
In-depth analysis of research on myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
4 subscribers
How to get URL link on X (Twitter) App


 2) The TIMES questionnaires is based on the DePaul Symptom Questionnaire (DSQ) but the authors adapted it to make it more suitable for clinical assessment (rather than diagnosis).
2) The TIMES questionnaires is based on the DePaul Symptom Questionnaire (DSQ) but the authors adapted it to make it more suitable for clinical assessment (rather than diagnosis). 
 2) The project will be based at the UK Dementia Research Institute’s Fluid Biomarker Laboratory.
2) The project will be based at the UK Dementia Research Institute’s Fluid Biomarker Laboratory.
 2) The researchers split the participants into two groups and told one of them (the catastrophizing group) that a few people who did the experiment fainted during the ice-water immersion. And the people who fainted had similar responses to the questionnaire as you.
2) The researchers split the participants into two groups and told one of them (the catastrophizing group) that a few people who did the experiment fainted during the ice-water immersion. And the people who fainted had similar responses to the questionnaire as you.
https://twitter.com/mecfsskeptic/status/2005671302196043946
 2) The Netherlands Brain Bank has 40 years of experience.
2) The Netherlands Brain Bank has 40 years of experience. 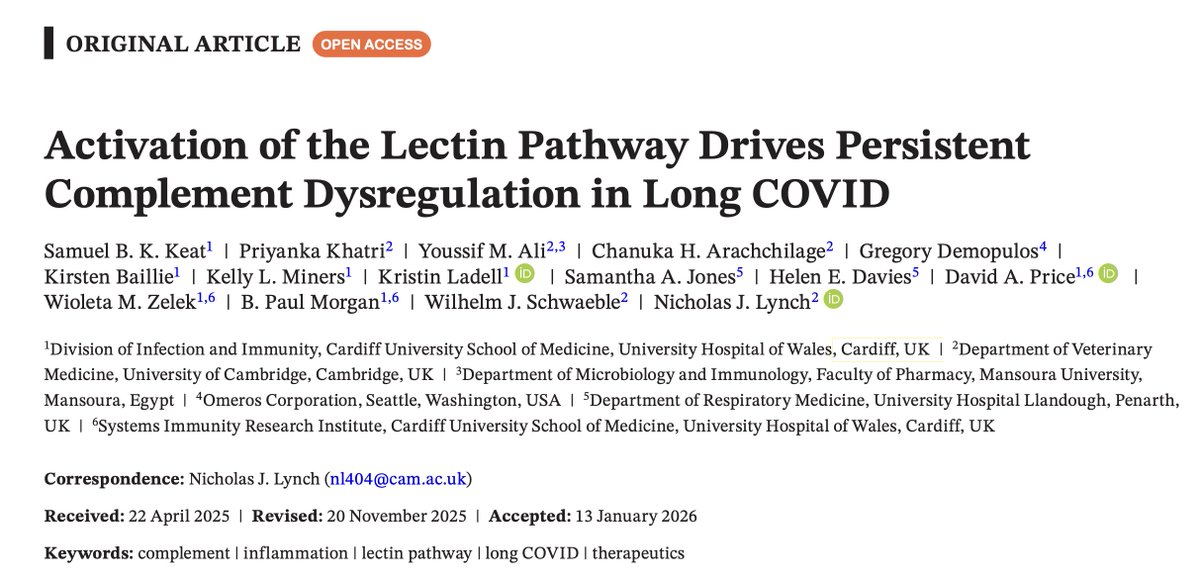
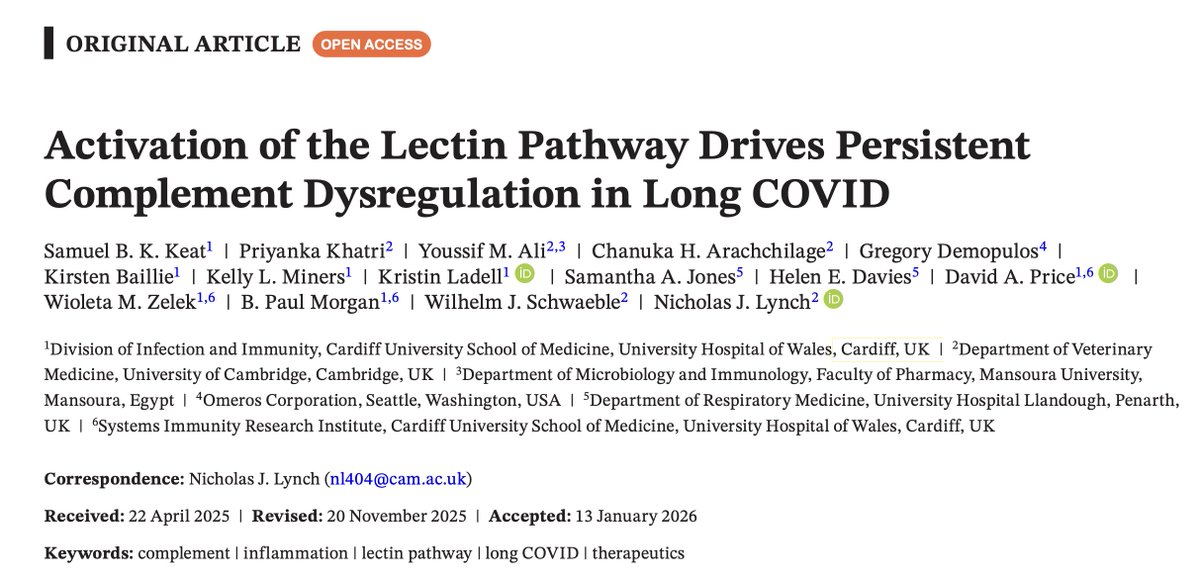 2) The complement system consists of tiny proteins all over your body that can be activated to initiate an immune response and tagg pathogens so that you immune cells can more easily catch and destroy them.
2) The complement system consists of tiny proteins all over your body that can be activated to initiate an immune response and tagg pathogens so that you immune cells can more easily catch and destroy them.
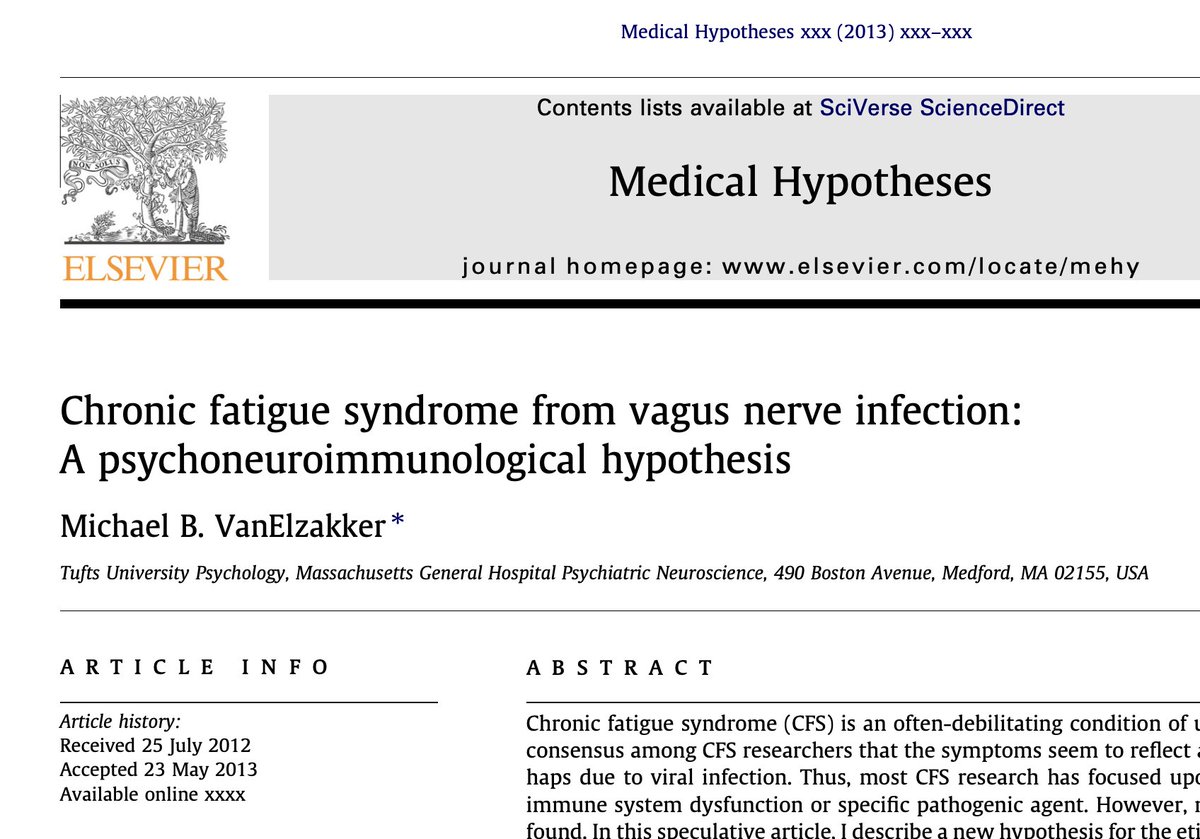
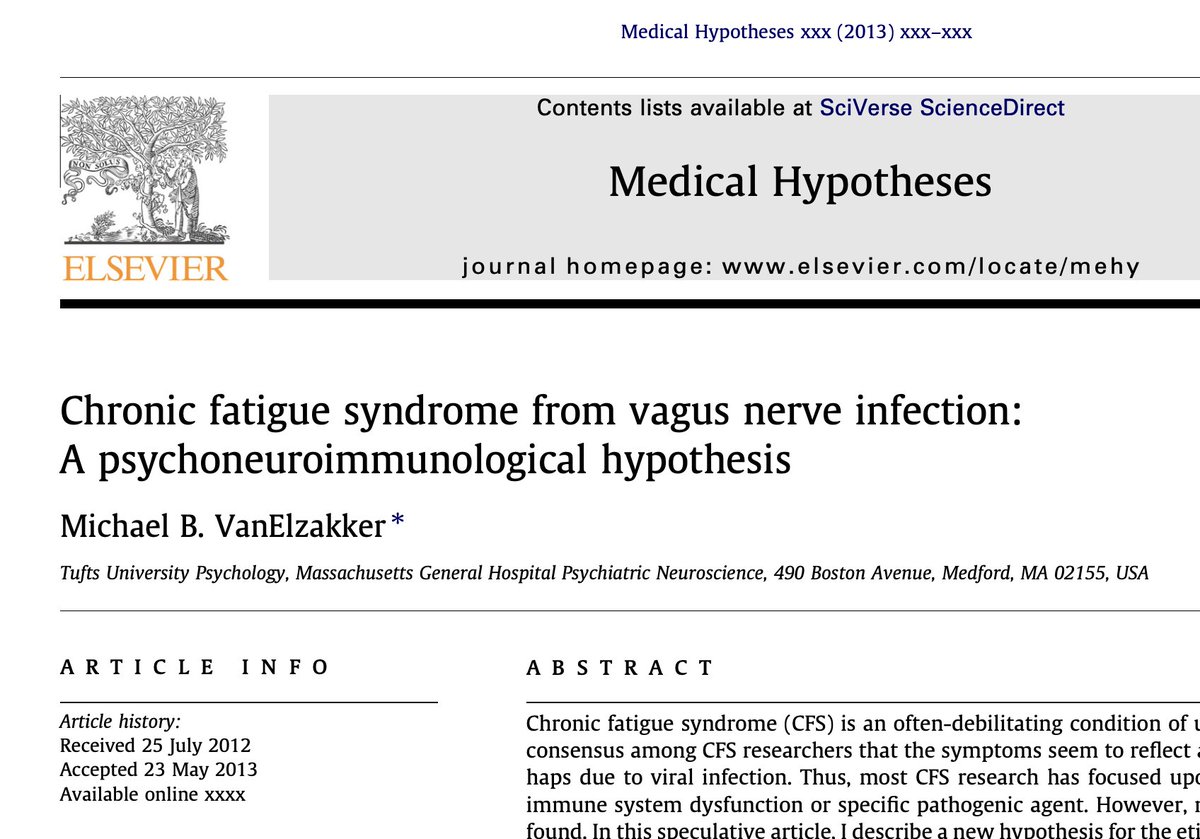 2) The vagus nerve is like a highway from your brainstem all the way down to your abdomen, wandering (vagus means wandering in Latin) through major organs along the way.
2) The vagus nerve is like a highway from your brainstem all the way down to your abdomen, wandering (vagus means wandering in Latin) through major organs along the way. 
 2) These cardiopulmonary exercise tests (CPET) involve riding a bike for about 10 minutes. The resistance is increased until you reach your maximum effort.
2) These cardiopulmonary exercise tests (CPET) involve riding a bike for about 10 minutes. The resistance is increased until you reach your maximum effort.
 2) This paper focuses on epigenetics: how our genes are switched on or off. This is done by adding methyl groups to specific pieces of DNA, making it less likely that a gene will be expressed.
2) This paper focuses on epigenetics: how our genes are switched on or off. This is done by adding methyl groups to specific pieces of DNA, making it less likely that a gene will be expressed. 
 2) The full name of the call is: HORIZON-HLTH-2026-01-DISEASE-03: Advancing research on the prevention, diagnosis, and management of post-infection long-term conditions.
2) The full name of the call is: HORIZON-HLTH-2026-01-DISEASE-03: Advancing research on the prevention, diagnosis, and management of post-infection long-term conditions. 
 2) One of the most used tests is the Digit Span Backwards, where you have to remember and repeat a series of digits in reverse order (e.g., hearing "3-8-9" and saying "9-8-3").
2) One of the most used tests is the Digit Span Backwards, where you have to remember and repeat a series of digits in reverse order (e.g., hearing "3-8-9" and saying "9-8-3").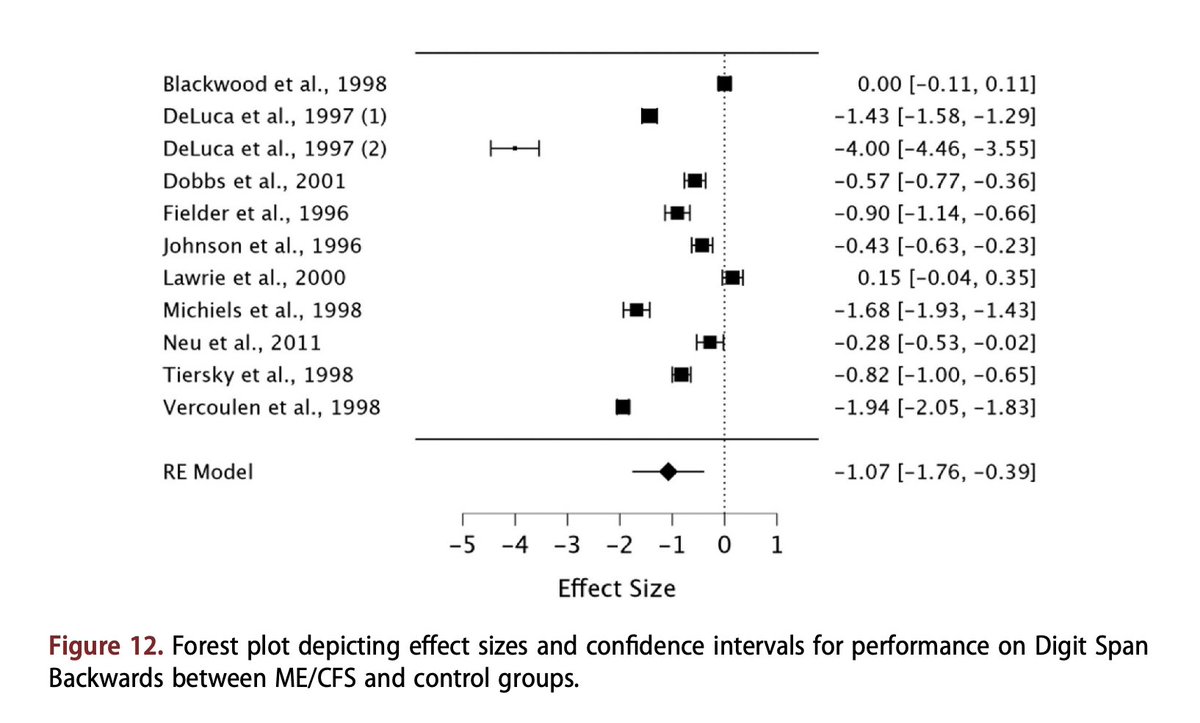

 2) During this partially active state, the virus activates some genes and proteins but doesn't fully complete its replication. So there's no increase in viral load, which would explain why no such difference has been found between ME/CFS patients and controls.
2) During this partially active state, the virus activates some genes and proteins but doesn't fully complete its replication. So there's no increase in viral load, which would explain why no such difference has been found between ME/CFS patients and controls.
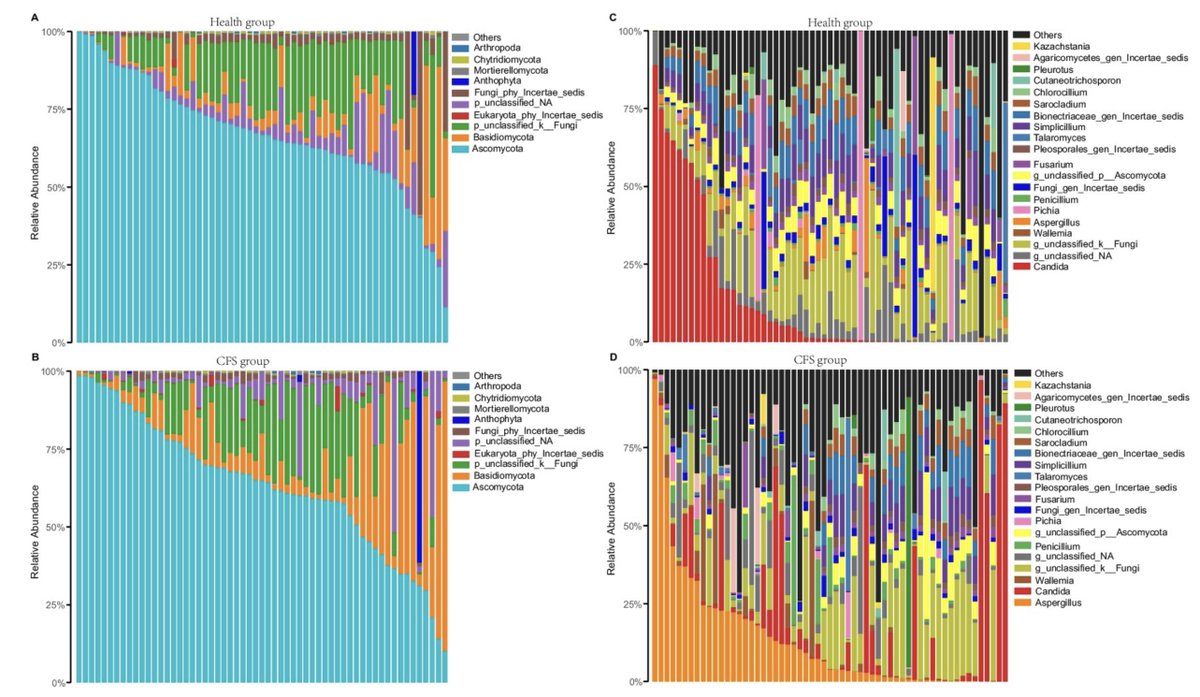
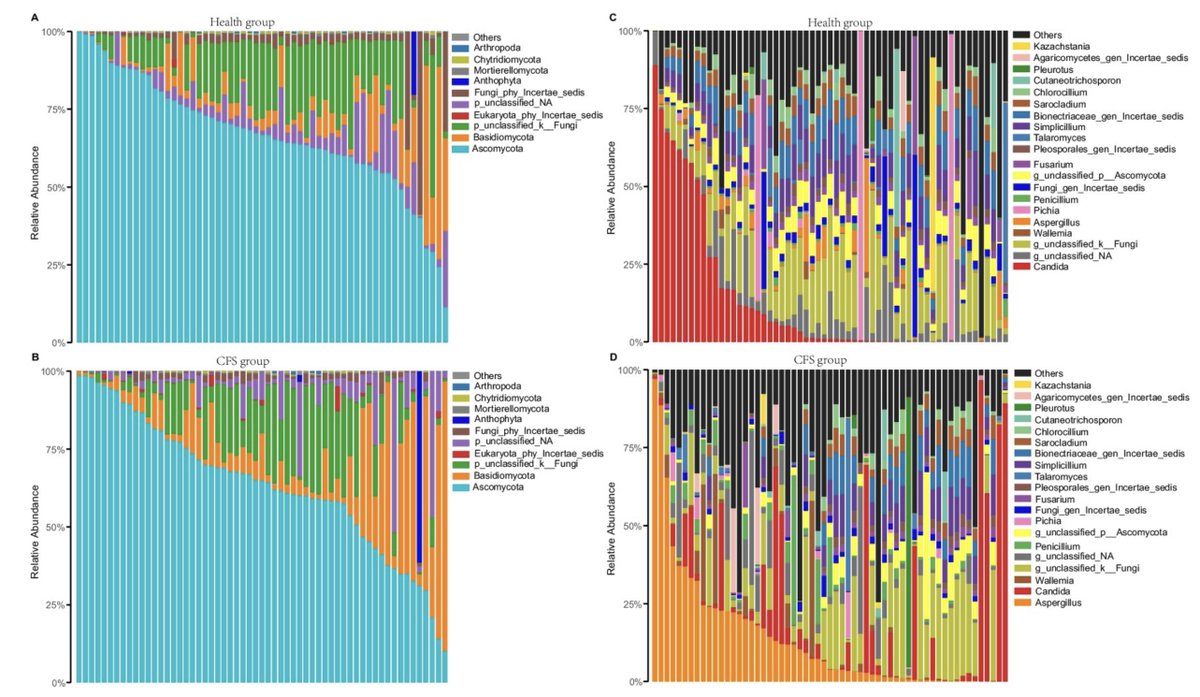 2) Overall, ME/CFS patients seemed to have less fungal diversity than controls, but because of heterogeneity (large variation within the ME/CFS group), some of the difference were not statistically significant.
2) Overall, ME/CFS patients seemed to have less fungal diversity than controls, but because of heterogeneity (large variation within the ME/CFS group), some of the difference were not statistically significant.
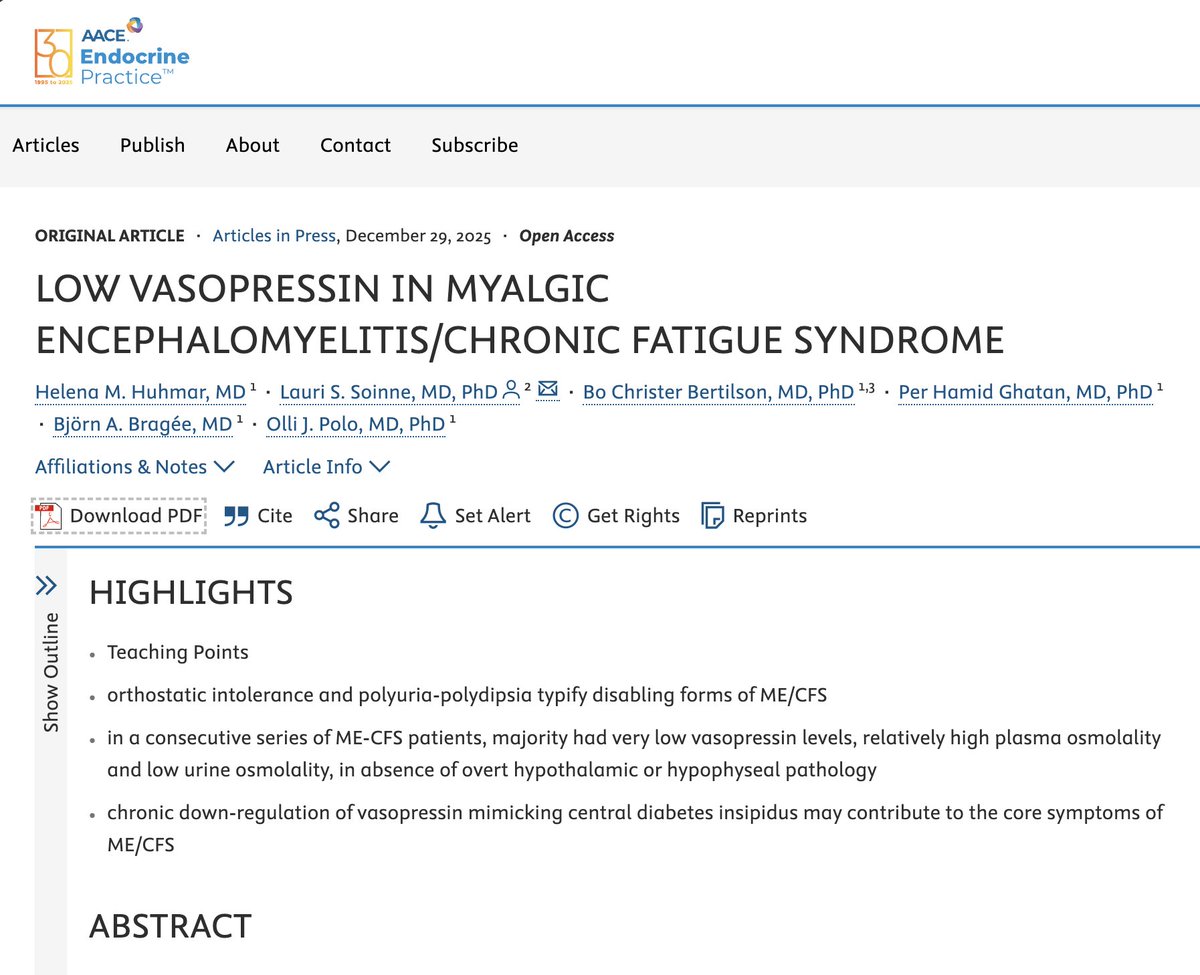
 2) The authors looked into this as ME/CFS patients often suffer from polyuria, similar to diabetes patients.
2) The authors looked into this as ME/CFS patients often suffer from polyuria, similar to diabetes patients.
 2) The biggest piece of the puzzle comes from DecodeME and the genetics study by Mark Snyder’s team at Stanford.
2) The biggest piece of the puzzle comes from DecodeME and the genetics study by Mark Snyder’s team at Stanford. 
 2) The research was done by scientists from the Netherlands Brain Bank (NBB). They received funding from the Dutch ME/CFS research agenda to store and study ME/CFS brains.
2) The research was done by scientists from the Netherlands Brain Bank (NBB). They received funding from the Dutch ME/CFS research agenda to store and study ME/CFS brains. 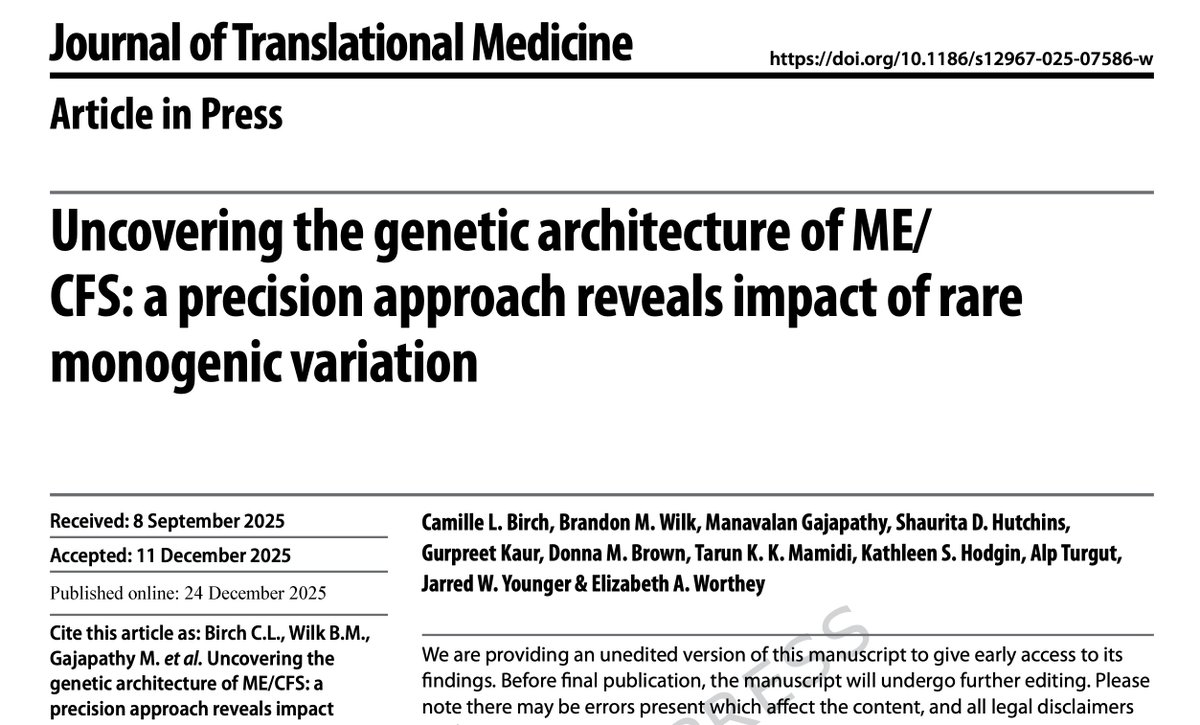
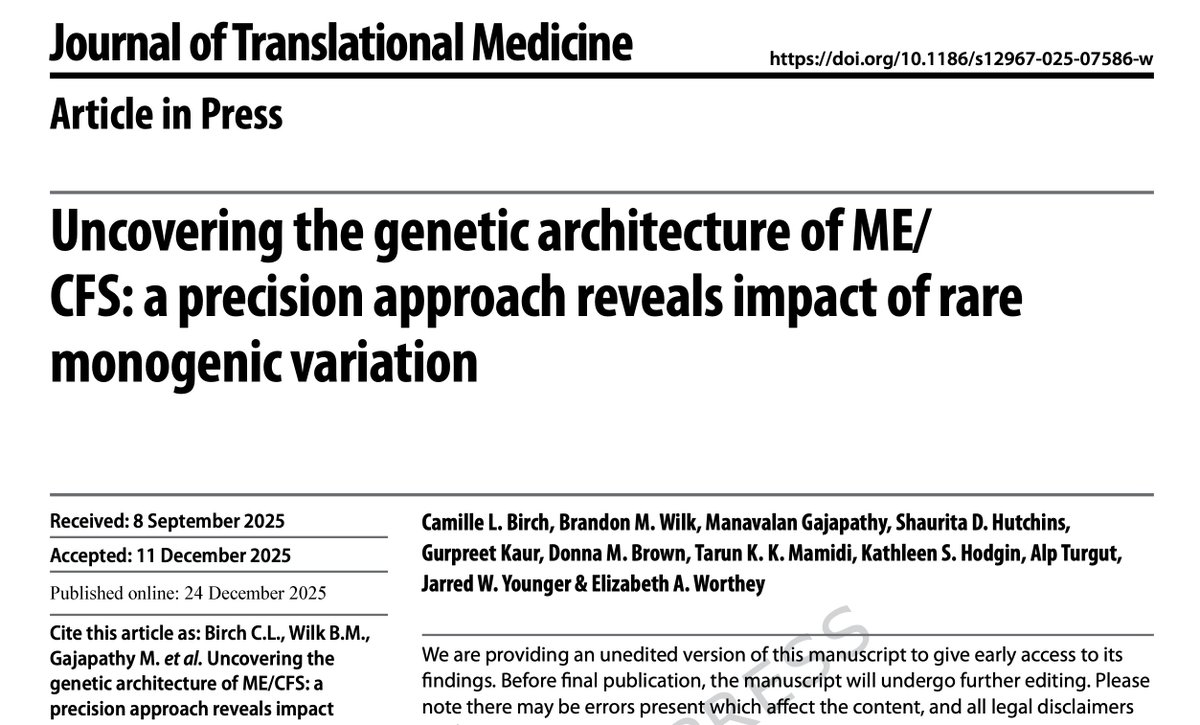 2) Take the mutations for the KCNJ18 gene which codes for a potassium channel. A 2016 study showed that mutations for this gene are "seldom pathogenic". This includes the Q407X mutation which Worthey et al. describe as "pathogenic: definitive".
2) Take the mutations for the KCNJ18 gene which codes for a potassium channel. A 2016 study showed that mutations for this gene are "seldom pathogenic". This includes the Q407X mutation which Worthey et al. describe as "pathogenic: definitive". 
 2) One patient had been ill for 3 decades and "had all her teeth removed as the severity of her illness meant that she had been unable to care for them."
2) One patient had been ill for 3 decades and "had all her teeth removed as the severity of her illness meant that she had been unable to care for them." 
 2) Even if we include funding for Ian Lipkin’s team at Columbia University (which did not appear in the database), the funding still decreased by 7% to $ 9.4 million.
2) Even if we include funding for Ian Lipkin’s team at Columbia University (which did not appear in the database), the funding still decreased by 7% to $ 9.4 million.
 2) In the white blood cells of patients, the researchers found increased AMP and a lower ATP/ADP ratio, which both hint at an issue with sufficient energy production in immune cells.
2) In the white blood cells of patients, the researchers found increased AMP and a lower ATP/ADP ratio, which both hint at an issue with sufficient energy production in immune cells.
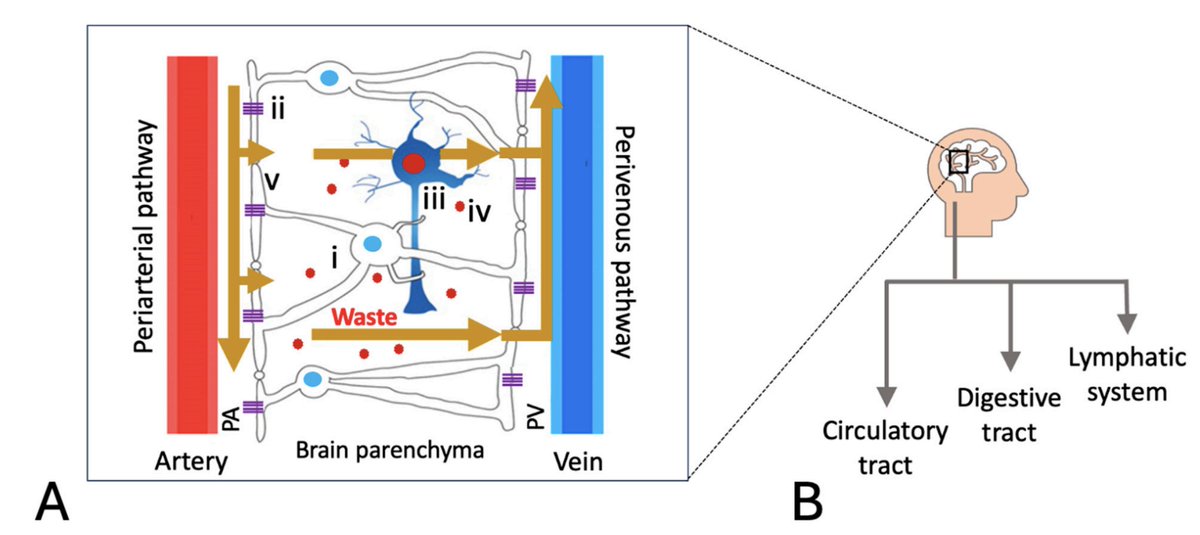
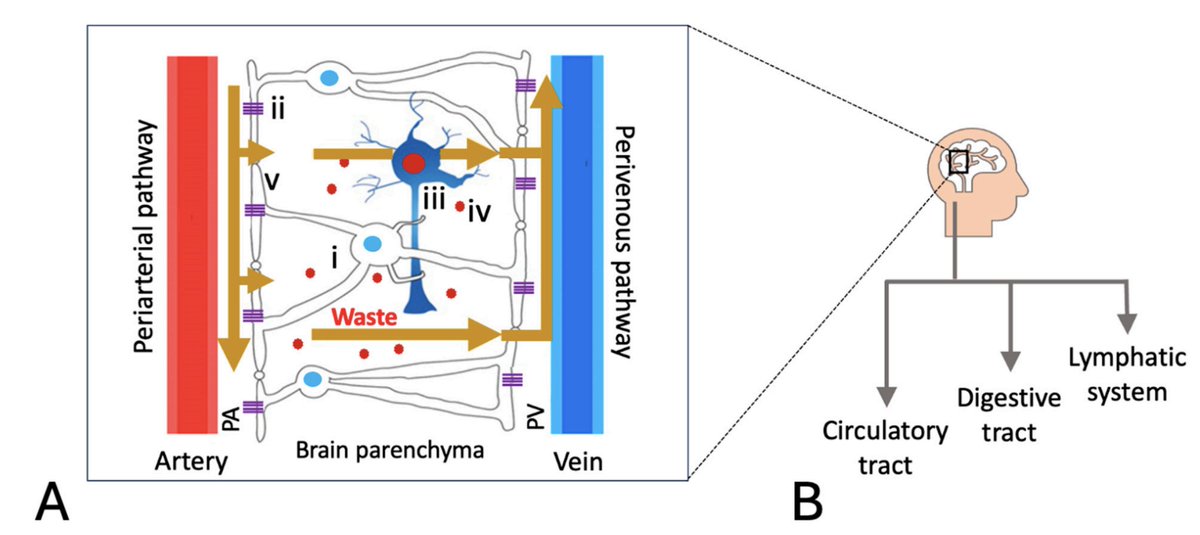 2) The glymphatic system helps to clear waste products from the brain, similar to the lymphatic system elsewhere in the body. It assists with various clean-up processes, especially during sleep.
2) The glymphatic system helps to clear waste products from the brain, similar to the lymphatic system elsewhere in the body. It assists with various clean-up processes, especially during sleep. 
 2) The study included 79 ME/CFS patients (selected using the Canadian criteria) and 53 controls. Participants underwent 2 exercise tests, and samples were collected at 5 different time points before and between these tests.
2) The study included 79 ME/CFS patients (selected using the Canadian criteria) and 53 controls. Participants underwent 2 exercise tests, and samples were collected at 5 different time points before and between these tests.