
Rheumatologist at Christian Medical College, Vellore | 🎥 YouTube: "Sullys Rounds" | Passionate about travel and research. ✈️🔬@cmcvellore
How to get URL link on X (Twitter) App


 1/9 Why this question matters
1/9 Why this question matters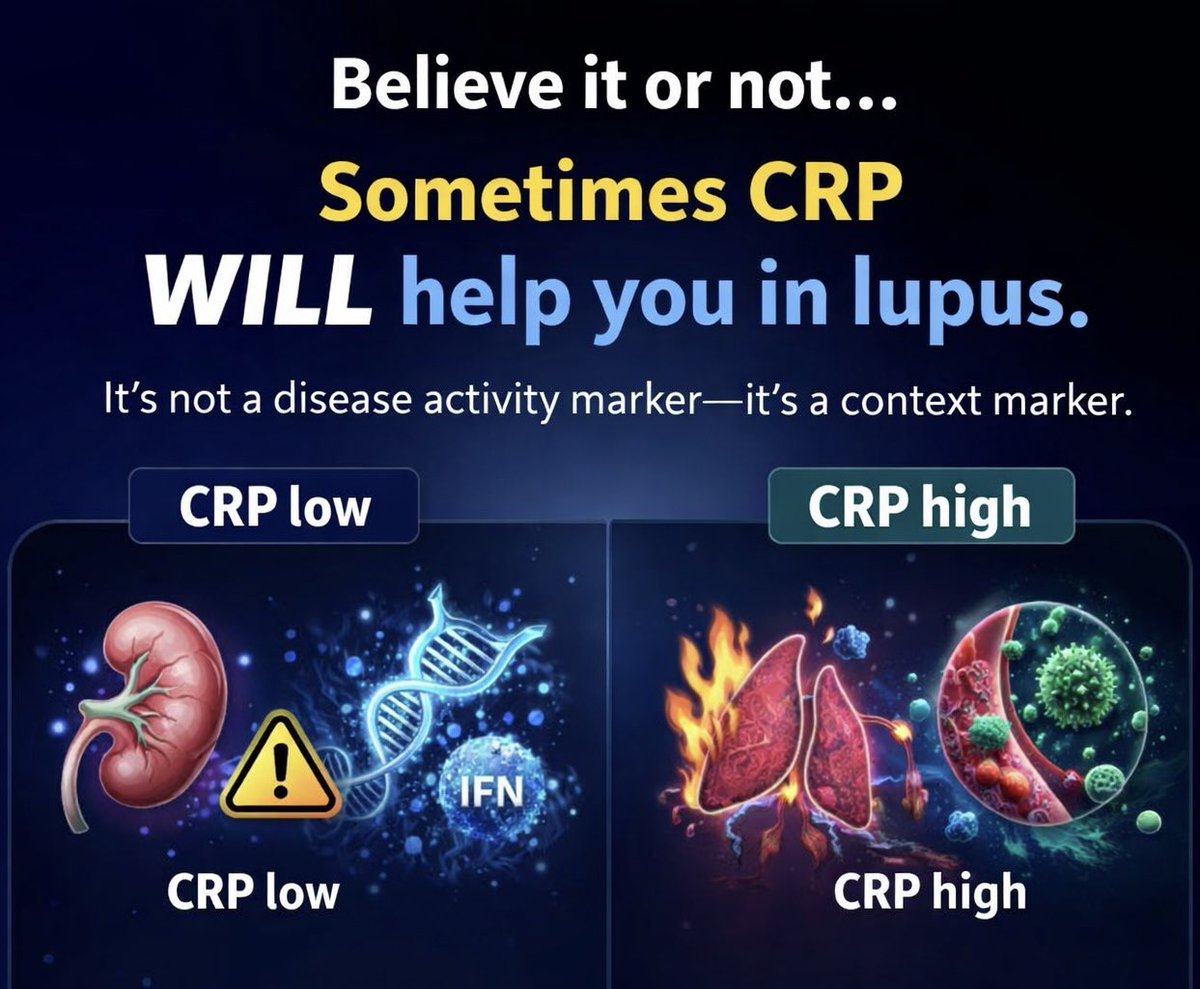
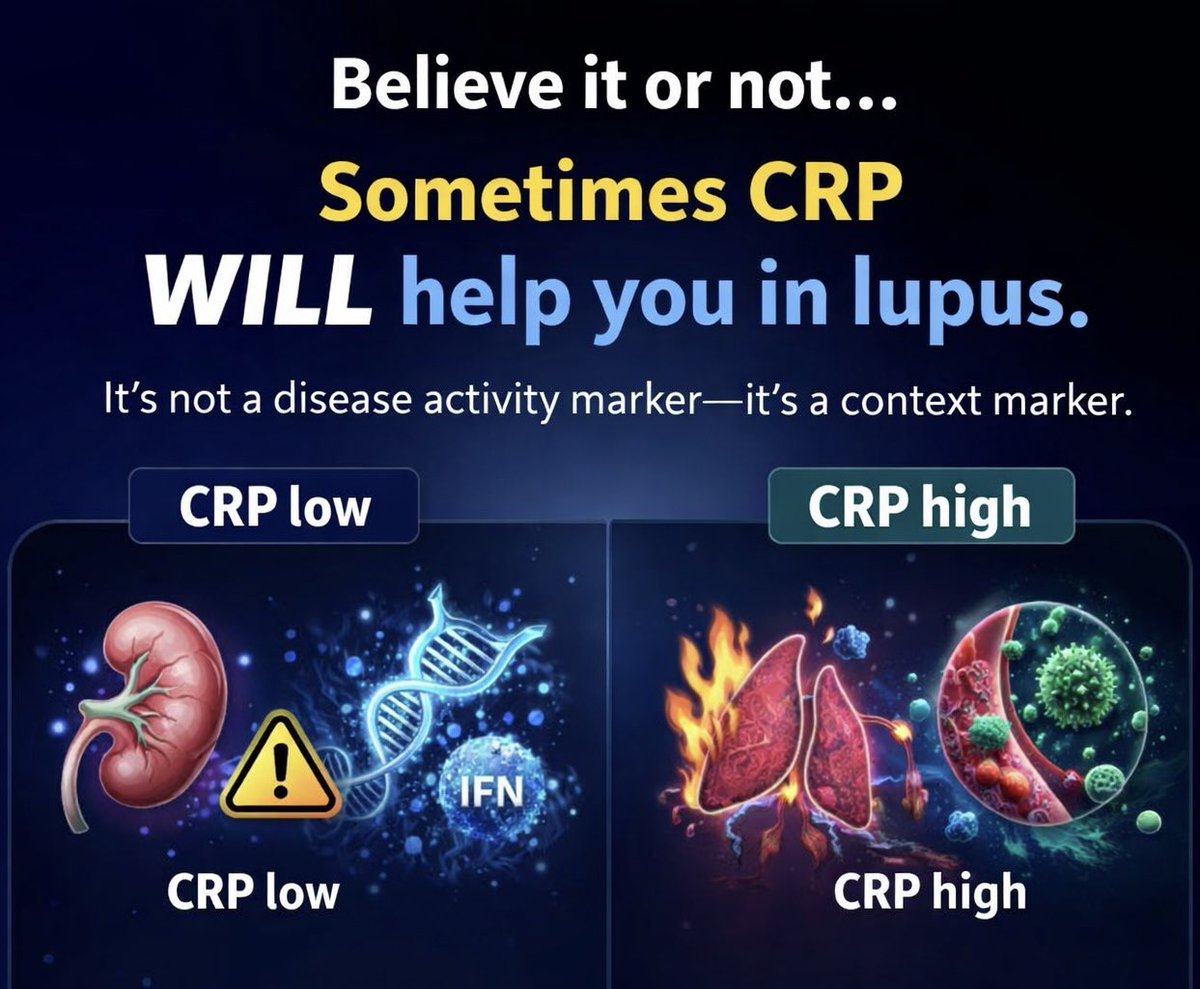 2/6. Lupus is not an IL-6 disease
2/6. Lupus is not an IL-6 disease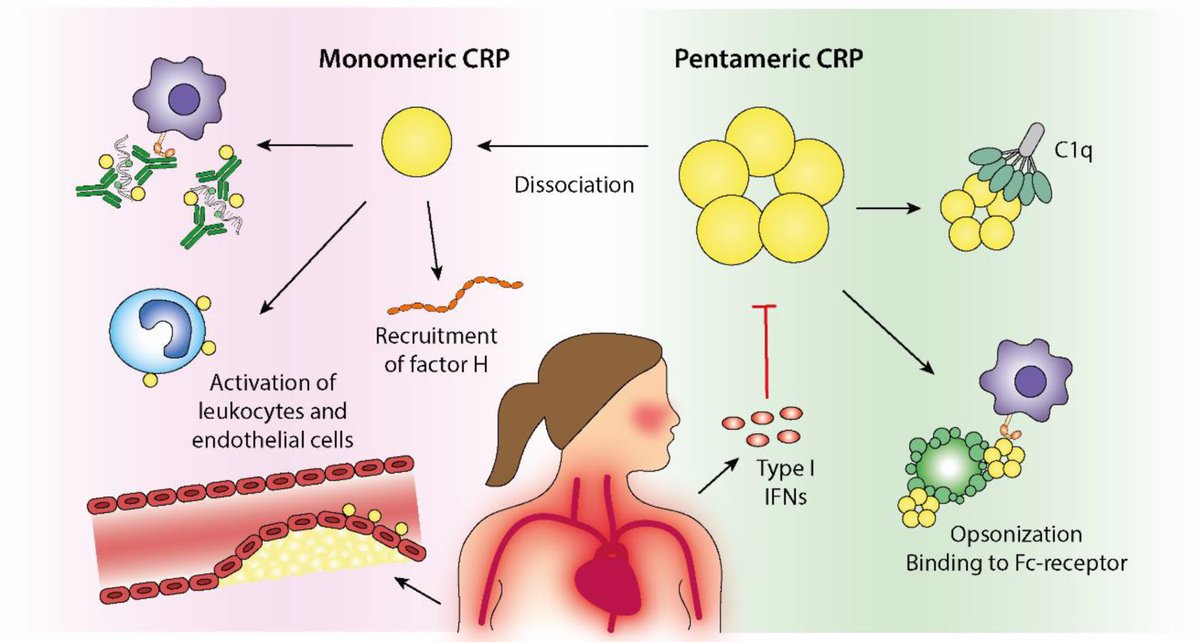

 1/3
1/3 
 1/10
1/10

 🧵 2/7 – STEP 1: Morphology
🧵 2/7 – STEP 1: Morphology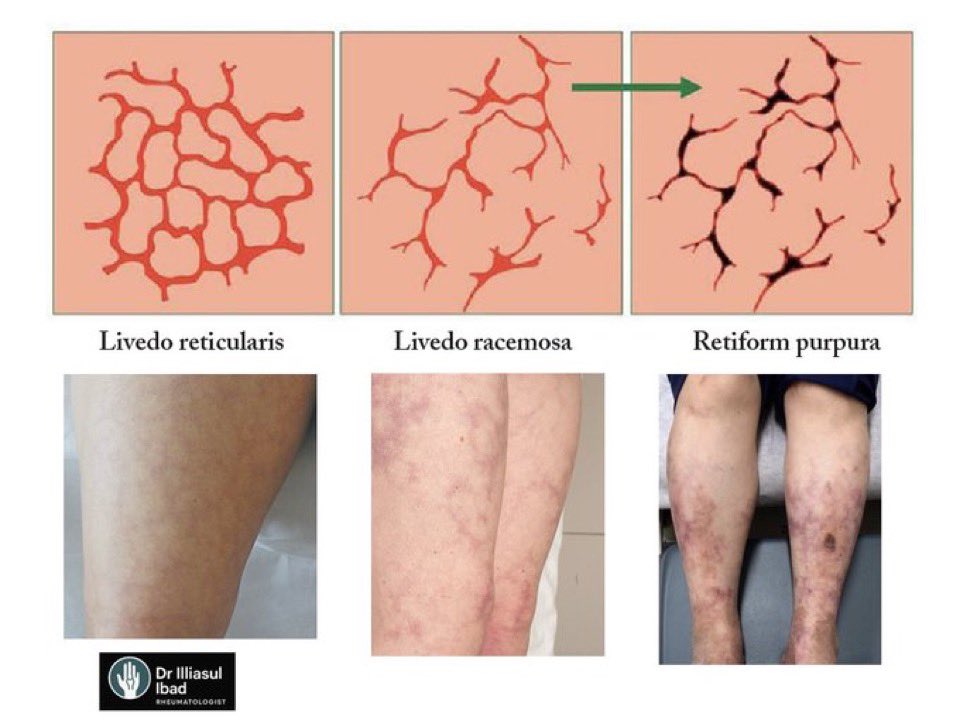

 Tweet 2/6
Tweet 2/6

 Tweet 2/10
Tweet 2/10
 Tweet 2/4
Tweet 2/4
 Tweet 2/5
Tweet 2/5

 Tweet 2/7
Tweet 2/7
 2- Asymptomatic carrier
2- Asymptomatic carrier 

 Tweet 2:
Tweet 2:

 1/
1/

 1/
1/

 2/ Definition of PAH
2/ Definition of PAH 
 2/
2/

 2/
2/

 2/
2/
 Tweet 2:
Tweet 2:

 2/
2/

 But few know about the brilliant scientist who paved the way for its success—Dr. Yellapragada SubbaRow. Let’s uncover his story. 👇
But few know about the brilliant scientist who paved the way for its success—Dr. Yellapragada SubbaRow. Let’s uncover his story. 👇