Cardiologist and researcher, in cardiovascular magnetic resonance imaging, at the University of Minnesota
How to get URL link on X (Twitter) App

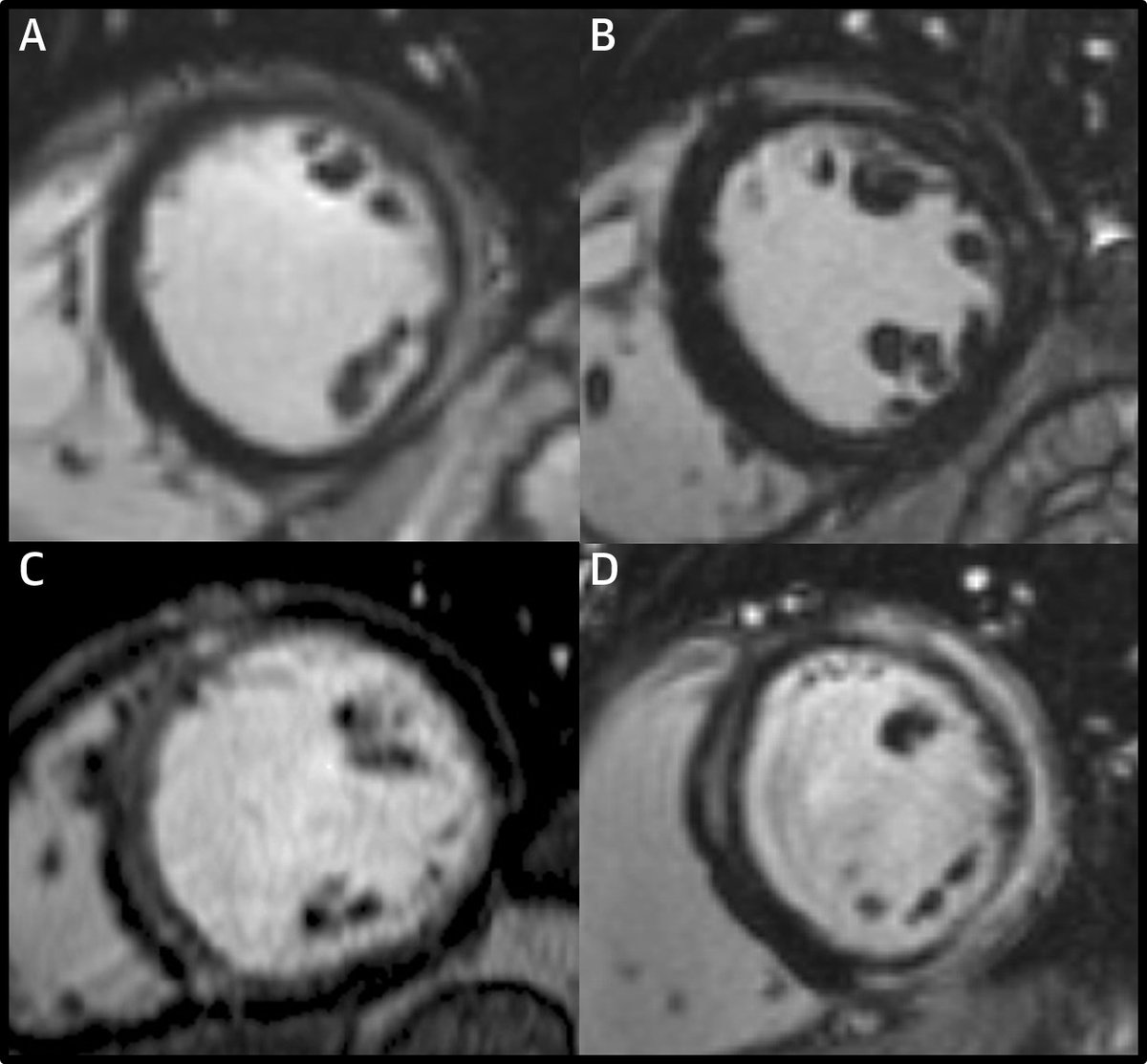
https://twitter.com/MAecocardio/status/1469990529920290817First, was the LGE in this study an artifact ("overcalling")?
https://twitter.com/VDelgadoGarcia/status/1469992047281156103?s=20


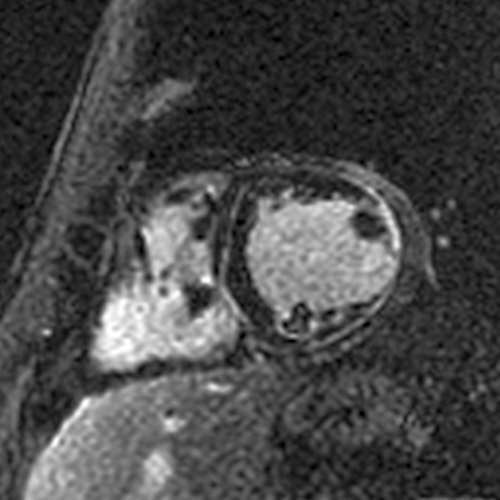
https://twitter.com/cshenoy3/status/1194307122017849345?s=20The first is a case of Desmoplakin cardiomyopathy that we published a few years ago:
https://twitter.com/pnagpalMD/status/1387381414698627072The lateral wall involvement spares the most subendocardial portion and/or the papillary muscles and trabeculations, indicating it is subepicardial (unlike a transmural MI that started subendocardially and involves the papillary muscles/trabeculations).