Pulmonary & Critical Care physician at the University of Michigan. I study the microbiome's role in lung disease and critical illness.
https://t.co/pNGz1N5Wtu
How to get URL link on X (Twitter) App



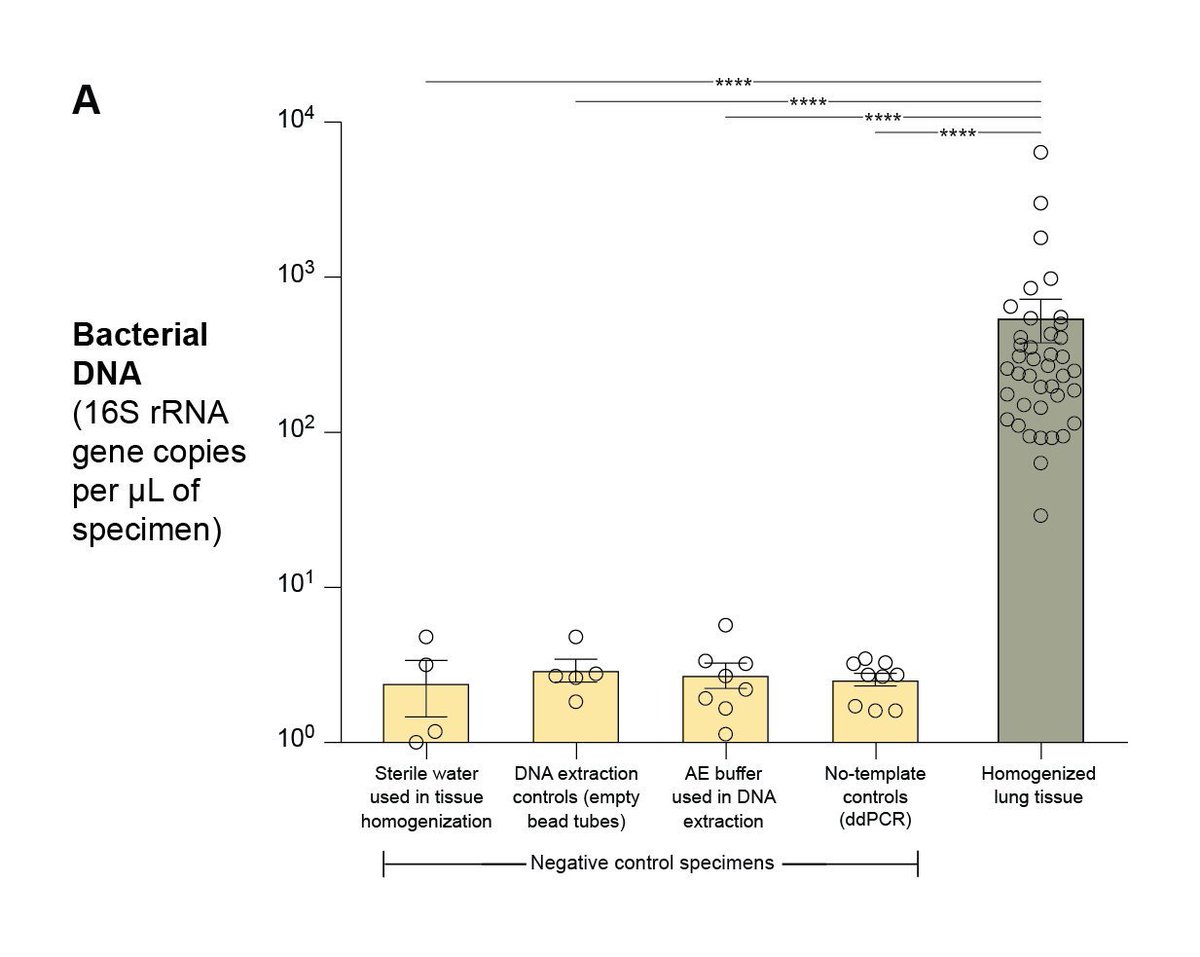
 Background: we know that gut anaerobes matter in sepsis. In multiple animal models, depleting the gut of commensal anaerobes consistently makes animals more vulnerable to infectious and non-infectious models of critical illness.
Background: we know that gut anaerobes matter in sepsis. In multiple animal models, depleting the gut of commensal anaerobes consistently makes animals more vulnerable to infectious and non-infectious models of critical illness.



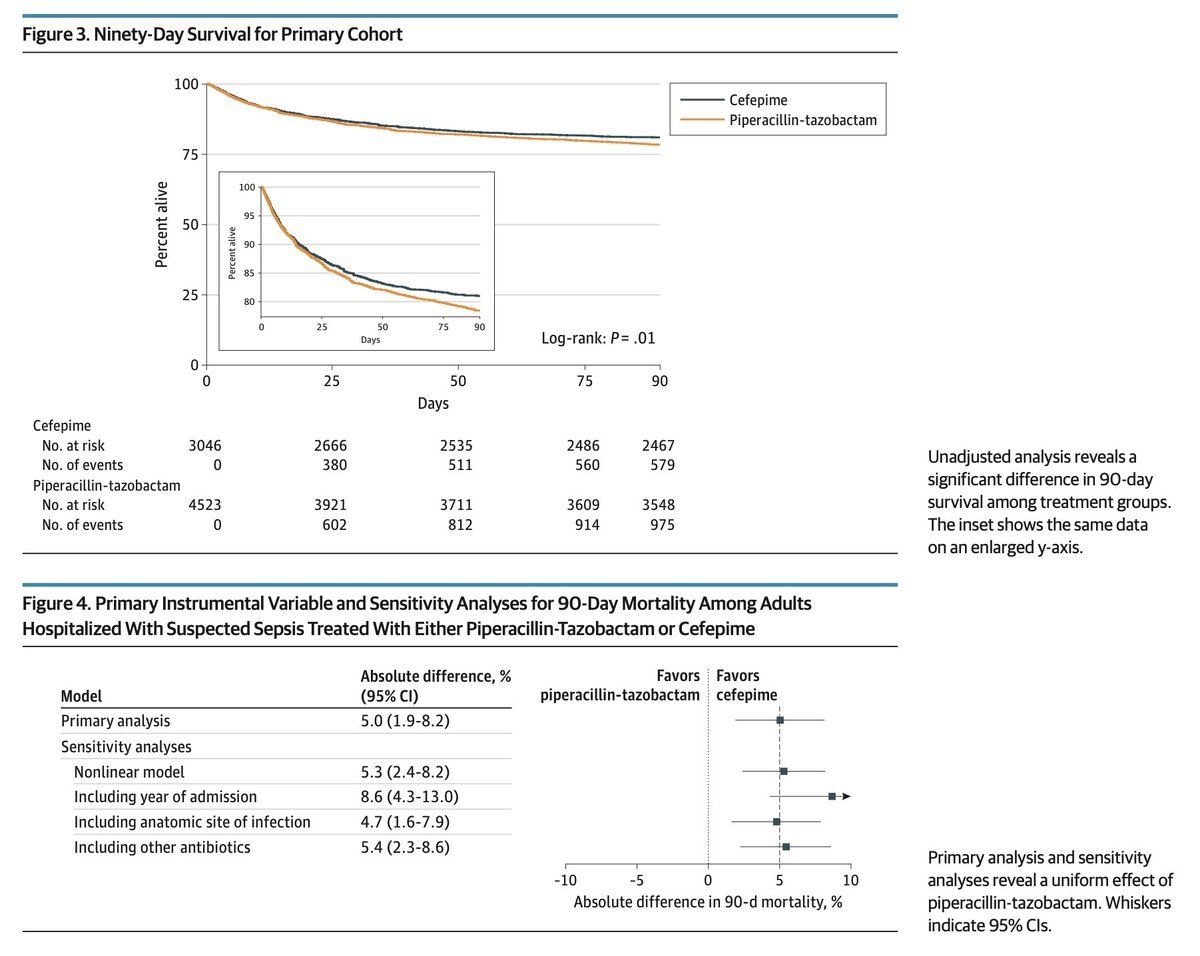
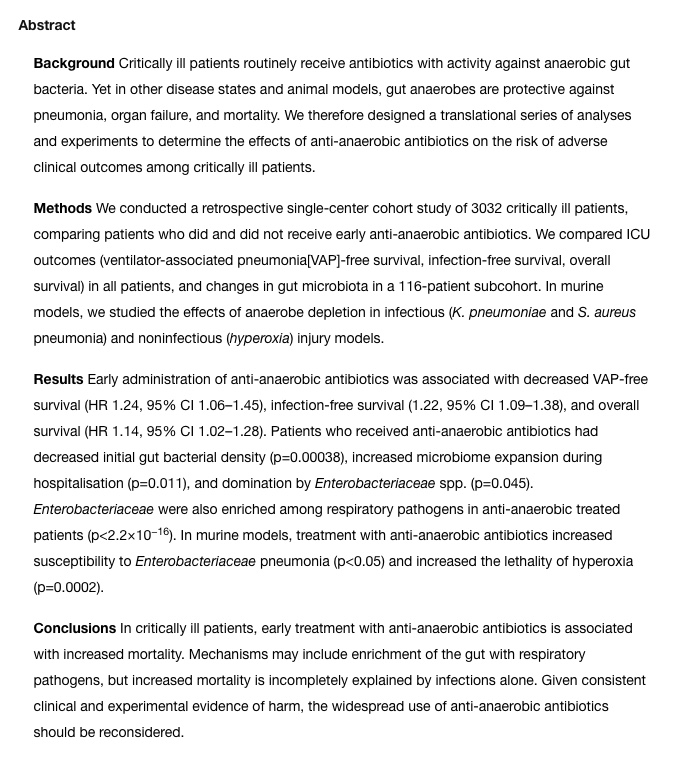 In multiple animal models, if you kill gut anaerobes, it worsens pneumonia, organ failure, and mortality. Yet we give anti-anaerobic antibiotics to patients all the time (most often pip-tazo, metronidazole, and amp-sulbactam).
In multiple animal models, if you kill gut anaerobes, it worsens pneumonia, organ failure, and mortality. Yet we give anti-anaerobic antibiotics to patients all the time (most often pip-tazo, metronidazole, and amp-sulbactam). 


 First: acknowledgements. This was ~ 5 years of work, major team effort. Shanna Ashley was its brains & motor; this was her post-doc project, and she's now a Senior Scientist @ AbbVie. Contributions from colleagues in Pulm, Micro, Peds, Path, etc. Will thank along the way.
First: acknowledgements. This was ~ 5 years of work, major team effort. Shanna Ashley was its brains & motor; this was her post-doc project, and she's now a Senior Scientist @ AbbVie. Contributions from colleagues in Pulm, Micro, Peds, Path, etc. Will thank along the way.

https://twitter.com/jopo899/status/1262125268388532225Hyaline membranes are a hallmark of diffuse alveolar damage (DAD), which is the pathological hallmark of ARDS, which has been called "hyaline membrane disease" in the past. If you had to pick one specific biologic finding that implies ARDS: hyaline membranes.