
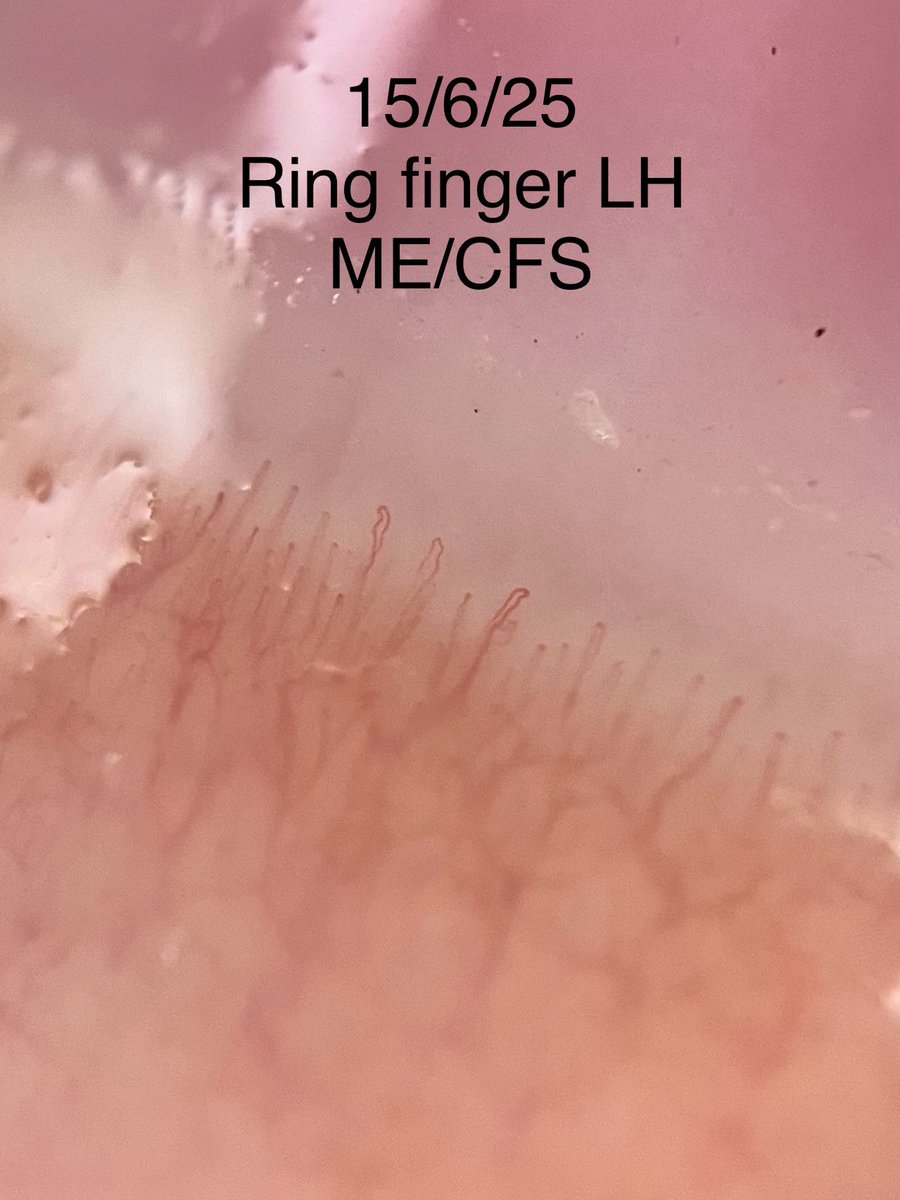
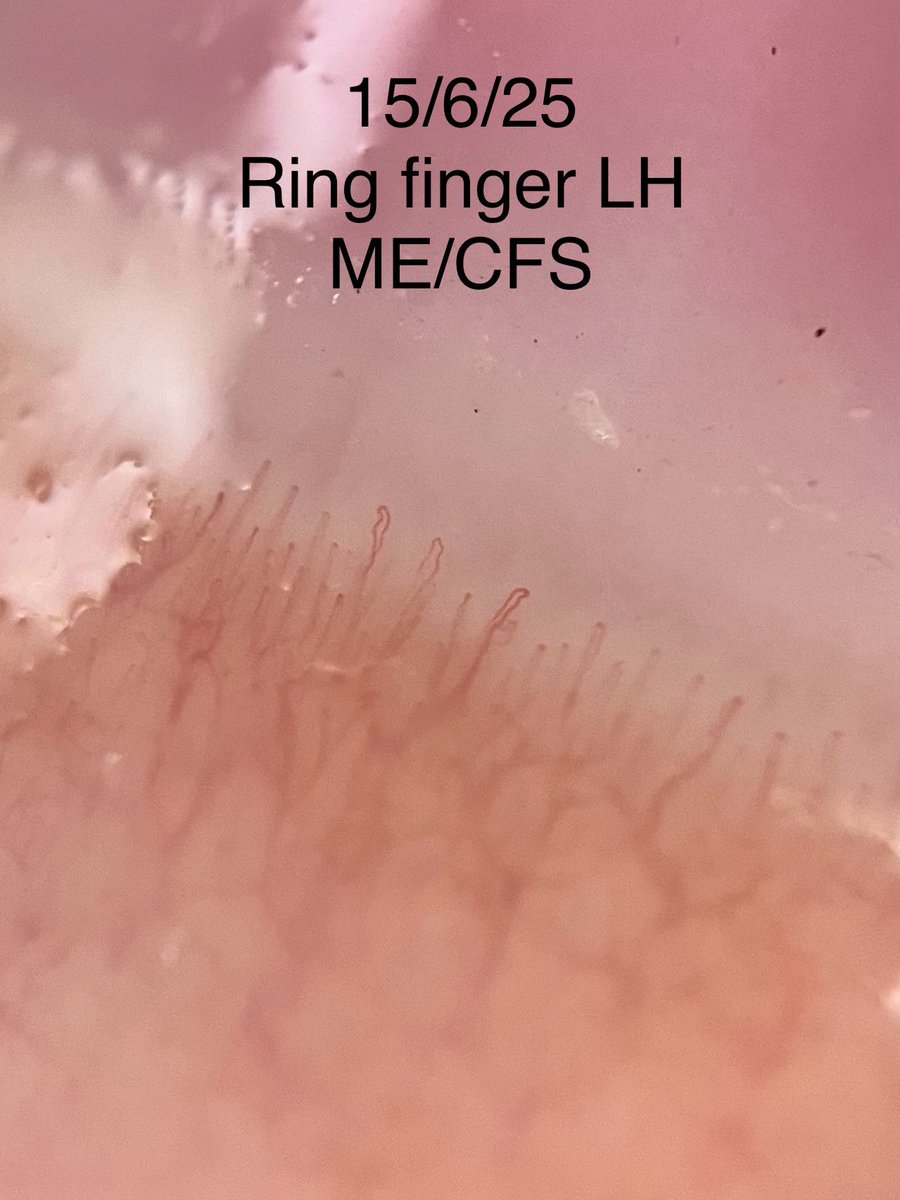
Zoologist. She/her. ME/CFS since 2002, now Severe. Pro-vax but vaccine injured. Life on pause (views my own - unemployed) ♿️ https://t.co/YeMrEWwEg5
4 subscribers
How to get URL link on X (Twitter) App


https://twitter.com/c_scheibenbogen/status/1876680928766128359Seriously though, just look 👀 at these statistics:


https://twitter.com/melrobuilds/status/1942581021448225197This is the machine I have that’s closest to the one sold in the US
https://twitter.com/PeeNee2/status/1928071726606287239
 This was my thumb on the left hand. A lot fainter and sparse looking to my eye.
This was my thumb on the left hand. A lot fainter and sparse looking to my eye. 
https://twitter.com/geneticlifehack/status/1861506781933117589⬇️
https://twitter.com/naomi_d_harvey/status/1836703110653227212
https://twitter.com/naomi_d_harvey/status/1838957681240920140Dr Ramsay advocated for use of objective testing with hand grip strength measurement on consecutive days to ascertain muscle weakness and a worse performance on day 2.
https://twitter.com/naomi_d_harvey/status/1834983334553784619This applies to basic antihistamines as well as meds like Ketotifen and travel sickness meds.




https://twitter.com/Naomi_D_Harvey/status/1798075966234980663It’s a tricky one to shop for as some are just ‘grape seed’ & provide 2-3grams of grape seed powder. But what is needed is 200-400mg of OPC extract.