Brain Fog after COVID-19: What’s driving it?
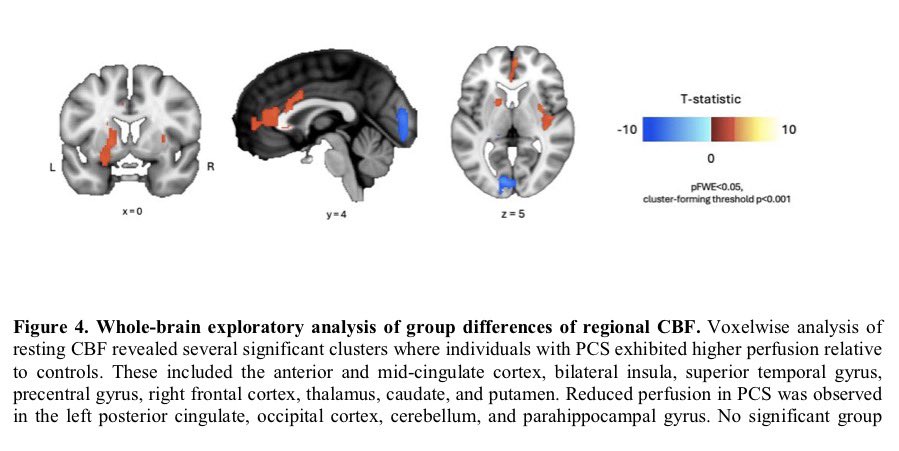
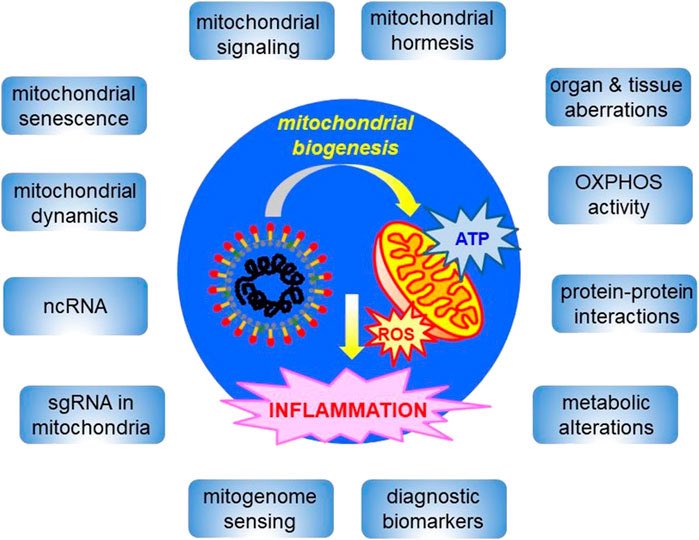
➡️ New review highlights that persistent cognitive symptoms in COVID survivors are strongly linked to pro-inflammatory cytokines and blood–brain barrier (BBB) dysfunction.
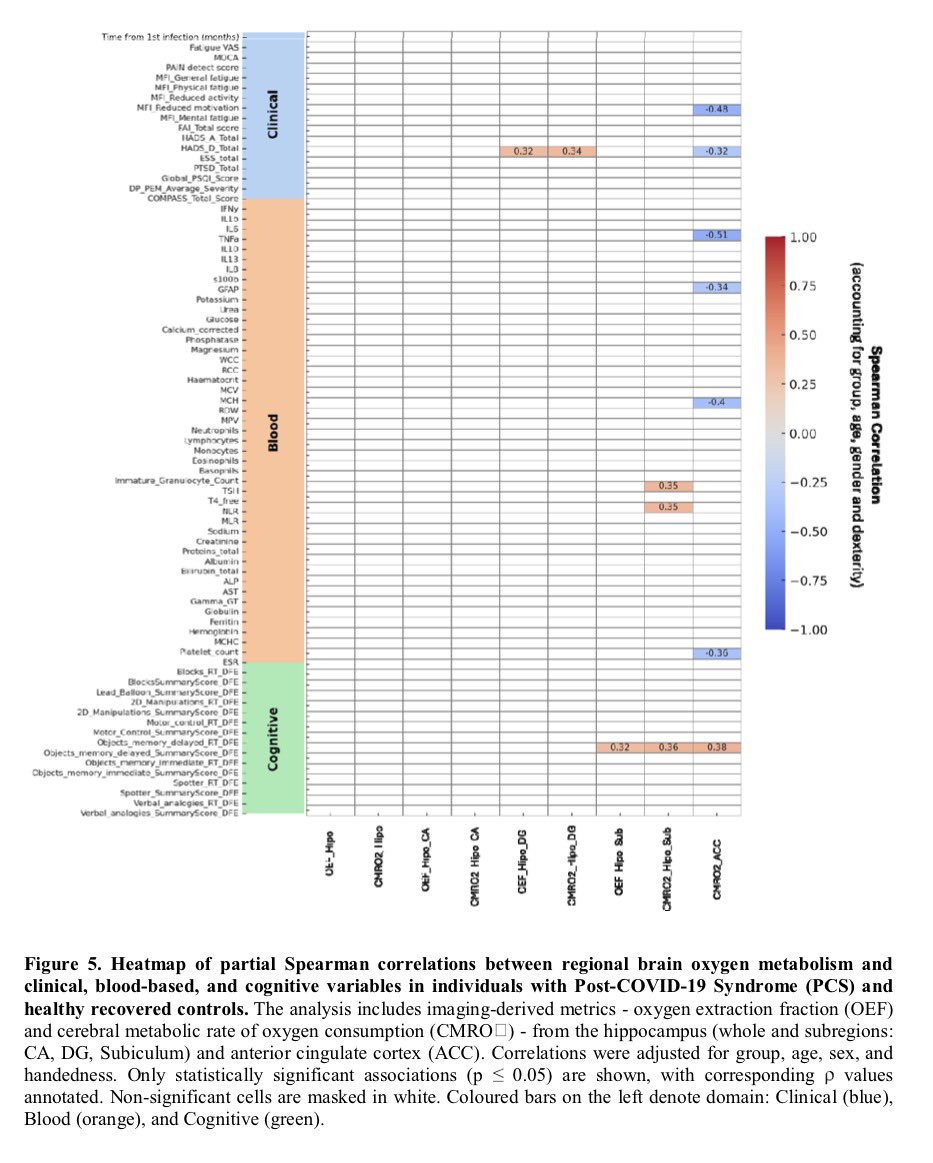
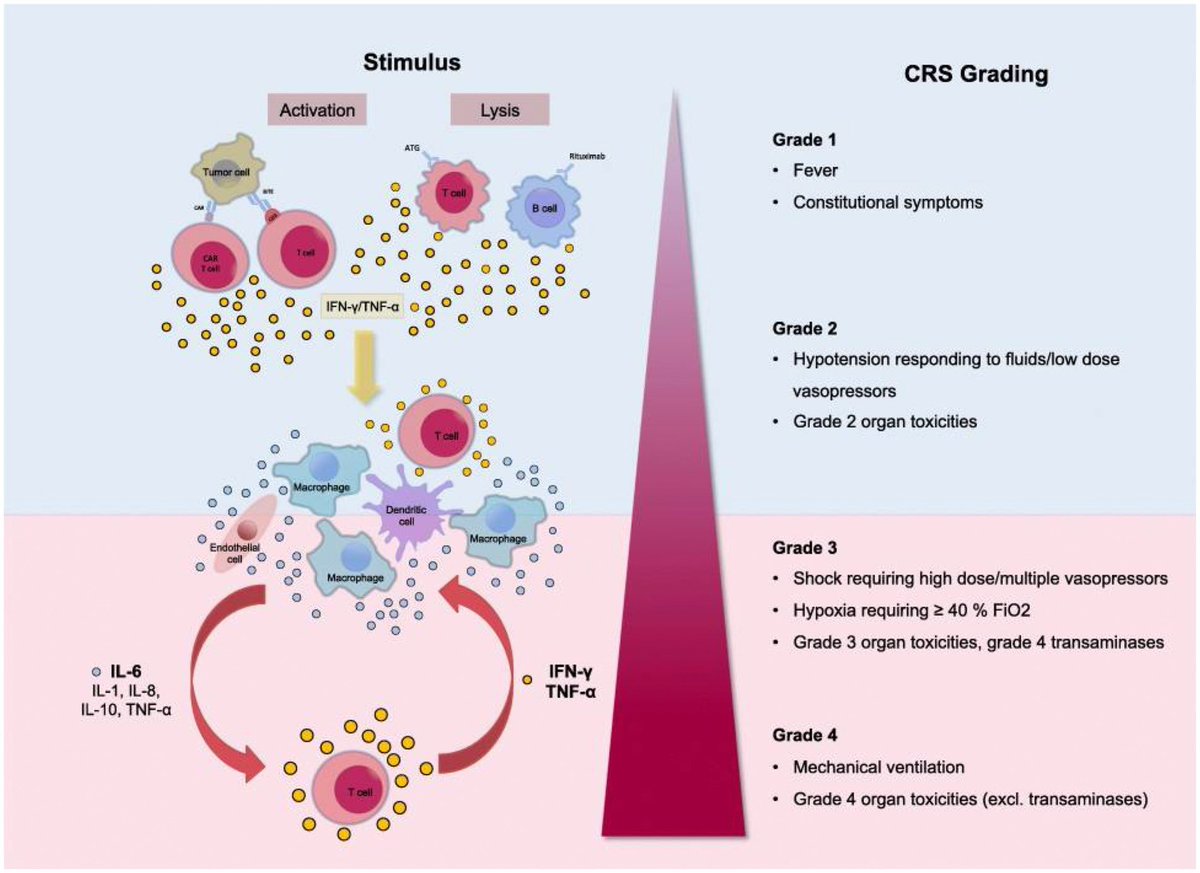
➡️ Key culprits include IL-6, TNF-α, IL-1β, IL-8, IL-13 and MCP-1 — many remain elevated months after infection.
🔥 COVID-19 is not just a respiratory disease.
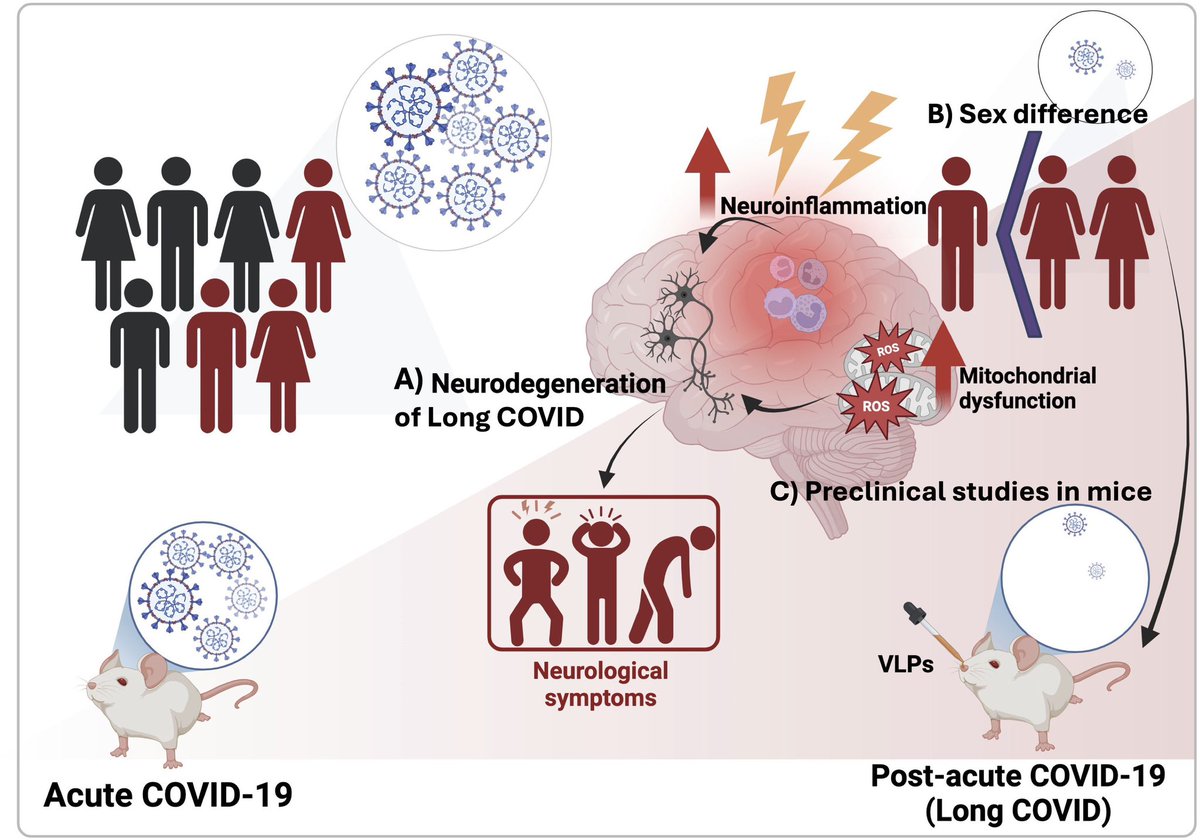
➡️ Evidence suggests cognitive impairment can occur due to:
• Systemic inflammation
• Neuroinflammation
• Microvascular injury
• Persistent immune activation
• BBB disruption
➡️ These mechanisms may explain prolonged attention, memory & executive dysfunction. 1/
➡️ New review highlights that persistent cognitive symptoms in COVID survivors are strongly linked to pro-inflammatory cytokines and blood–brain barrier (BBB) dysfunction.
➡️ Key culprits include IL-6, TNF-α, IL-1β, IL-8, IL-13 and MCP-1 — many remain elevated months after infection.
🔥 COVID-19 is not just a respiratory disease.
➡️ Evidence suggests cognitive impairment can occur due to:
• Systemic inflammation
• Neuroinflammation
• Microvascular injury
• Persistent immune activation
• BBB disruption
➡️ These mechanisms may explain prolonged attention, memory & executive dysfunction. 1/
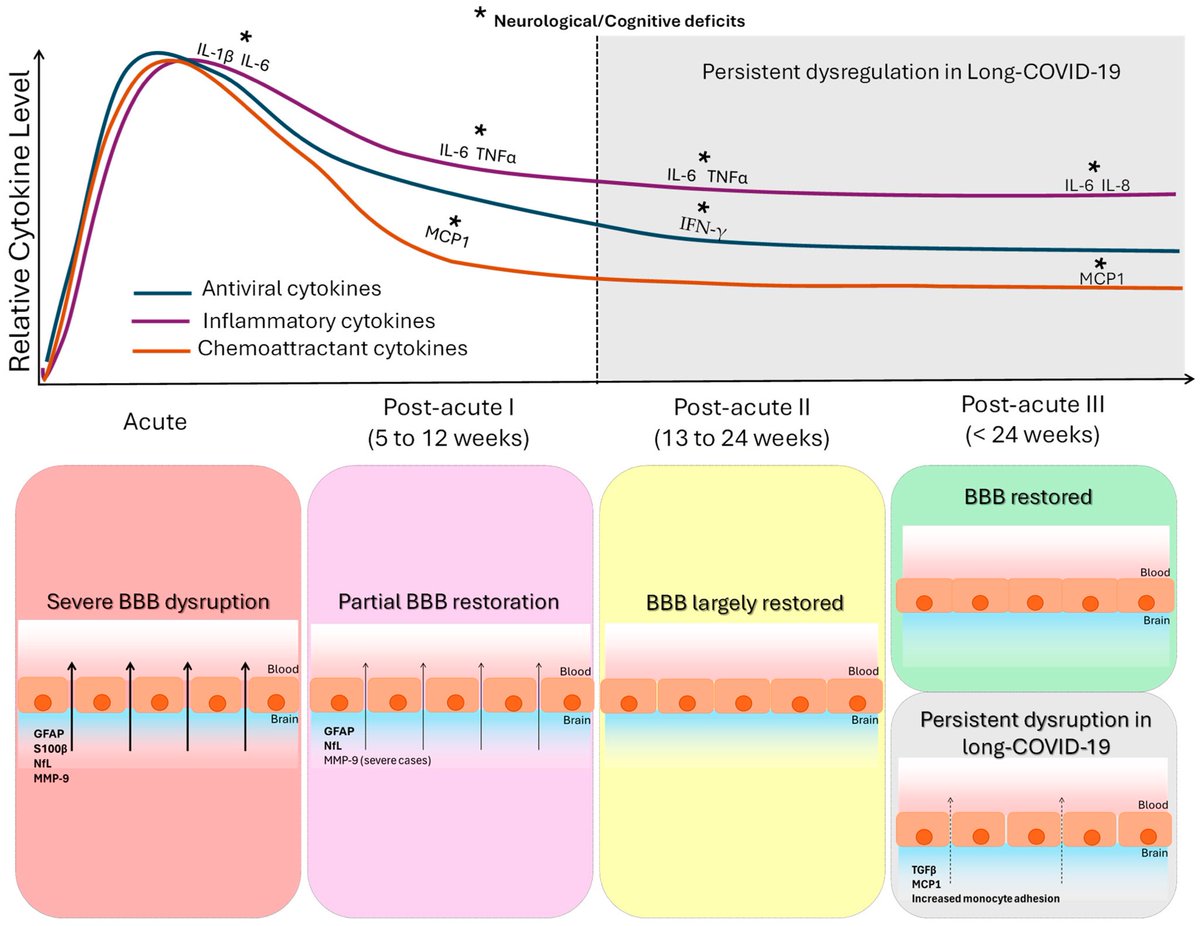
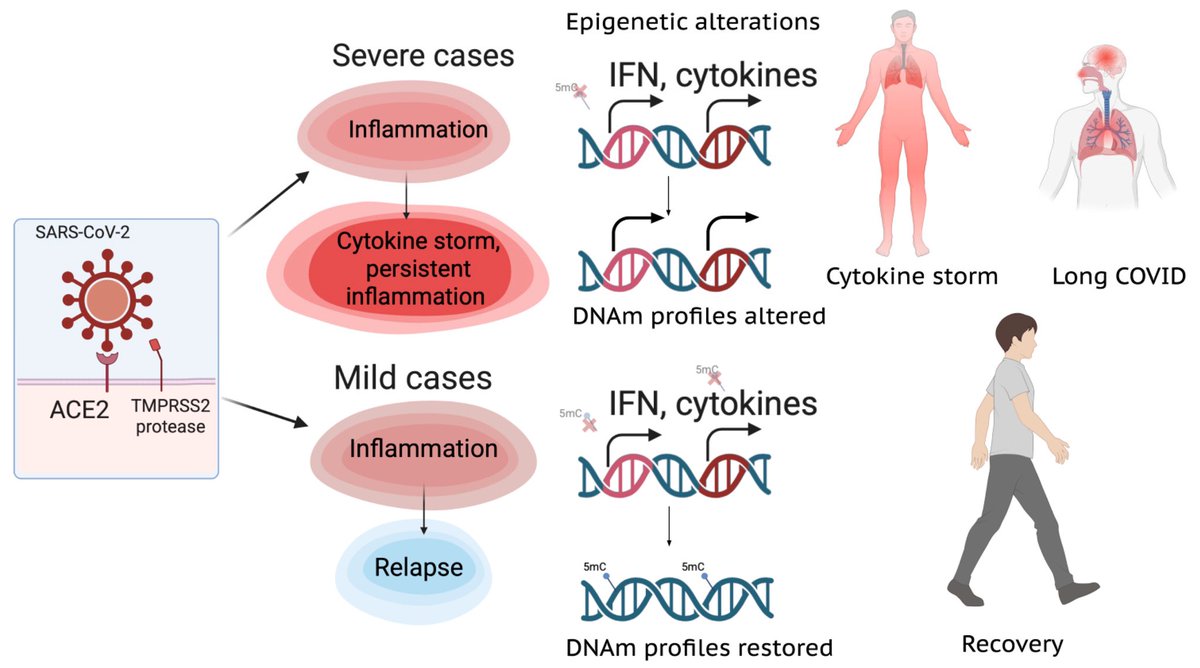
Cytokine signature of cognitive impairment in #LongCOVID:
🔹 Acute phase → IL-6, IL-1β, CXCL10 rise
🔹 Post-acute → Persistent IL-6, TNF-α, MCP-1
🔹 Long phase (>6 months) → IL-6, IL-13, IL-8 linked with “brain fog”
Inflammation clearly outlives the infection.
➡️ Blood–brain barrier disruption appears central in post-COVID cognitive decline.
Markers suggesting BBB injury:
• GFAP
• Neurofilament light chain
• MMP-9
• S100β
➡️ BBB leakage may persist in patients with cognitive symptoms even >1 year. 2/
🔹 Acute phase → IL-6, IL-1β, CXCL10 rise
🔹 Post-acute → Persistent IL-6, TNF-α, MCP-1
🔹 Long phase (>6 months) → IL-6, IL-13, IL-8 linked with “brain fog”
Inflammation clearly outlives the infection.
➡️ Blood–brain barrier disruption appears central in post-COVID cognitive decline.
Markers suggesting BBB injury:
• GFAP
• Neurofilament light chain
• MMP-9
• S100β
➡️ BBB leakage may persist in patients with cognitive symptoms even >1 year. 2/
Blood–brain barrier disruption appears central in post-COVID cognitive decline.
➡️ Markers suggesting BBB injury:
• GFAP
• Neurofilament light chain
• MMP-9
• S100β
➡️ BBB leakage may persist in patients with cognitive symptoms even >1 year.
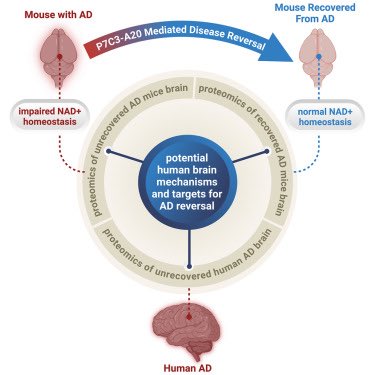
Post-COVID cognitive deficits often affect:
✔ Attention
✔ Working memory
✔ Executive function
✔ Processing speed
➡️ Deficits may start as inflammatory-driven dysfunction but can evolve into persistent neuronal/glial injury.
Early cognitive rehabilitation may be crucial. 3/
➡️ Markers suggesting BBB injury:
• GFAP
• Neurofilament light chain
• MMP-9
• S100β
➡️ BBB leakage may persist in patients with cognitive symptoms even >1 year.
Post-COVID cognitive deficits often affect:
✔ Attention
✔ Working memory
✔ Executive function
✔ Processing speed
➡️ Deficits may start as inflammatory-driven dysfunction but can evolve into persistent neuronal/glial injury.
Early cognitive rehabilitation may be crucial. 3/
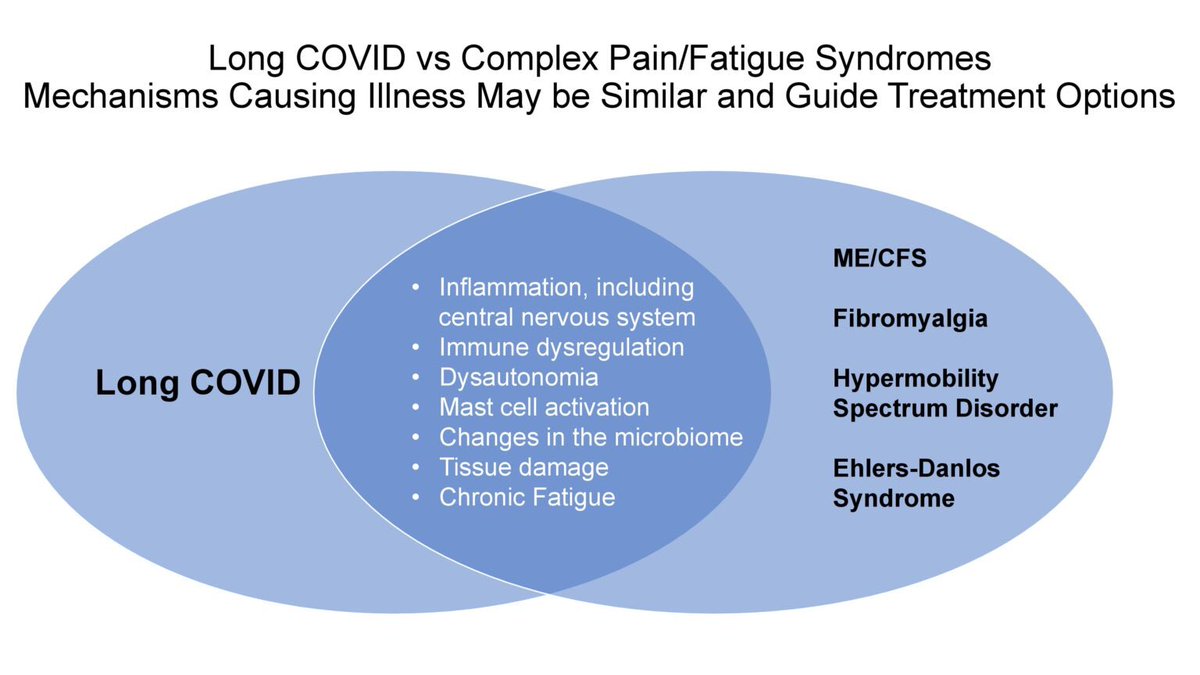
Important clinical takeaway:
➡️ #LongCOVID cognitive symptoms are multifactorial — involving biological injury, systemic illness, and psychosocial factors.
➡️ Management requires:
• Objective cognitive testing
• Mental health screening
• Long-term rehabilitation strategies. 5/5
mdpi.com/1422-0067/27/1…
➡️ #LongCOVID cognitive symptoms are multifactorial — involving biological injury, systemic illness, and psychosocial factors.
➡️ Management requires:
• Objective cognitive testing
• Mental health screening
• Long-term rehabilitation strategies. 5/5
mdpi.com/1422-0067/27/1…
• • •
Missing some Tweet in this thread? You can try to
force a refresh