
Solving problems with technology. Chief Clinical Information Officer, Consultant Neurologist, Chair Welsh Technical Standards Board, Developer, Researcher.
2 subscribers
How to get URL link on X (Twitter) App


 1. The same data can be used for direct care, service management, continuous improvement, audit governance, and research if we do our job right. Different levels of granularity, and governance wrap, but we artificially separate these.
1. The same data can be used for direct care, service management, continuous improvement, audit governance, and research if we do our job right. Different levels of granularity, and governance wrap, but we artificially separate these. 

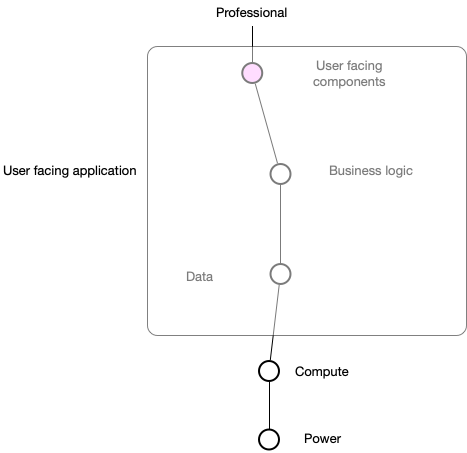
 The conventional approach means thinking in terms of applications, and not data, and is centred on organisations / providers, not the patient, or the wider ‘service’. Architecturally, it is a monolith, at least to outsides, and proprietary and organisationally-centric.
The conventional approach means thinking in terms of applications, and not data, and is centred on organisations / providers, not the patient, or the wider ‘service’. Architecturally, it is a monolith, at least to outsides, and proprietary and organisationally-centric. 

 If you look carefully, I’m asking for attributes - but I’m drilling into those and having my queries resolved by multiple microservices; this is a federated distributed electronic health record. We start at an edge and navigate seamlessly. Notice how I can resolve ethnicity and
If you look carefully, I’m asking for attributes - but I’m drilling into those and having my queries resolved by multiple microservices; this is a federated distributed electronic health record. We start at an edge and navigate seamlessly. Notice how I can resolve ethnicity and

https://twitter.com/mustbemistry/status/13732049992542003221. We want the right information at the right time, for patient, for professional, for direct care, for management, for quality improvement and for research. We use that information to make the best decisions we can.
https://twitter.com/amidgley/status/1359180844133416963For instance, I'm now able to resolve e.g. an index of deprivation score against a patient by walking the graph of properties from current address to LSOA to the index. At the client level, I don't care how those data are fulfilled.
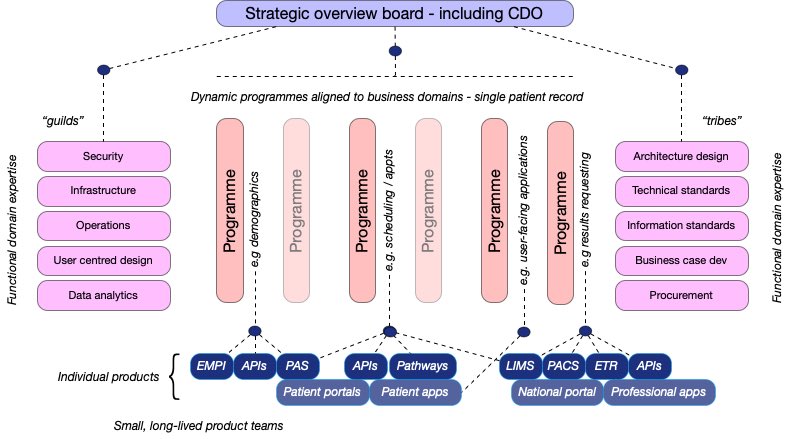
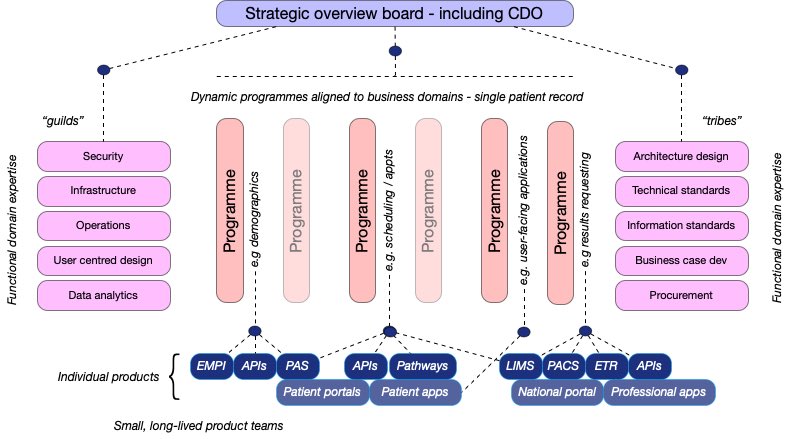
 Most us of recognise that health and care need to provide a suite of computing & data services forming a platform on which a range of user-centred solutions can be built, underpinned by robust open standards?
Most us of recognise that health and care need to provide a suite of computing & data services forming a platform on which a range of user-centred solutions can be built, underpinned by robust open standards? 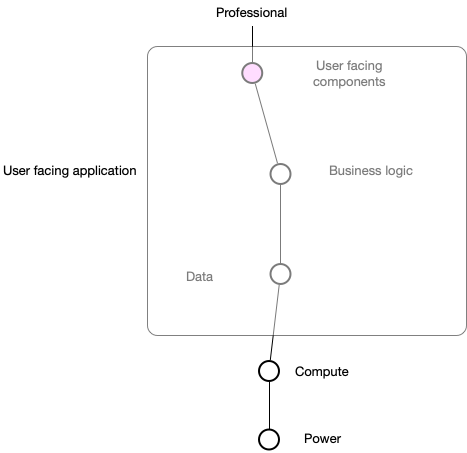
 Firstly, I’m sure that we all agree that we want to create a seamless patient-centred service that blurs the boundaries between disciplines and organisations across health and care. Likewise, we surely recognise that technology is an enabler of those ambitions.
Firstly, I’m sure that we all agree that we want to create a seamless patient-centred service that blurs the boundaries between disciplines and organisations across health and care. Likewise, we surely recognise that technology is an enabler of those ambitions.
https://twitter.com/swardley/status/1071427090812162048But not clear to me that policy-makers or industry have the foresight to embrace this new future, the next generation of electronic health systems, in which data drives decisions for direct care, service design, quality improvement, research & design of the systems themselves.
https://twitter.com/Atul_Gawande/status/1059431597546594305He gives an example of a real-life/model mismatch, thinking a single problem list can be shared within an organisation of scale. The description of the clinician’s frustration is one reason I have designed multiple context-bound problem lists based on pathways and services.

