
India's Best Academic Group in Internal Medicine.Over 9000 K physicians , 12 WhatsApp groups,live interaction,and case based. Editor-in-chief:Dr N K Singh
How to get URL link on X (Twitter) App

 Keypoints
Keypoints
 Keypoints
Keypoints
 The T-wave is the repolarizing event on ECG , formed at the end of ST-segment.
The T-wave is the repolarizing event on ECG , formed at the end of ST-segment. 

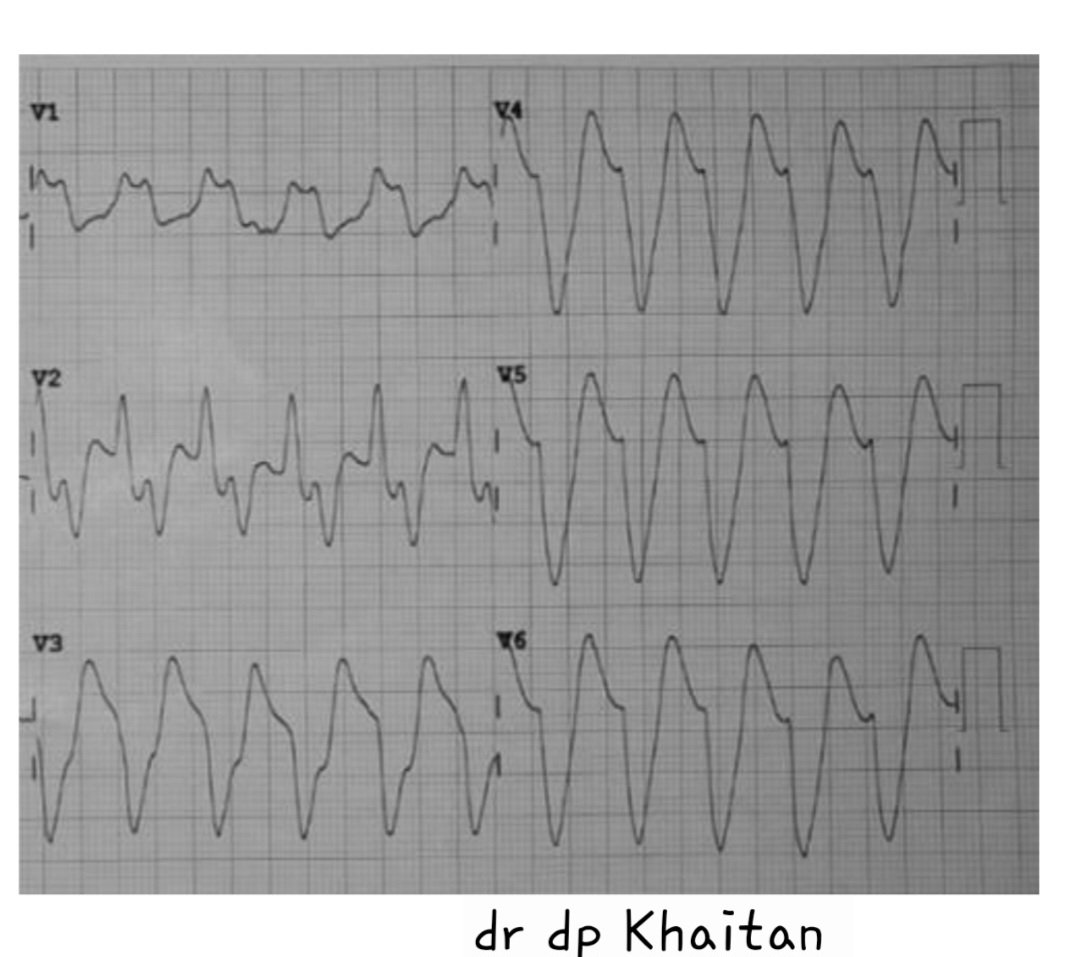
 This ECG 2 shows :
This ECG 2 shows :