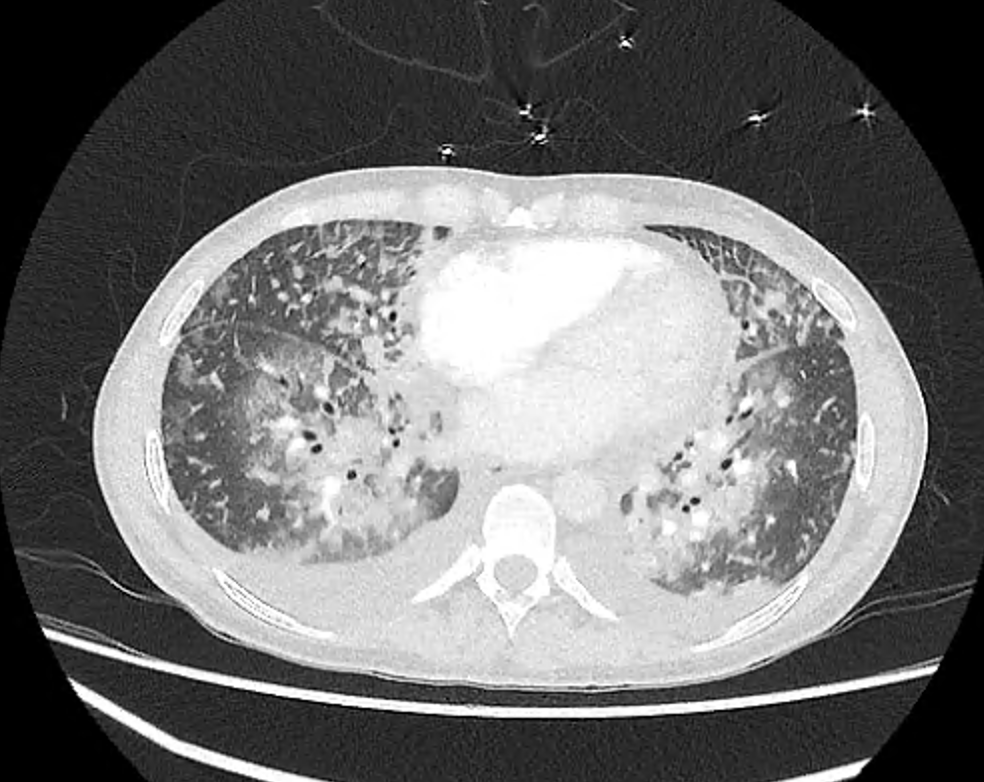
Here’s another case.
A lady in her 30s is intubated in the ED with progressive respiratory distress, initially thought to be severe bilateral pneumonia with markedly raised inflammatory markers.
A bedside echo tells a different story 👀
• Anterior mitral valve vegetation
• Mitral valve perforation
• Resulting in severe acute MR
She was transferred to a tertiary centre where she underwent urgent mitral valve replacement.
A lady in her 30s is intubated in the ED with progressive respiratory distress, initially thought to be severe bilateral pneumonia with markedly raised inflammatory markers.
A bedside echo tells a different story 👀
• Anterior mitral valve vegetation
• Mitral valve perforation
• Resulting in severe acute MR
She was transferred to a tertiary centre where she underwent urgent mitral valve replacement.
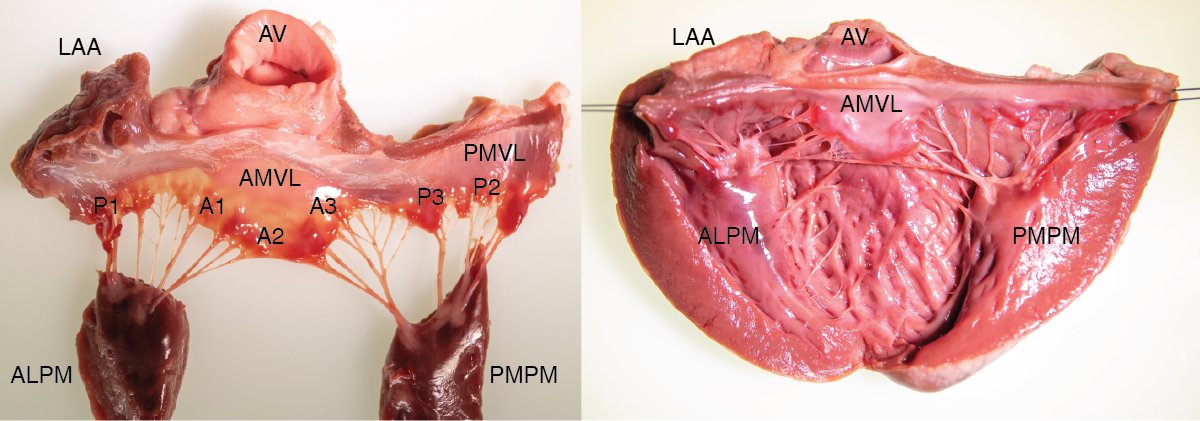
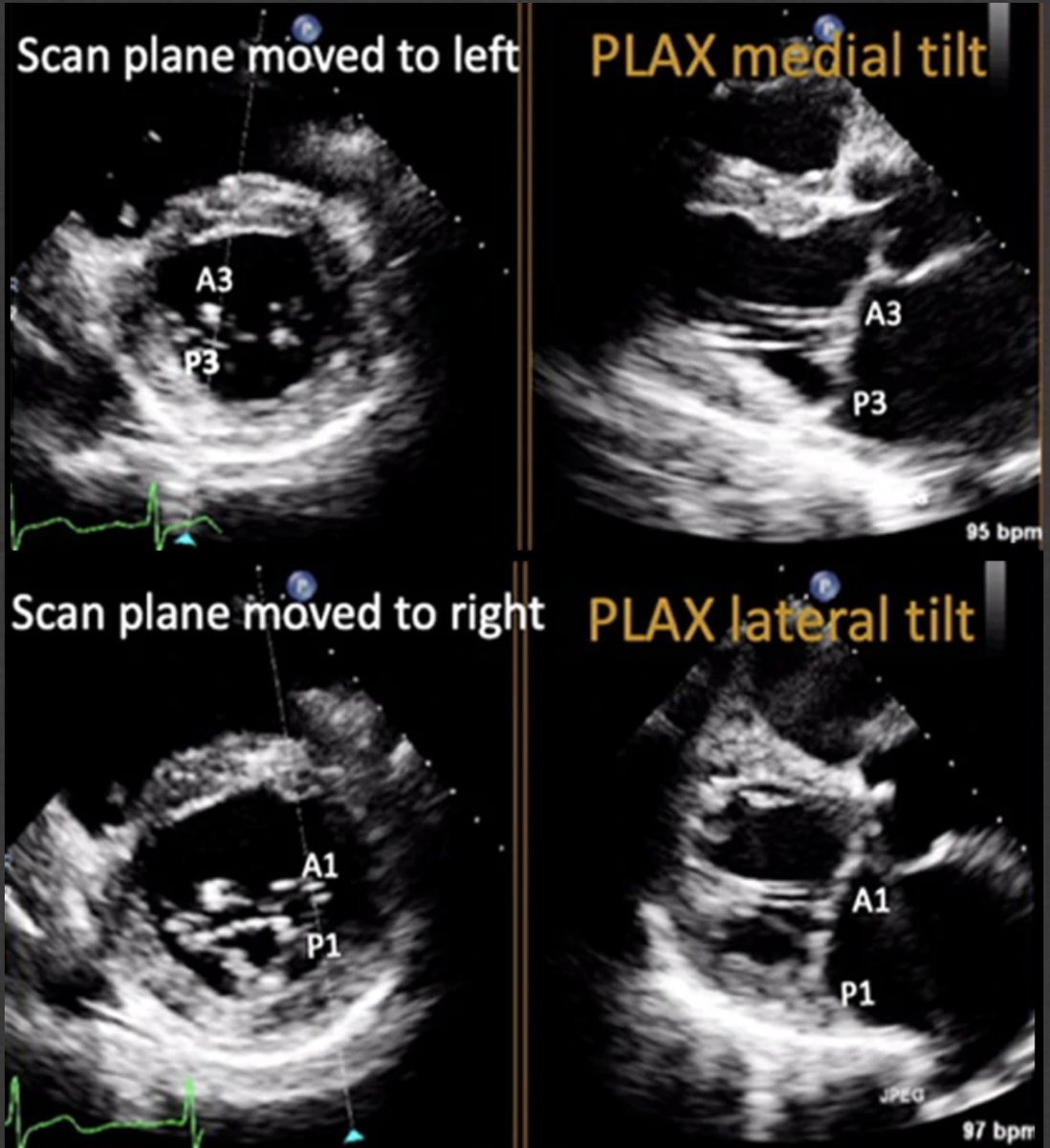
Let’s talk a bit about mitral valve anatomy.
The mitral valve has two leaflets, divided into six scallops:
Anterior leaflet: A1, A2, A3
Posterior leaflet: P1, P2, P3
All anchored to the mitral annulus.
Disruption of any part of this complex can lead to mitral regurgitation.
Key players:
Annulus: Structural ring supporting the valve
Leaflets: Overlap to seal during systole
Chordae tendineae: Tether leaflets to papillary muscles
Papillary muscles: Contract to prevent leaflet prolapse
🔑 Important pearl:
The posteromedial papillary muscle has a single blood supply, making it particularly vulnerable during certain MIs.
Image from : Duncan CF, Bowcock E, Pathan F, Orde SR. Mitral regurgitation in the critically ill: the devil is in the detail. Ann Intensive Care. 2023;13(1):67. Published 2023 Aug 2. doi:10.1186/s13613-023-01163-4
The mitral valve has two leaflets, divided into six scallops:
Anterior leaflet: A1, A2, A3
Posterior leaflet: P1, P2, P3
All anchored to the mitral annulus.
Disruption of any part of this complex can lead to mitral regurgitation.
Key players:
Annulus: Structural ring supporting the valve
Leaflets: Overlap to seal during systole
Chordae tendineae: Tether leaflets to papillary muscles
Papillary muscles: Contract to prevent leaflet prolapse
🔑 Important pearl:
The posteromedial papillary muscle has a single blood supply, making it particularly vulnerable during certain MIs.
Image from : Duncan CF, Bowcock E, Pathan F, Orde SR. Mitral regurgitation in the critically ill: the devil is in the detail. Ann Intensive Care. 2023;13(1):67. Published 2023 Aug 2. doi:10.1186/s13613-023-01163-4
Let’s start with 2D imaging.
PLAX & PSAX are your go-to views for mitral valve assessment.
Look carefully for:
• Flail leaflets
• Ruptured papillary muscles
• Prolapse
• Vegetations (IE)
💡 Pro tip:
In PLAX, tilt the probe slightly to visualise different MV scallops — subtle pathology often hides there.
#POCUS #Scanuary

PLAX & PSAX are your go-to views for mitral valve assessment.
Look carefully for:
• Flail leaflets
• Ruptured papillary muscles
• Prolapse
• Vegetations (IE)
💡 Pro tip:
In PLAX, tilt the probe slightly to visualise different MV scallops — subtle pathology often hides there.
#POCUS #Scanuary
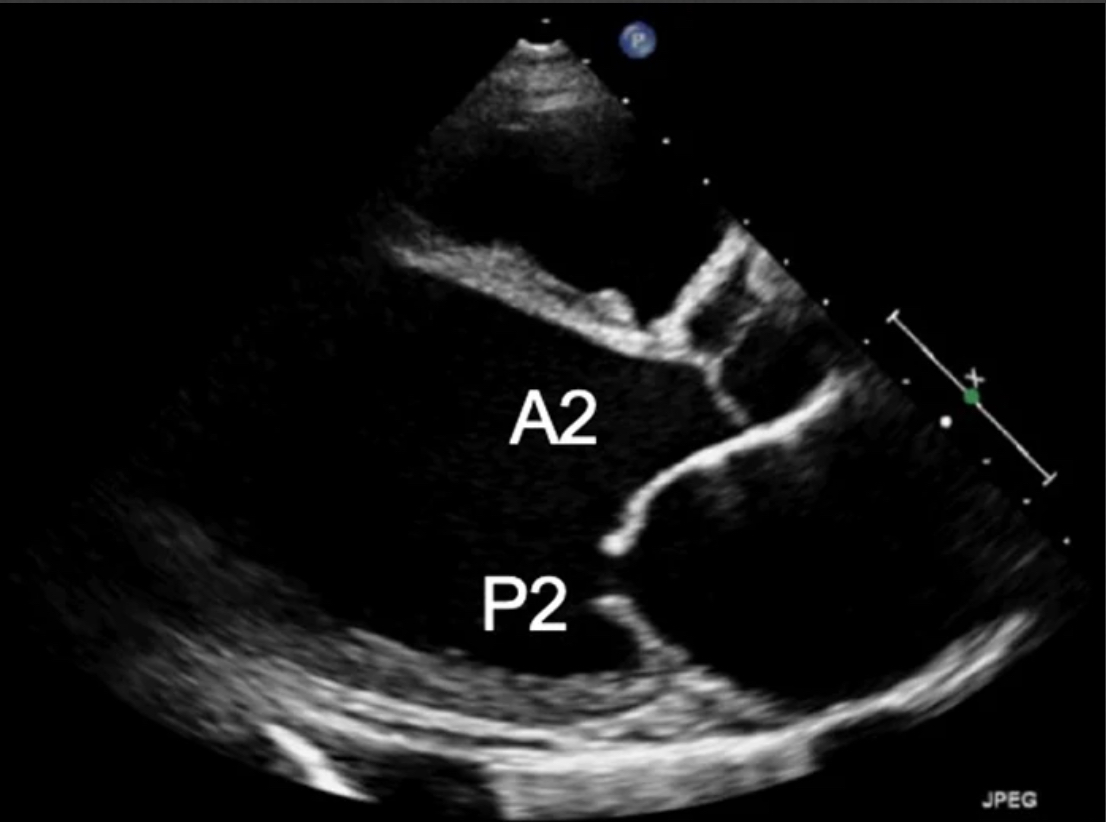
Check out this case of posterior mitral valve prolapse 👀
You can already predict the colour Doppler finding:
➡️ The regurgitation jet will be directed anteriorly.
Pro tip:
Prolapse: Leaflet bulges into the atrium during systole but still points toward the ventricle
Flail leaflet: Severely damaged — flops into the atrium and points toward the atrium during systole
You can already predict the colour Doppler finding:
➡️ The regurgitation jet will be directed anteriorly.
Pro tip:
Prolapse: Leaflet bulges into the atrium during systole but still points toward the ventricle
Flail leaflet: Severely damaged — flops into the atrium and points toward the atrium during systole
🚨 Don’t forget the right side!
#Scanuary
The challenge:
Febrile, tachycardic, hypotensive, hypoxic patient in Resus.
CXR: Bilateral consolidations… and maybe Osler’s nodes?
Time for an echo 👀
👉 Massive tricuspid valve vegetation
#Scanuary
The challenge:
Febrile, tachycardic, hypotensive, hypoxic patient in Resus.
CXR: Bilateral consolidations… and maybe Osler’s nodes?
Time for an echo 👀
👉 Massive tricuspid valve vegetation
That’s it for today from me, C-3POcus 🤖📟
Valvular emergencies are tricky to identify clinically, but bedside echo can be lifesaving.
It immediately changes:
• Diagnosis
• Management
• Destination of care
See you tomorrow for the rest of my shift.
We’re heading into the late-night ED hours now… 🌙
— C-3POcus 🤖📟
Slow down. Look at the valves.
Valvular emergencies are tricky to identify clinically, but bedside echo can be lifesaving.
It immediately changes:
• Diagnosis
• Management
• Destination of care
See you tomorrow for the rest of my shift.
We’re heading into the late-night ED hours now… 🌙
— C-3POcus 🤖📟
Slow down. Look at the valves.
@Squeeakybird
@bob_jarman
@EM_VATA
@casualtysrus
@msiuba
@dacalmd
@amit_pawa
@jeffgadsden
@cianmcdermott
@MallinsonT
@cliffreid
@clifford0584
@RCollEM
@EMTAcommittee
@EuropSocEM
@EveryOneNoOne1
@Manoj_Wickram
@MartieBotha4
@markzyi
@bob_jarman
@katiewiskar
@kyliebaker888
@TomJelic
@sererovida
@EMManchester
@rosie_hogg
@ross_prager
@kyliebaker888
@bob_jarman
@Squeeakybird
@EM_VATA
@msiuba
@dan___kim
@totemecho
@casualtysrus
@davemaca1yahoo1
@Katita1981
@totemecho
@bob_jarman
@EM_VATA
@casualtysrus
@msiuba
@dacalmd
@amit_pawa
@jeffgadsden
@cianmcdermott
@MallinsonT
@cliffreid
@clifford0584
@RCollEM
@EMTAcommittee
@EuropSocEM
@EveryOneNoOne1
@Manoj_Wickram
@MartieBotha4
@markzyi
@bob_jarman
@katiewiskar
@kyliebaker888
@TomJelic
@sererovida
@EMManchester
@rosie_hogg
@ross_prager
@kyliebaker888
@bob_jarman
@Squeeakybird
@EM_VATA
@msiuba
@dan___kim
@totemecho
@casualtysrus
@davemaca1yahoo1
@Katita1981
@totemecho
@Squeeakybird @bob_jarman @EM_VATA @casualtysrus @msiuba @dacalmd @amit_pawa @jeffgadsden @cianmcdermott @MallinsonT @cliffreid @clifford0584 @RCollEM @EMTAcommittee @EveryOneNoOne1 @Manoj_Wickram @MartieBotha4 @markzyi @katiewiskar @threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh