
We are a registered charity promoting education, communication and the sharing of knowledge to ensure safer IV fluid prescribing.
How to get URL link on X (Twitter) App

 2/
2/
 2/
2/
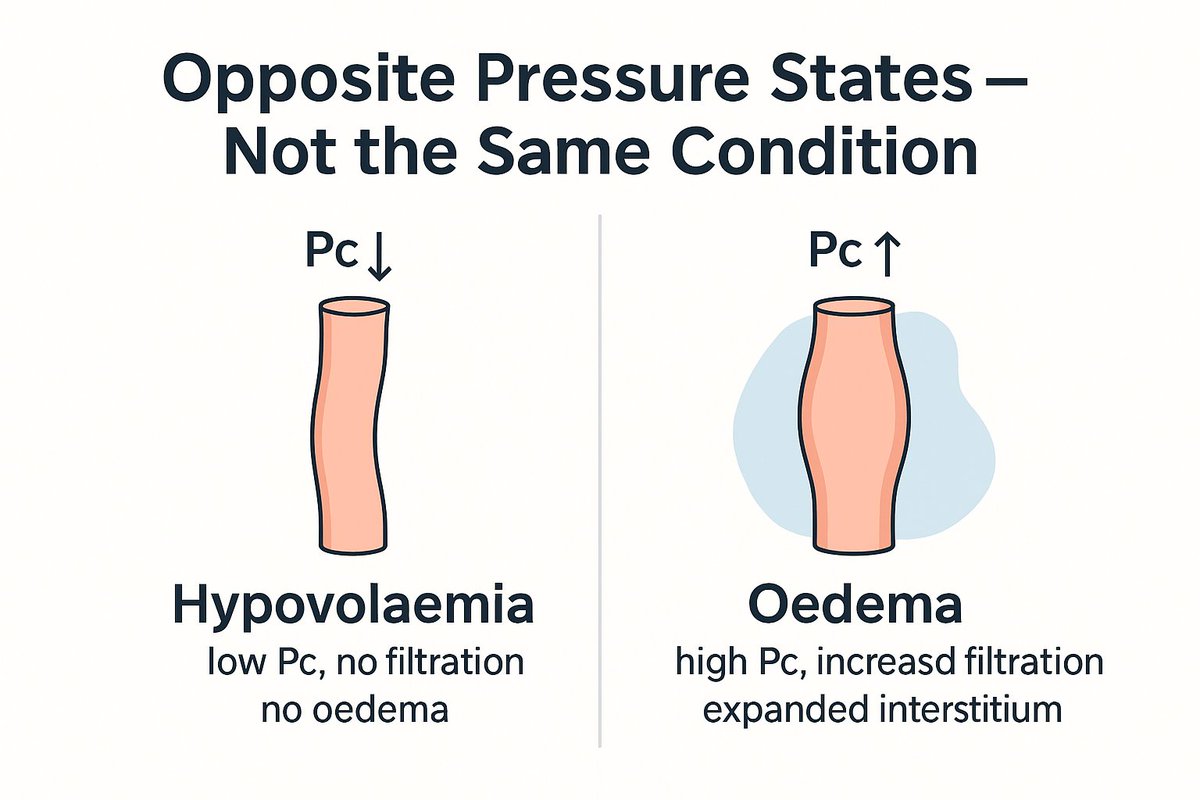
 2/ In our hypovolaemia thread we saw:
2/ In our hypovolaemia thread we saw:https://x.com/Turningthe_Tide/status/1936438468852191425

 2/
2/
 2/
2/
 2/
2/

 2. Your kidneys have an impressive range — but they need the tools.
2. Your kidneys have an impressive range — but they need the tools.

 2/
2/
 2/
2/
 The lungs are uniquely fragile:
The lungs are uniquely fragile:
 2/
2/