Gastroenterologist & Hepatologist.
Disorders of the Gut Brain Axis.
Treating Long Covid, POTS, MCAS, hEDS.
5 subscribers
How to get URL link on X (Twitter) App

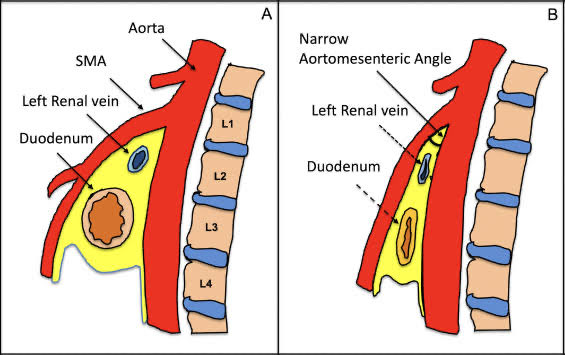
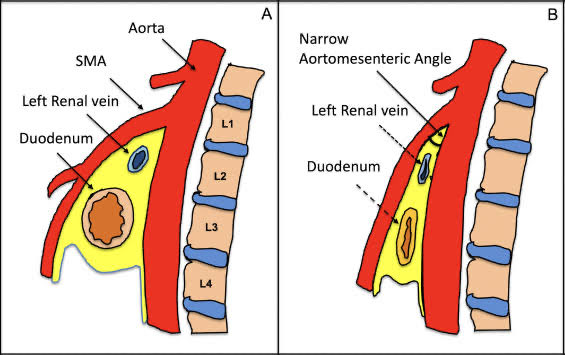 If MALS is thought to be then SMAS is thought to be a unicorn.
If MALS is thought to be then SMAS is thought to be a unicorn. 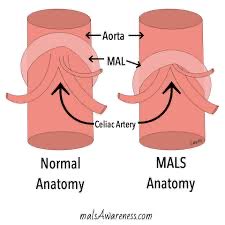
https://twitter.com/valerieanne1970/status/1901871907315560950I have performed over 30,000 colonoscopies