POCUS, NBE CCE diplomat, Echo, Resuscitation, VExUS, Emergency Medicine, 🏴
2 subscribers
How to get URL link on X (Twitter) App








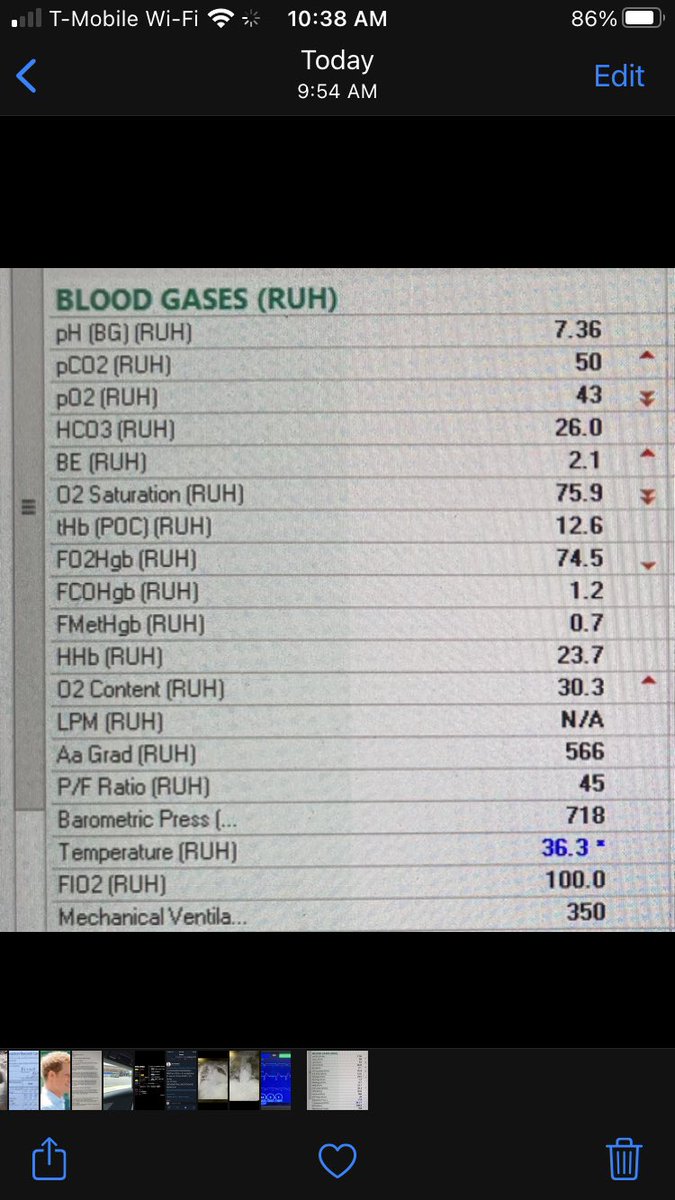
 2/ Initial vent settings were with 6cc/kg TV. Initial ABG on FiO2 100% is seen below.
2/ Initial vent settings were with 6cc/kg TV. Initial ABG on FiO2 100% is seen below.