
Pulmonary & ICU doctor @challiance, assistant professor @HarvardMed, healthcare researcher @LabCambridge, past president @PNHP, author of "To Heal Humankind"
2 subscribers
How to get URL link on X (Twitter) App


https://twitter.com/atrupar/status/1930612560161616105An important study of the 2005 TennCare Disenrollment — a large scale Medicaid cut in Tennessee in 2005 that pushed about 170,000 out of the program — found that it was led to a 5.4 percentage point reduction in Medicaid coverage and a 4.7 percent point increase in uninsurance. Pretty similar !

 (1) This is exactly as expected because, fortunately, cases of severe COVID fell sharply after 2022 — very evident from death certificate data (and certainly observable for those of us in the ICU).
(1) This is exactly as expected because, fortunately, cases of severe COVID fell sharply after 2022 — very evident from death certificate data (and certainly observable for those of us in the ICU). 


 The above have argued that private insurance is not the real problem — the problem is those who provide healthcare. They contend the primary savings from Medicare for All-type system is not via reduced insurer waste, but lower hospital funding & clinician reimbursement.
The above have argued that private insurance is not the real problem — the problem is those who provide healthcare. They contend the primary savings from Medicare for All-type system is not via reduced insurer waste, but lower hospital funding & clinician reimbursement.

https://twitter.com/ArmandDoma/status/1864744992063000643
 This often goes unstated, I believe, because it undercuts the idea that "supply side" solutions would bring US healthcare costs in line with other nations, which is not true. We do need a PCP:specialist physician rebalancing. But the interesting thing is that increasing supply...
This often goes unstated, I believe, because it undercuts the idea that "supply side" solutions would bring US healthcare costs in line with other nations, which is not true. We do need a PCP:specialist physician rebalancing. But the interesting thing is that increasing supply...

https://twitter.com/mattyglesias/status/1864746856955154508
 And that doesn't account for provider-side administrative savings: Canadian hospitals spend half what US hospitals do on administrative **as a share of total revenue**
And that doesn't account for provider-side administrative savings: Canadian hospitals spend half what US hospitals do on administrative **as a share of total revenue**
 There is not too much controversy at this point that Medicare Advantage bilks taxpayers.
There is not too much controversy at this point that Medicare Advantage bilks taxpayers. 


 2: Not a significant difference, but 0.8% of those who got paxlovid and 1.6% of those who got placebo had a COVID-19 hospitalization or death from any cause. Underpowered for this outcome & not really high-risk group (e.g. a single death from any cause among 1,288 participants).
2: Not a significant difference, but 0.8% of those who got paxlovid and 1.6% of those who got placebo had a COVID-19 hospitalization or death from any cause. Underpowered for this outcome & not really high-risk group (e.g. a single death from any cause among 1,288 participants). 


https://twitter.com/TRyanGregory/status/1654840715850002432
 It shouldn't need to be said: severe COVID, manifested as overwhelming pneumonia, is as ghastly as described, the cause of horrifying surges in deaths and a once-in-a-century pandemic.
It shouldn't need to be said: severe COVID, manifested as overwhelming pneumonia, is as ghastly as described, the cause of horrifying surges in deaths and a once-in-a-century pandemic.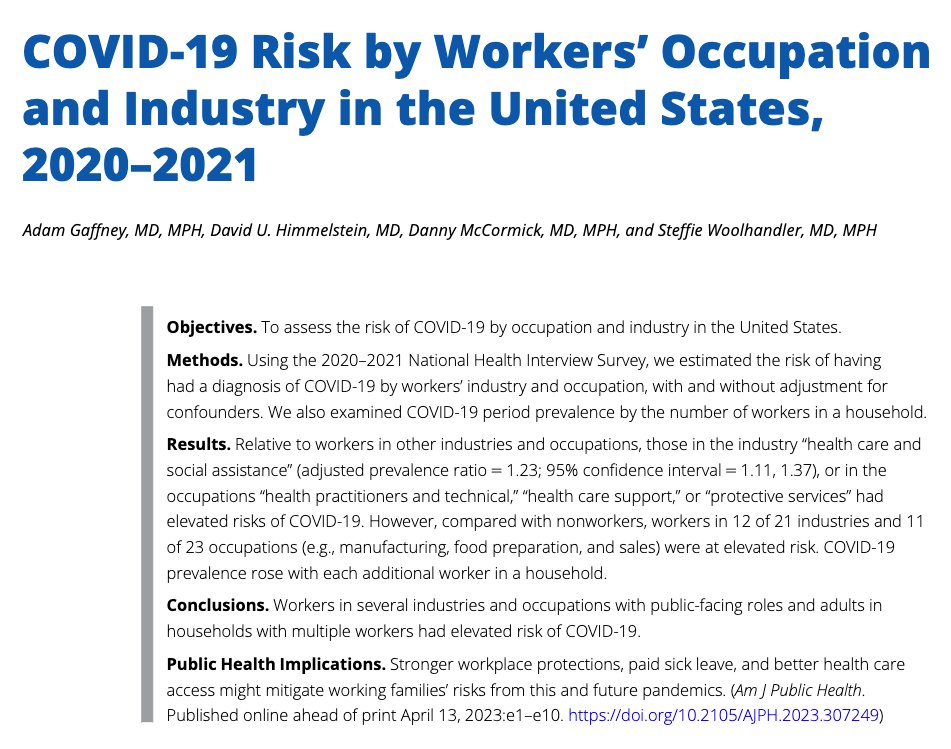
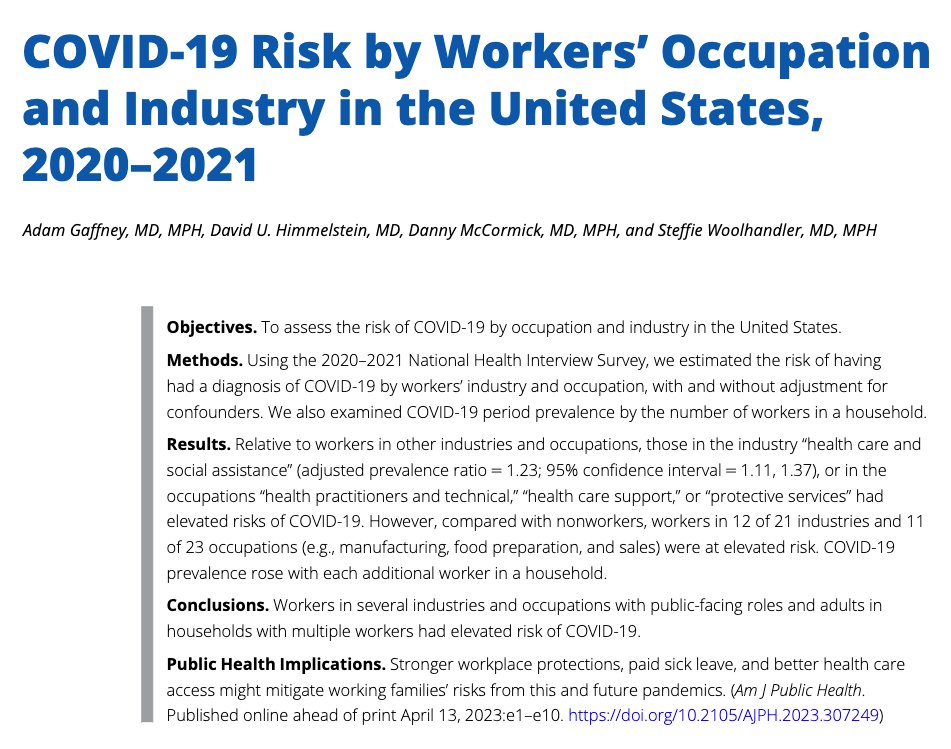 Many studies have identified workplaces as important site of COVID spread. And national data show disparities in death by occupation — although death risk can also reflect differences in health status, & death-certificate data may not account for many confounding factors.
Many studies have identified workplaces as important site of COVID spread. And national data show disparities in death by occupation — although death risk can also reflect differences in health status, & death-certificate data may not account for many confounding factors.

 Using numerous historical & current data sources, we examined public vs. private financing AND ownership of US healthcare over the past 100 years.
Using numerous historical & current data sources, we examined public vs. private financing AND ownership of US healthcare over the past 100 years. 
 Fundamentally the reason why cost control happens in most nations with national health insurance OR national health service systems is the same: single-source public financing (a point made by Robert Evans some years ago), which effectively creates the political *means* &
Fundamentally the reason why cost control happens in most nations with national health insurance OR national health service systems is the same: single-source public financing (a point made by Robert Evans some years ago), which effectively creates the political *means* &