
Ravi Gupta is Professor of Clinical Microbiology, University of Cambridge. TIME100 Most Influential 2020; Clarivate Highly Cited Researcher 2022-24 global lists
6 subscribers
How to get URL link on X (Twitter) App







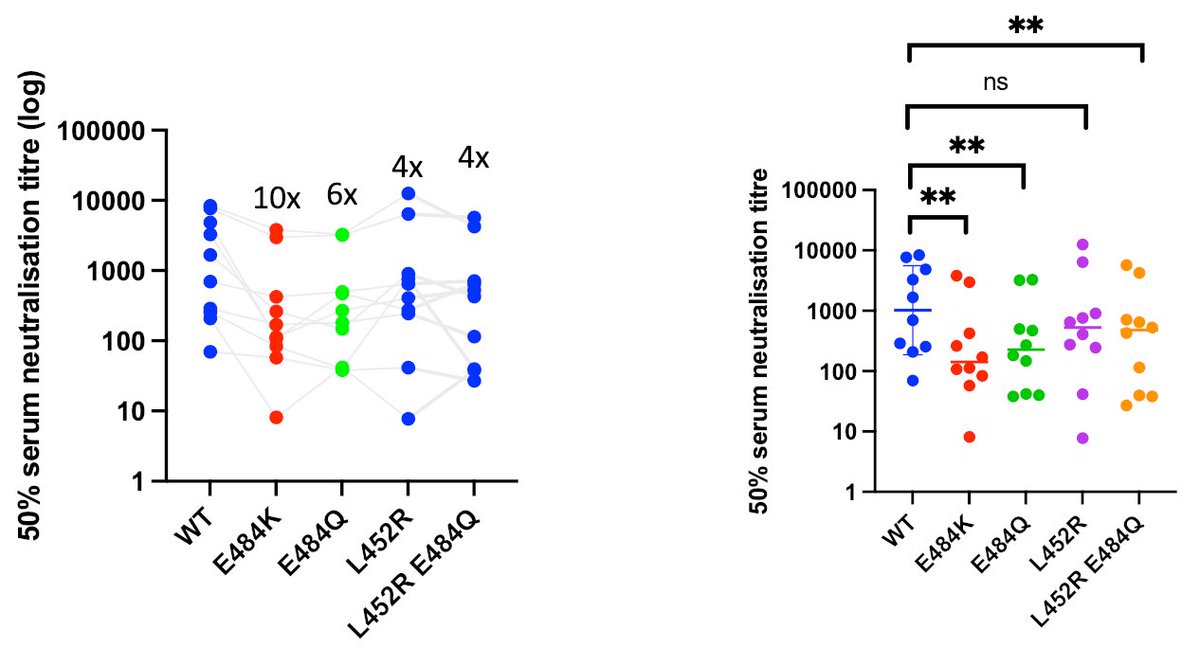
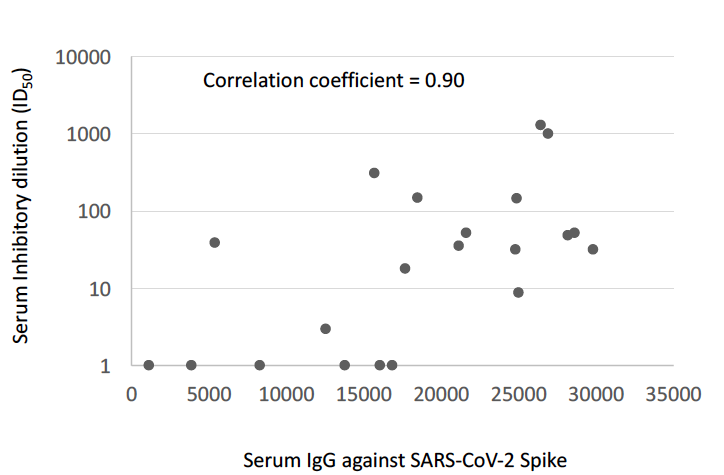
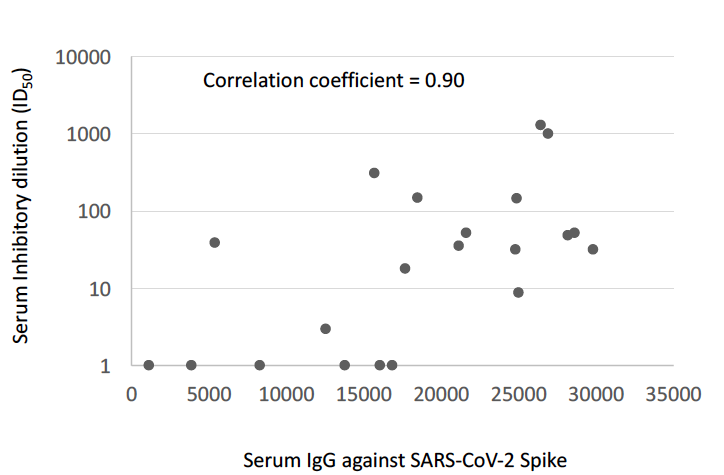
 We first measured baseline SARS-CoV-2 seroprevalence prior to vaccination using flow cytometry methods for binding antibodies to nucleocapsid (N), coupled with virus neutralisation approaches for protective neutralizing antibody responses to VOC (January 2021)
We first measured baseline SARS-CoV-2 seroprevalence prior to vaccination using flow cytometry methods for binding antibodies to nucleocapsid (N), coupled with virus neutralisation approaches for protective neutralizing antibody responses to VOC (January 2021)














https://twitter.com/GuptaR_lab/status/1350131626240598019It could be that >80 yo are slower in mounting responses but this is unlikely and also leaves people vulnerable despite vaccine. Remember >80 y o are not featuring in trials so they might still get severe disease. Pre print to come but significant delays.
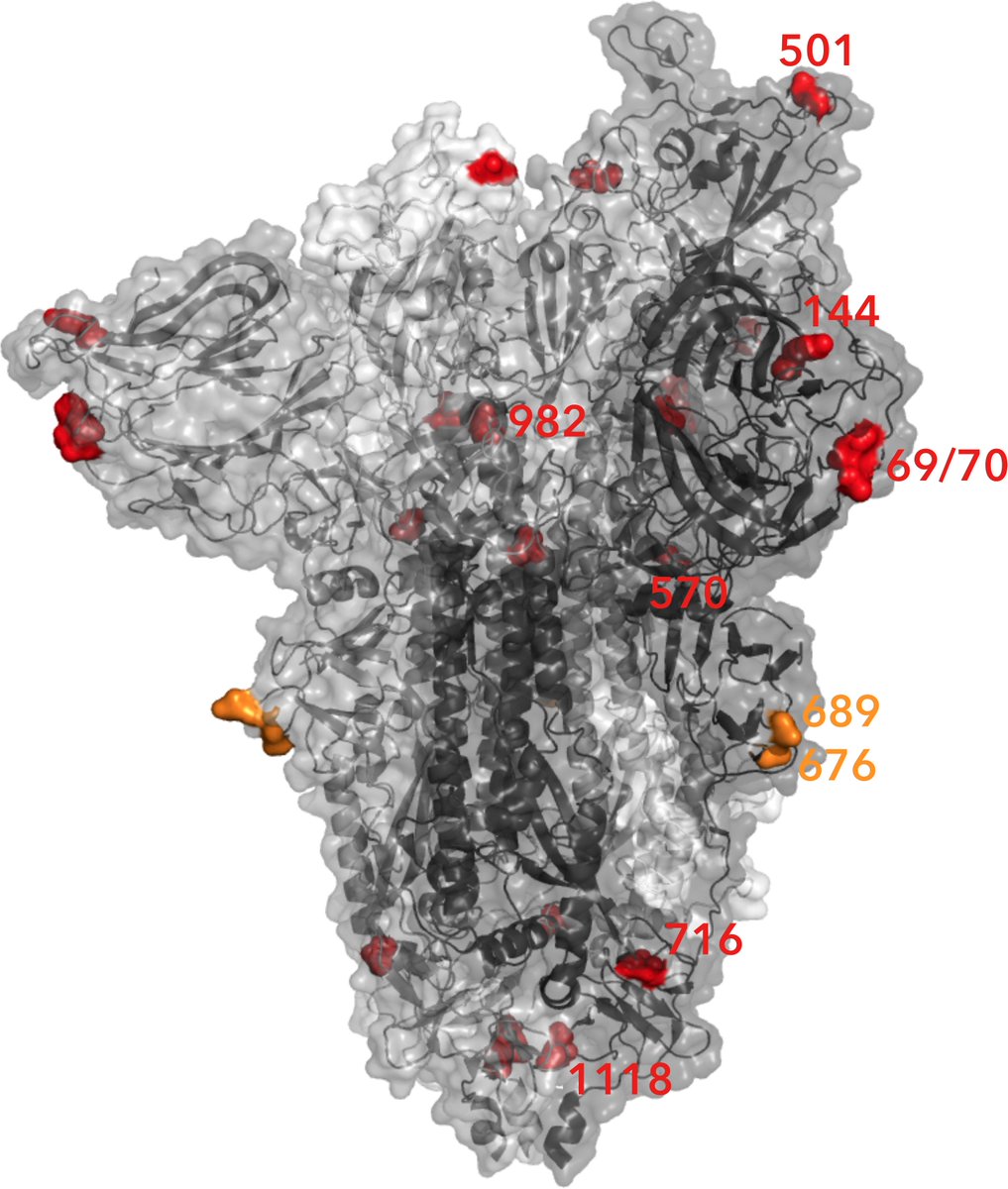
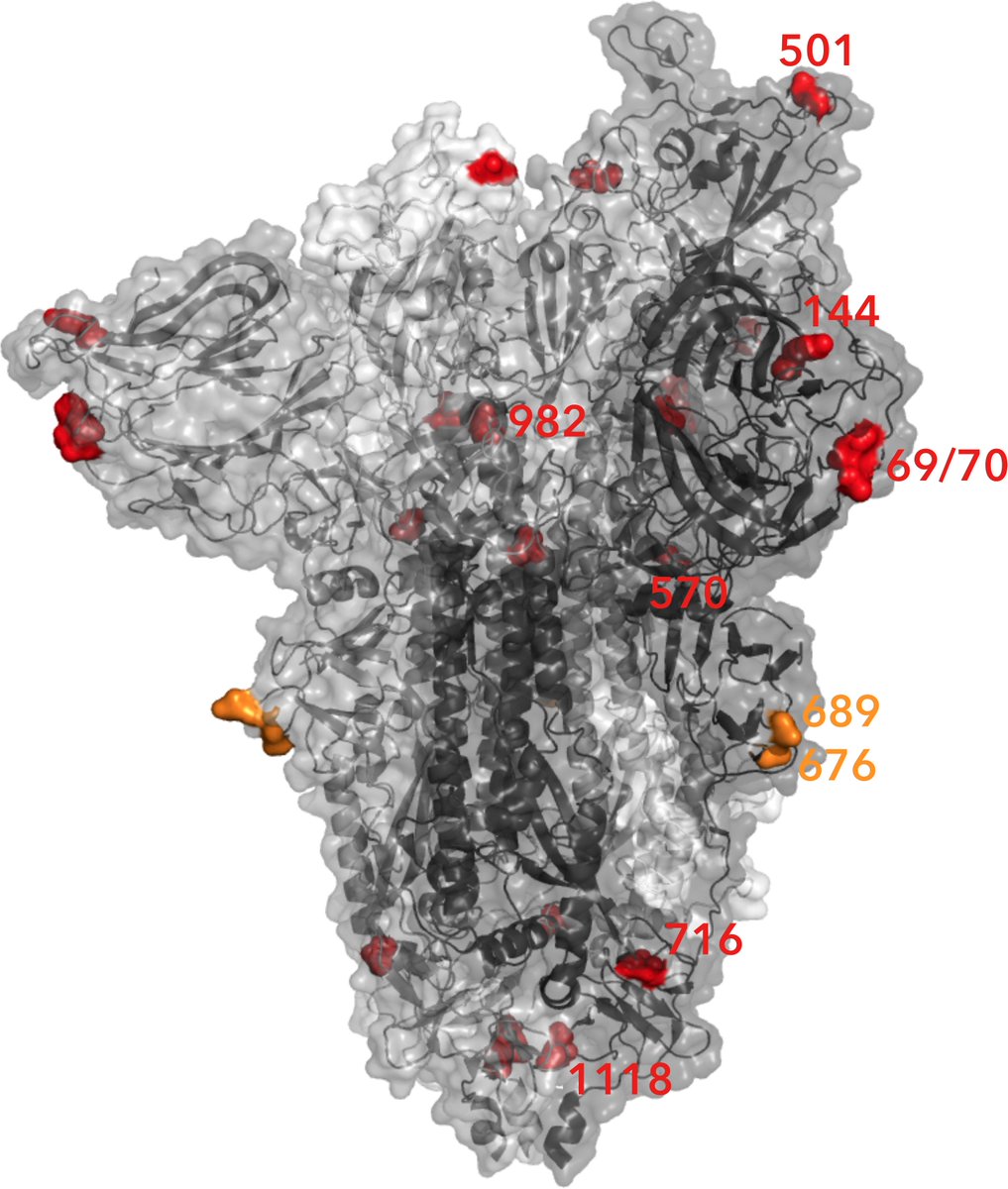 The numbers infected with B1.1.7 has been growing faster than other UK variants based on independent data sources. This variant of SARS-CoV-2 is therefore thought to be more transmissible by around 50%. Data suggest it does not lead to more severe illness however.
The numbers infected with B1.1.7 has been growing faster than other UK variants based on independent data sources. This variant of SARS-CoV-2 is therefore thought to be more transmissible by around 50%. Data suggest it does not lead to more severe illness however.

