Committed to truth in science | Animal-based nutrition for chronic disease | Free lectures online | Consults: https://t.co/k1VIoIR7Nm | Tweets ≠ medical advice
8 subscribers
How to get URL link on X (Twitter) App

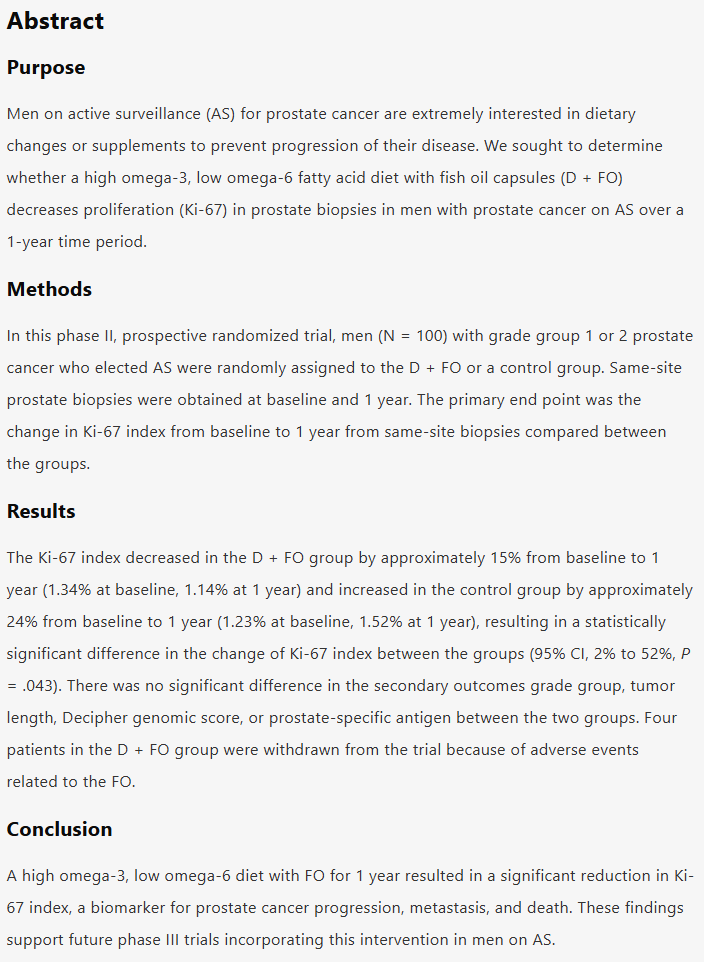
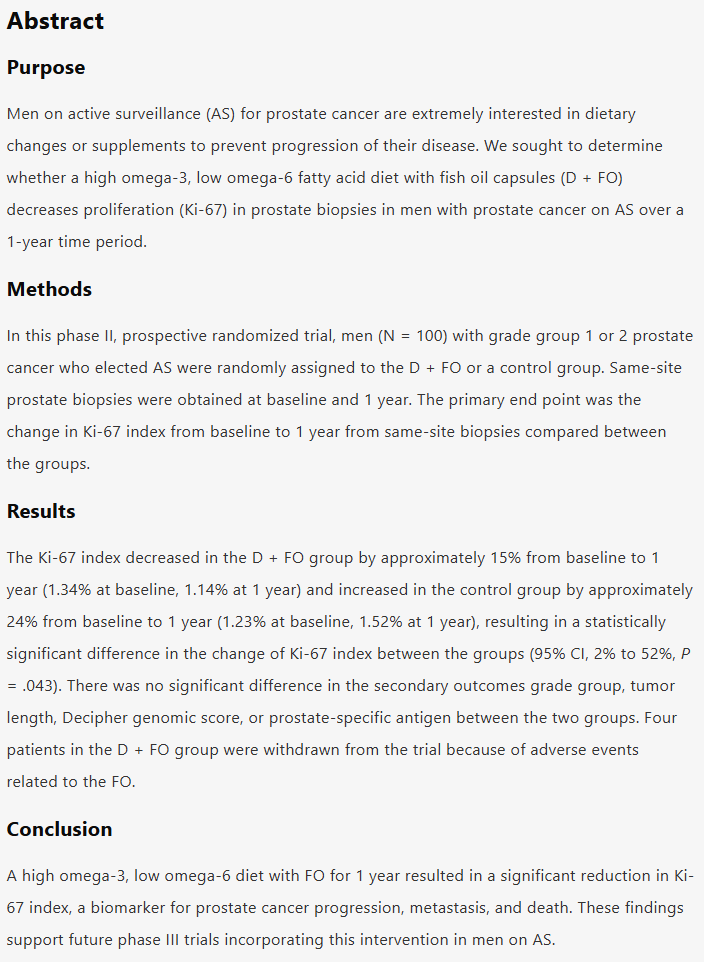 This was a prospective randomised observational study - gold standard for epidemiology.
This was a prospective randomised observational study - gold standard for epidemiology. 
https://twitter.com/Mangan150/status/999056736337051648
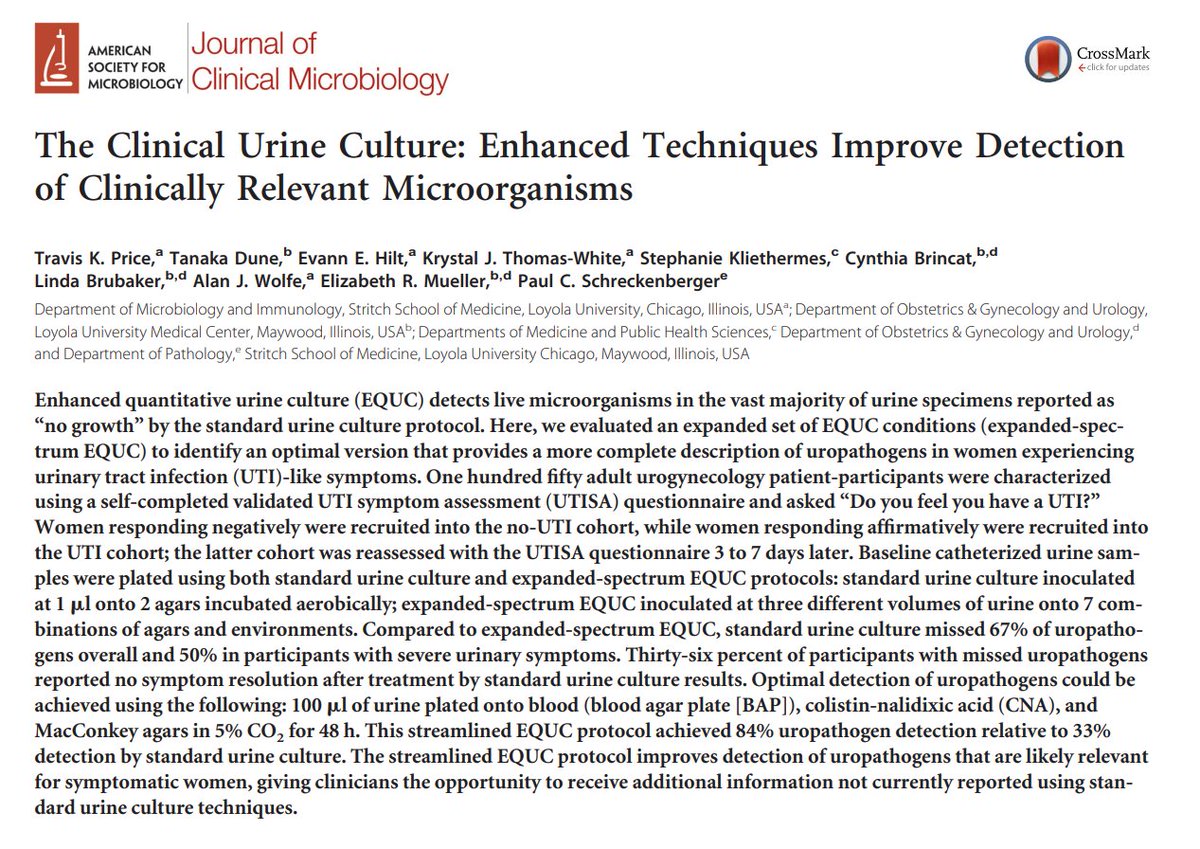
 2/5 - Given I am seeing more and more patients with symptoms of chronic UTIs non responsive to standard antibiotic regimens, it would be good to know which factor is most important - ketones or urea. Specific dietary recommendations could then be provided for either.
2/5 - Given I am seeing more and more patients with symptoms of chronic UTIs non responsive to standard antibiotic regimens, it would be good to know which factor is most important - ketones or urea. Specific dietary recommendations could then be provided for either.
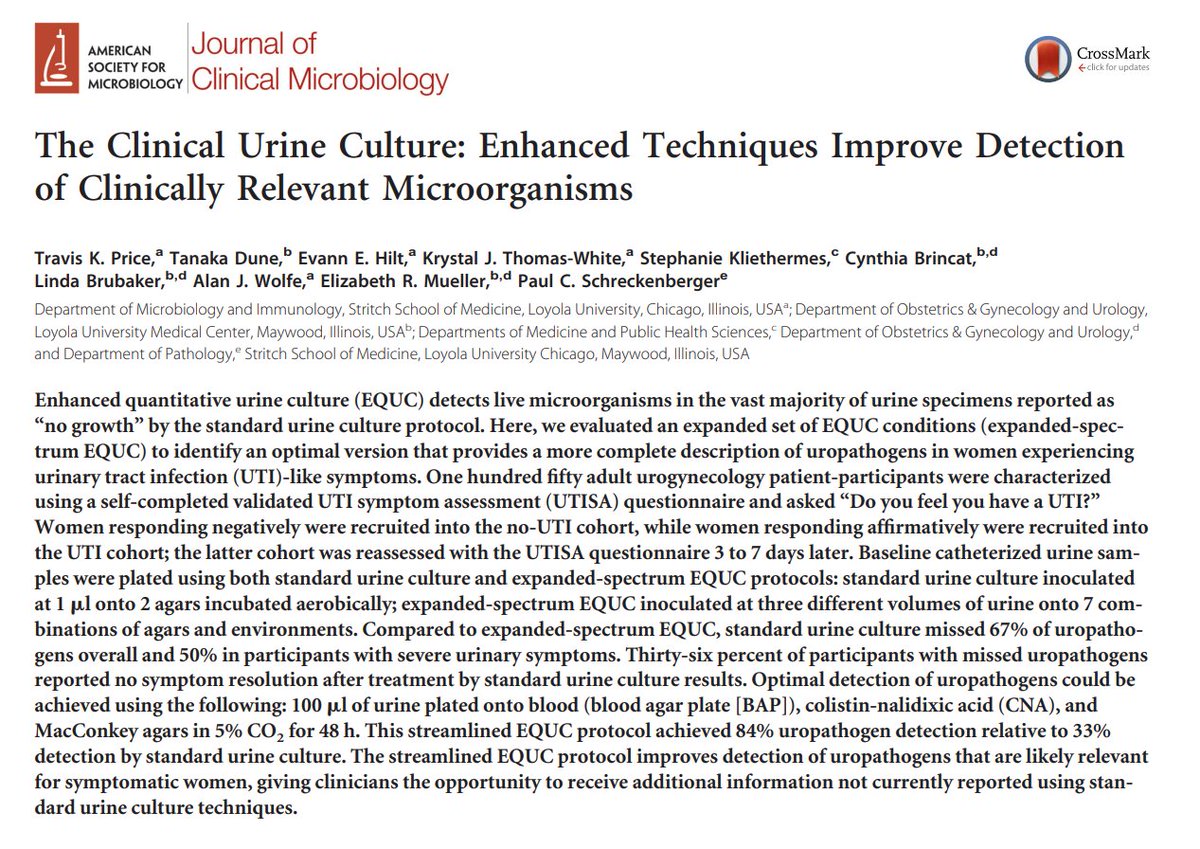
 Furthermore, even identified pathogens are commonly discounted if the bacterial count is <100,000 bugs per millilitre, which might simply happen if you are well hydrated (or the bugs are very effective at clinging to the wall of the bladder - which many are).
Furthermore, even identified pathogens are commonly discounted if the bacterial count is <100,000 bugs per millilitre, which might simply happen if you are well hydrated (or the bugs are very effective at clinging to the wall of the bladder - which many are).
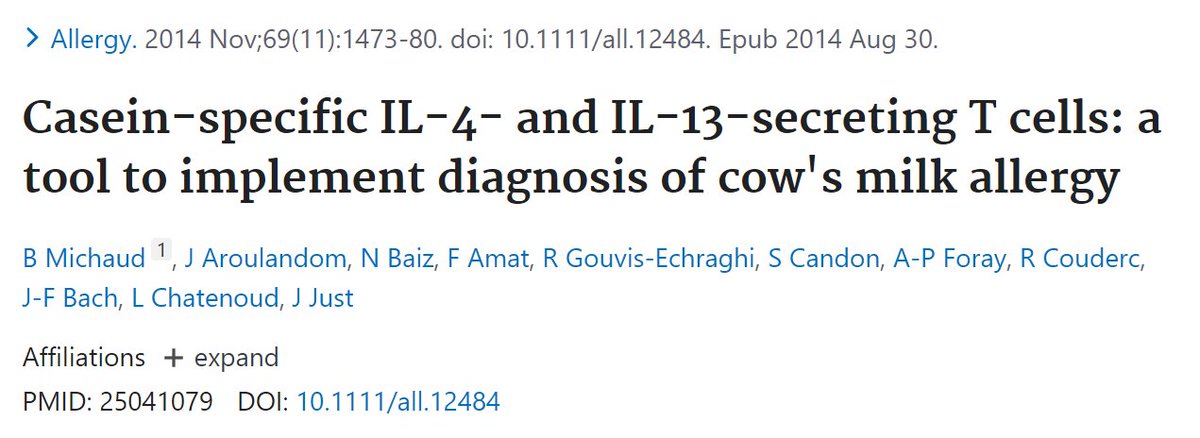
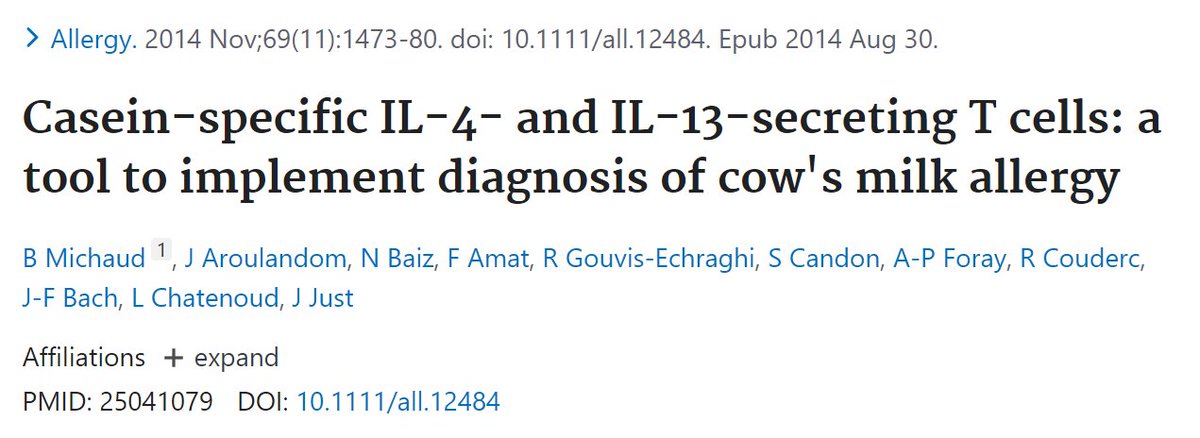
 2/6 -This may be why the meat and dairy consuming Masai have been found to have high rates of RA (if wondering about raw dairy, consider the Masai consume milk from the cow).
2/6 -This may be why the meat and dairy consuming Masai have been found to have high rates of RA (if wondering about raw dairy, consider the Masai consume milk from the cow). 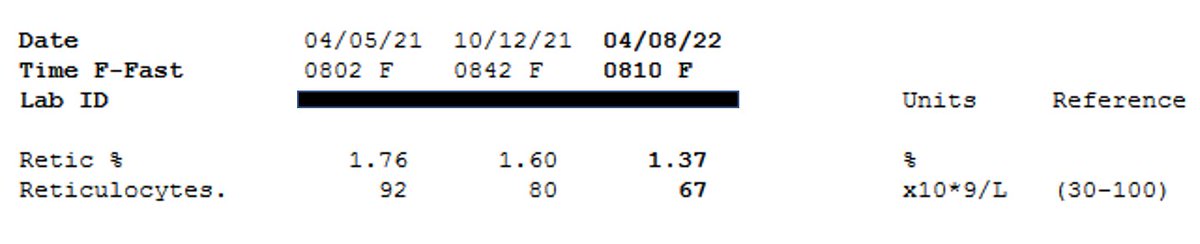
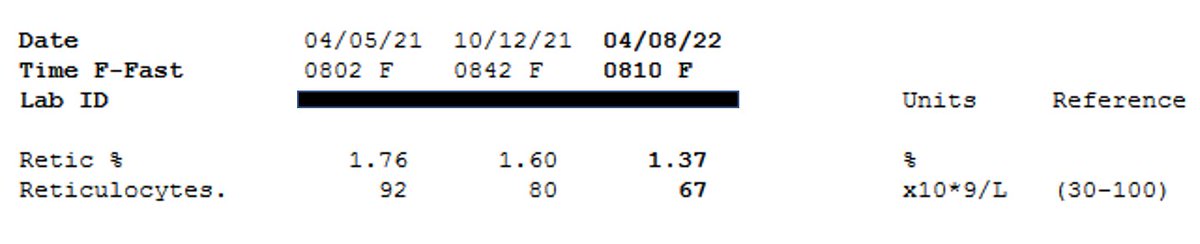 Reticulocytes are 'new' red blood cells. When RBC numbers are stable, few new red blood cells demonstrates a longer lifespan.
Reticulocytes are 'new' red blood cells. When RBC numbers are stable, few new red blood cells demonstrates a longer lifespan. 
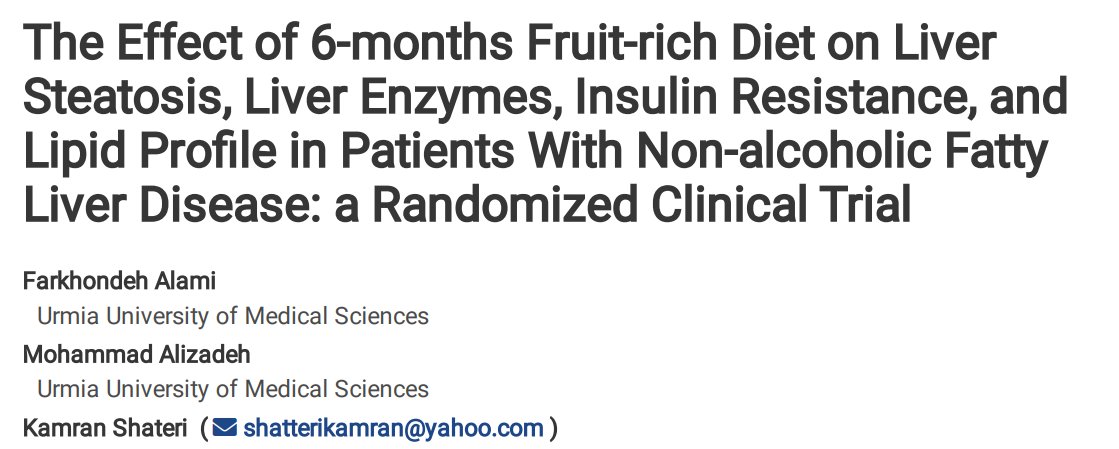
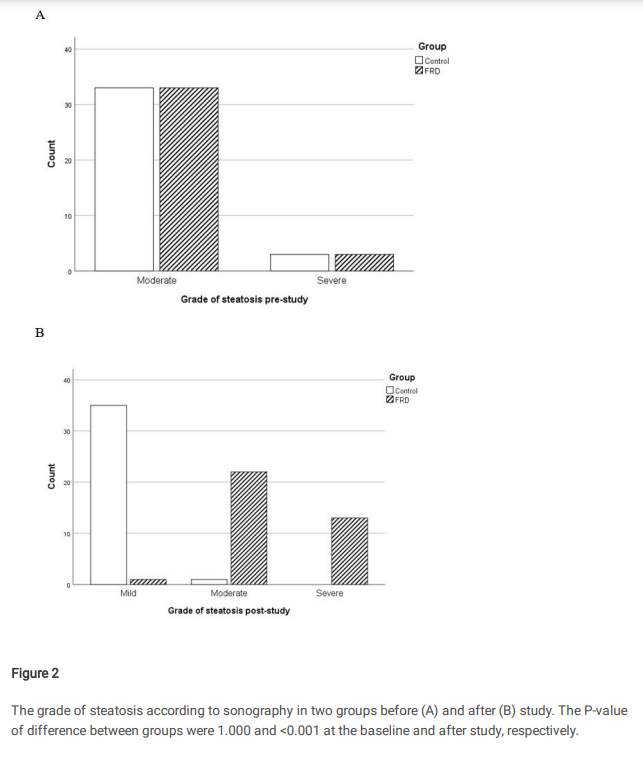
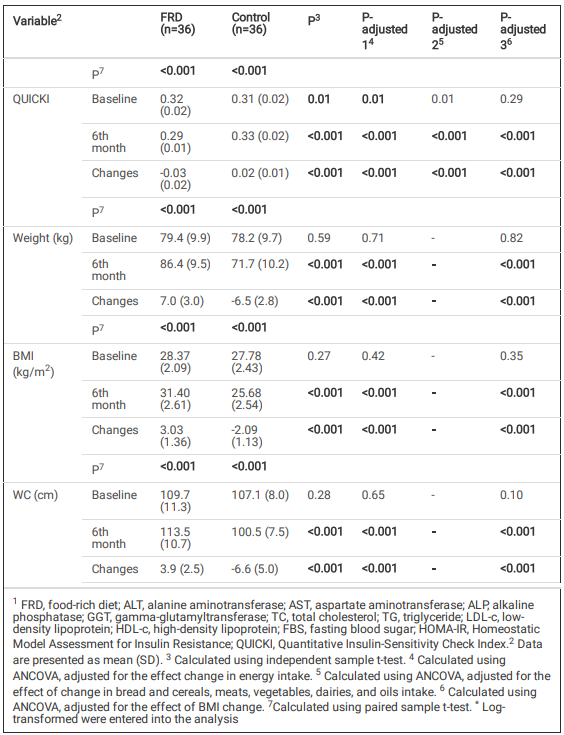 Those on the fruit rich diet gained on average 7.0kg over the 6 month period, while those on the reduced fruit diet lost 6.5kg.
Those on the fruit rich diet gained on average 7.0kg over the 6 month period, while those on the reduced fruit diet lost 6.5kg. 
 A 1976 study with found dialysis patients who died with dementia symptoms had brain aluminium levels 10x's greater than controls.
A 1976 study with found dialysis patients who died with dementia symptoms had brain aluminium levels 10x's greater than controls.


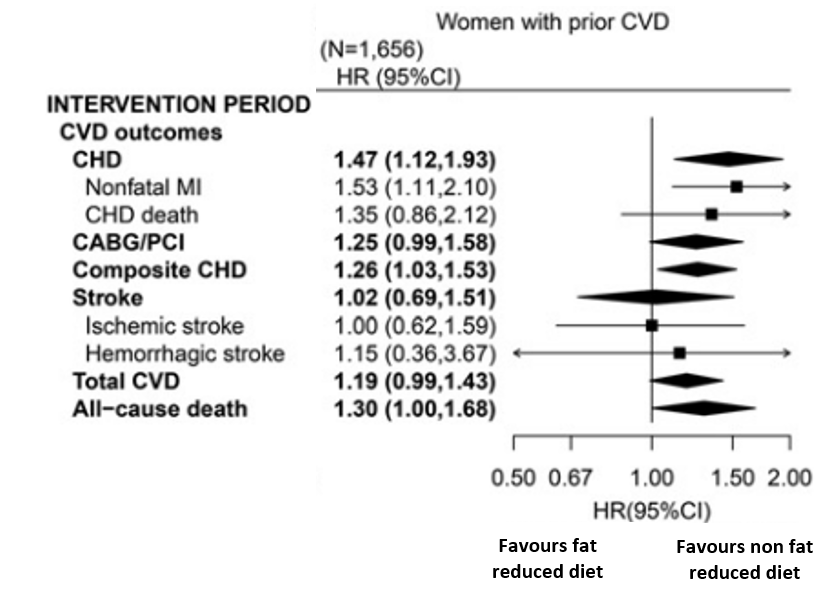
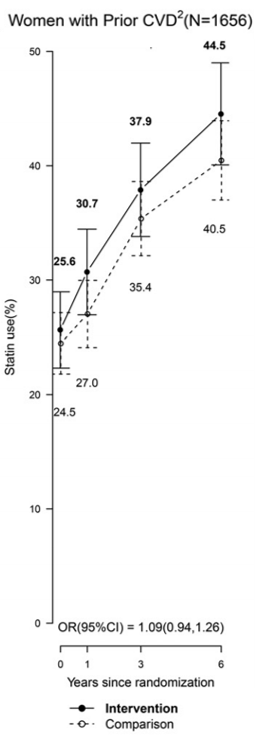
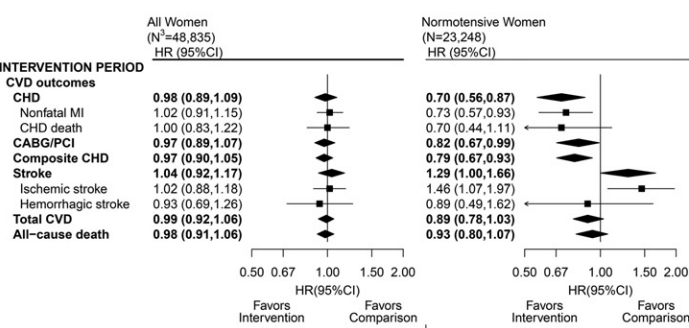
 Those with normal blood pressure had no statistical difference in mortality - they did however record a reduced risk of non fat heart attack on the low fat diet. This was offset by increased risk of stroke, which MAY more adversely impact on quality of life.
Those with normal blood pressure had no statistical difference in mortality - they did however record a reduced risk of non fat heart attack on the low fat diet. This was offset by increased risk of stroke, which MAY more adversely impact on quality of life.