Tips & tricks for axillary/subclavian central line
1. Start at midclavicular line -> the deltopectoral groove.
2. Collapsible, thin-walled
3. Continuous Doppler flow!
4. Presence of valves denotes a venous structure
5. BONUS inject fluid via ipsilateral peripheral IV!
1. Start at midclavicular line -> the deltopectoral groove.
2. Collapsible, thin-walled
3. Continuous Doppler flow!
4. Presence of valves denotes a venous structure
5. BONUS inject fluid via ipsilateral peripheral IV!
Longitudinal view note the alignment of the rib underneath to utilize the PART method
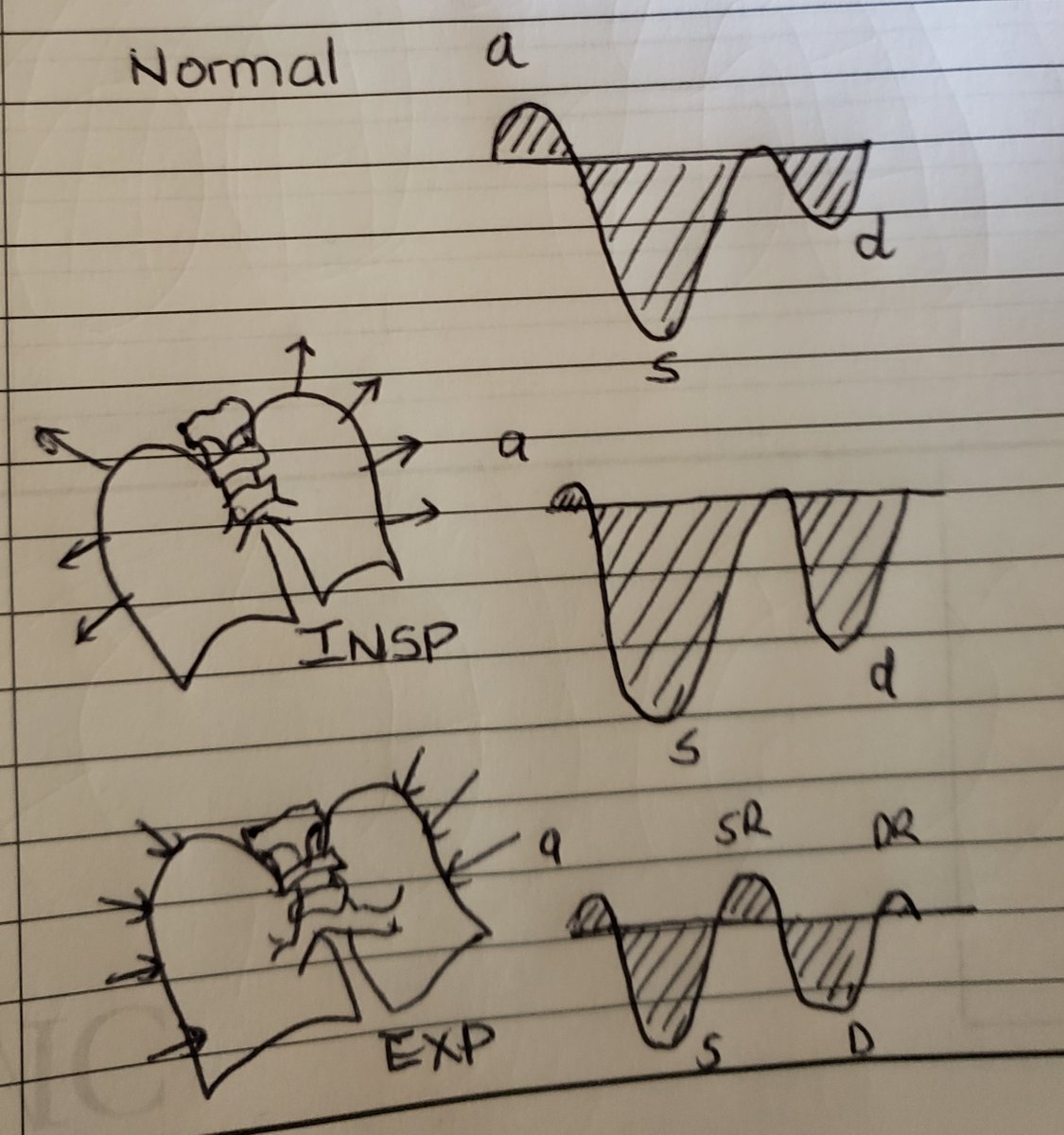
Continuous flow upon Doppler interrogation
Pulsatile flow when tilting cephalad. Big no no
Bonus: try flushing an ipsilateral peripheral IV to confirm
@iceman_ex @MasriAhmadMD @ThinkingCC @UTS_Australia @PulmCrit @ultrasoundpod @UltrasoundJelly @AIUMultrasound @EM_RESUS
Extra Bonus: By using color Doppler you can augment flow by squeezing the bicep to also confirm you are looking at the vein. With a combination of any of the above mentioned texhniques... This should be a cinch.
• • •
Missing some Tweet in this thread? You can try to
force a refresh