
Nutrition, metabolism & obesity scientist. Brady & Cameron’s dad. Tweets are my personal views. https://t.co/q8mHqBHeEj
How to get URL link on X (Twitter) App


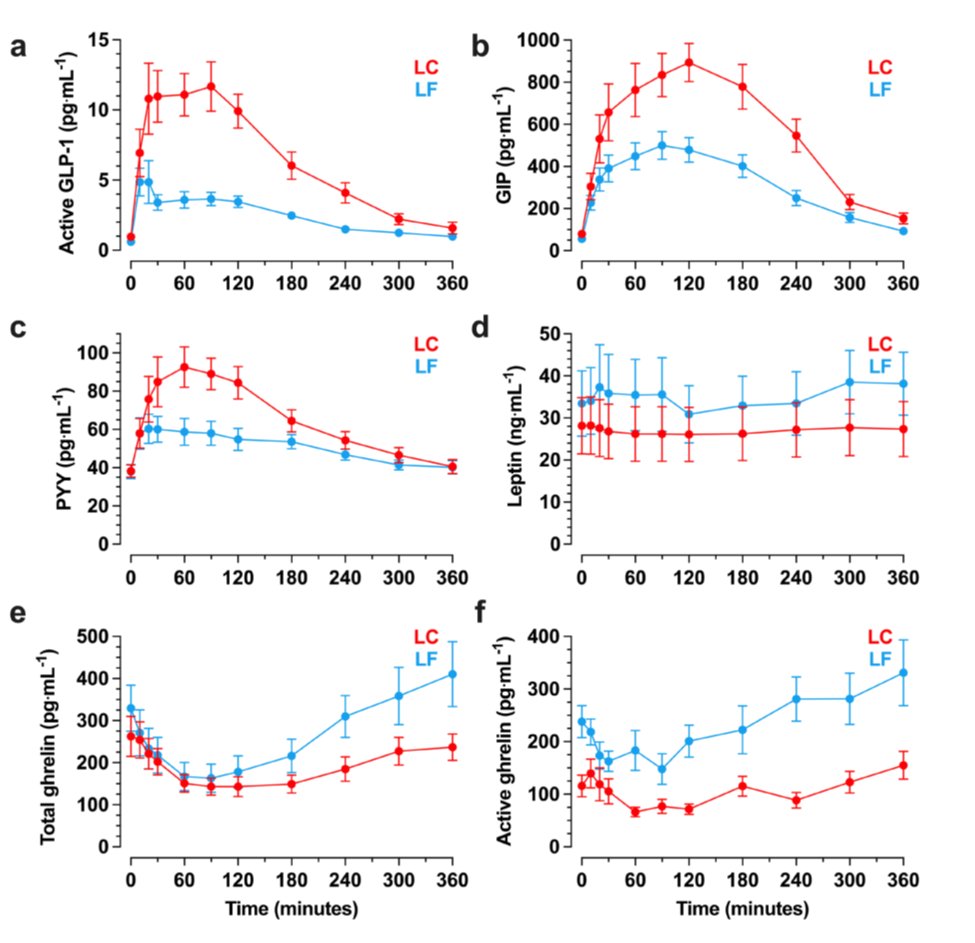
https://twitter.com/kevinh_phd/status/1861059465379819950Study participants were admitted to @NIHClinicalCntr for a month where we exposed them to 4 different food environments with 6000 kcal/d as described below and instructions to eat as much or as little as they wanted.





https://twitter.com/NatMetabolism/status/1668320524546744323Specifically, the authors elegantly showed that people without obesity have statistically significant neural responses to intragastric nutrients. Such responses weren't significant in people with obesity. But this doesn't necessarily imply there were significant group differences
https://twitter.com/jflier/status/1649793787248492546But the EBM does propose an approach to this question: study how changing food environments in specific ways alters ad libitum energy intake in people (or rodents) not trying to change their weight & study how these environmental changes affect neural circuits controlling feeding
https://twitter.com/juliaoftoronto/status/1633786127386550273“Subtyping people with obesity is not reliable,” said Samuel Klein,…“because there is not enough data to identify obesity subtypes and what specific treatment approaches would be most effective for individual subtypes.”







https://twitter.com/davidludwigmd/status/1501601876864733184The push model "explicitly excludes metabolic effects of food that are independent of calories. That is, all calories are considered alike to the body and no macronutrient has any special calorie- independent effect on lipid storage or energy expenditure for practical purposes."

https://twitter.com/davidludwigmd/status/1491038298349146115
 In other words, endocrine regulation of fat metabolism evolved to ensure that whole-body energy & fat imbalances (dictated by the hierarchy of metabolic fuel selection) are targeted mostly in the safest place for their storage (adipose) as opposed to their ectopic accumulation.
In other words, endocrine regulation of fat metabolism evolved to ensure that whole-body energy & fat imbalances (dictated by the hierarchy of metabolic fuel selection) are targeted mostly in the safest place for their storage (adipose) as opposed to their ectopic accumulation.


https://twitter.com/davidludwigmd/status/1488942663852199938
 This study was admittedly a purely exploratory analysis designed to detect *any* post 2-week changes, regardless of whether such changes were meaningful. This analysis was not included in the pre-specified statistical analysis plan for the CGM data: osf.io/m6v73/
This study was admittedly a purely exploratory analysis designed to detect *any* post 2-week changes, regardless of whether such changes were meaningful. This analysis was not included in the pre-specified statistical analysis plan for the CGM data: osf.io/m6v73/

https://twitter.com/AcademicChatter/status/1415713232828854276The logic appears solid: Insulin promotes fat storage & inhibits it's release from adipose tissue. Eating carbs causes insulin to increase after meals. Therefore, "carbohydrate is driving insulin is driving fat" as George Cahill purportedly told @garytaubes in an interview. True!

https://twitter.com/CMonteiro_USP/status/1413674735813251073The first involves calculating energy intake changes resulting from eliminating ultra-processed food. The authors rely on our metabolic ward study in 20 adults and make several unjustified assumptions to extrapolate to free-living children and adolescents pubmed.ncbi.nlm.nih.gov/31105044/