SVP @EliLillyandCo; CEO @VerveTx $VERV; We are developing one-time treatments to lower cholesterol lifelong and prevent or treat heart attack
3 subscribers
How to get URL link on X (Twitter) App


 @jsdron looked at sequence data from 2 different datasets
@jsdron looked at sequence data from 2 different datasets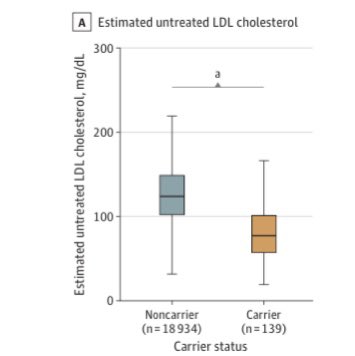


 @VerveTx first program VERVE-101 (targeting PCSK9) is designed to permanently lower LDL cholesterol after a single treatment and is intended to treat FH and ASCVD
@VerveTx first program VERVE-101 (targeting PCSK9) is designed to permanently lower LDL cholesterol after a single treatment and is intended to treat FH and ASCVD 

 We developed proprietary GalNAc-LNP last year in order to better treat patients with homozygous FH who completely lack LDLR
We developed proprietary GalNAc-LNP last year in order to better treat patients with homozygous FH who completely lack LDLR
 One-time treatment with VERVE-101
One-time treatment with VERVE-101
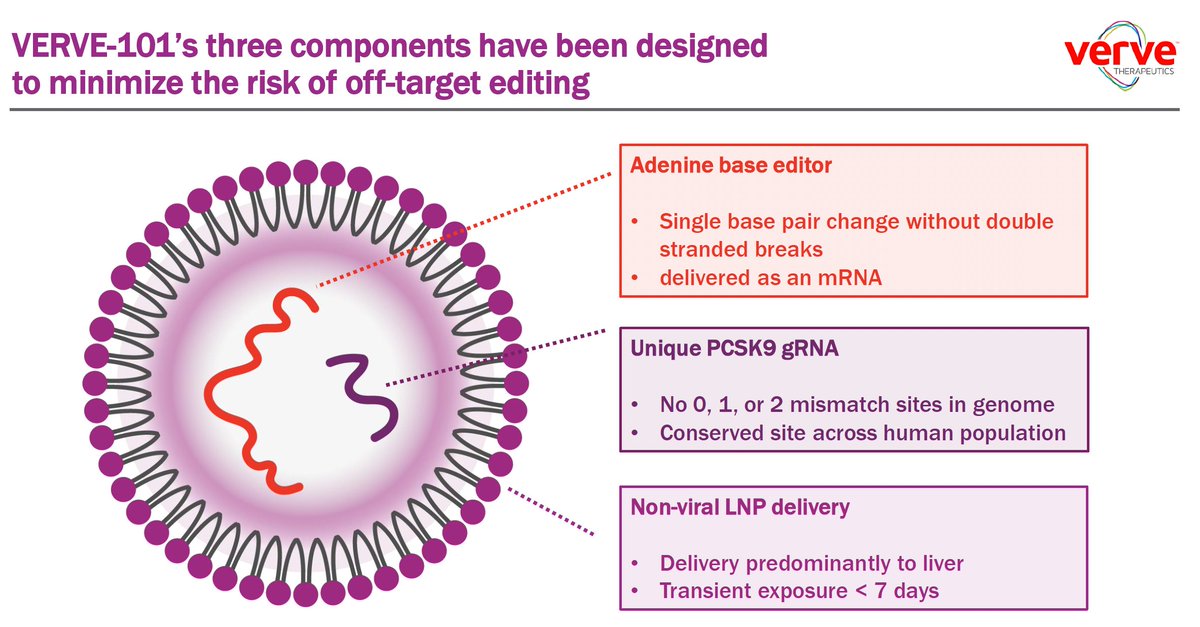
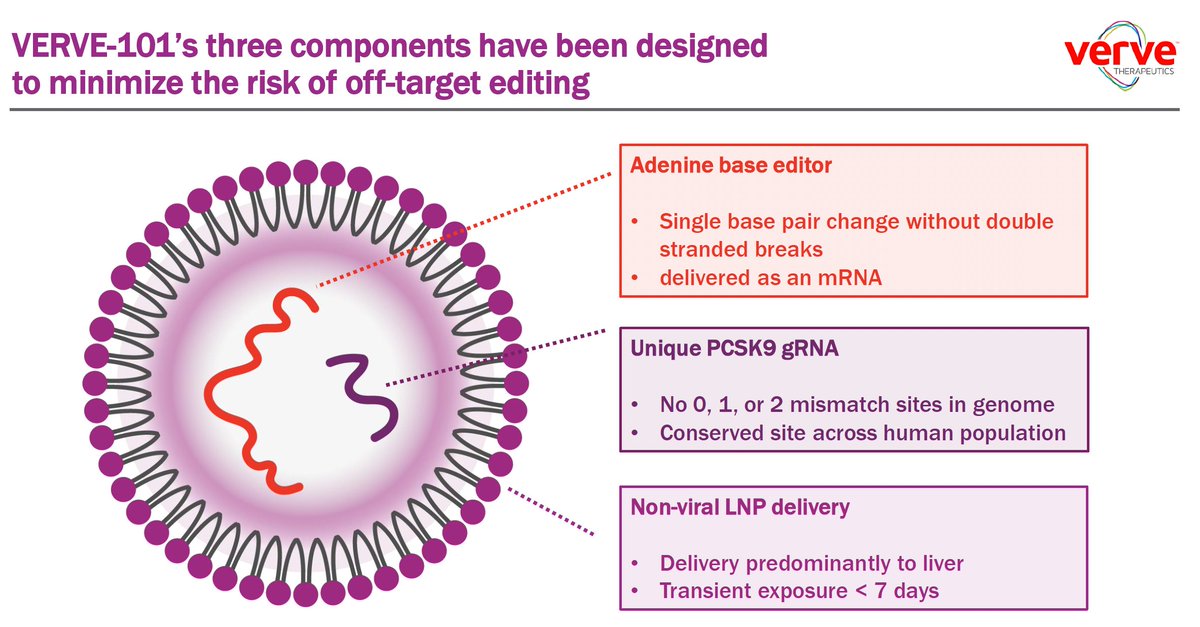 Before we get to off-target, let's look at on-target site in PCSK9 gene
Before we get to off-target, let's look at on-target site in PCSK9 gene

 NHPs treated:
NHPs treated:

 some ASCVD patients start with very-high LDL
some ASCVD patients start with very-high LDL 

 New large NHP study (n=36) with clinical formulation VERVE-101
New large NHP study (n=36) with clinical formulation VERVE-101

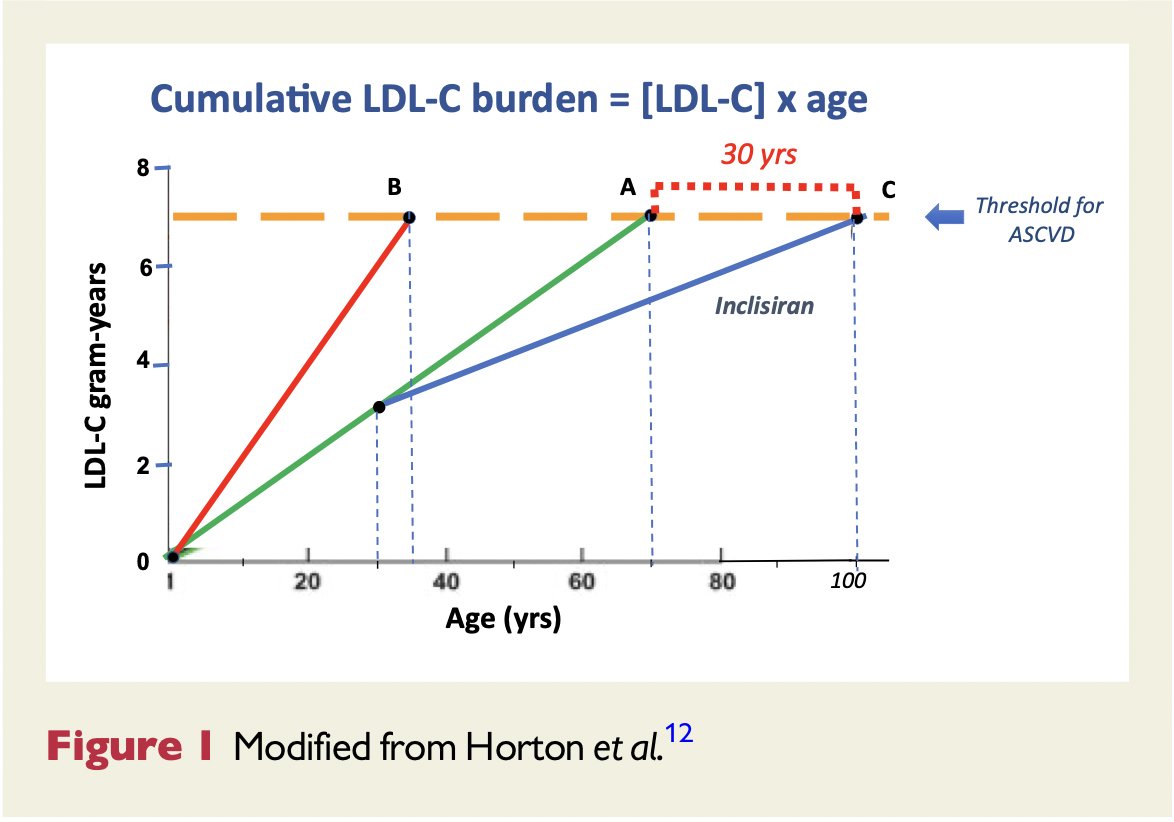
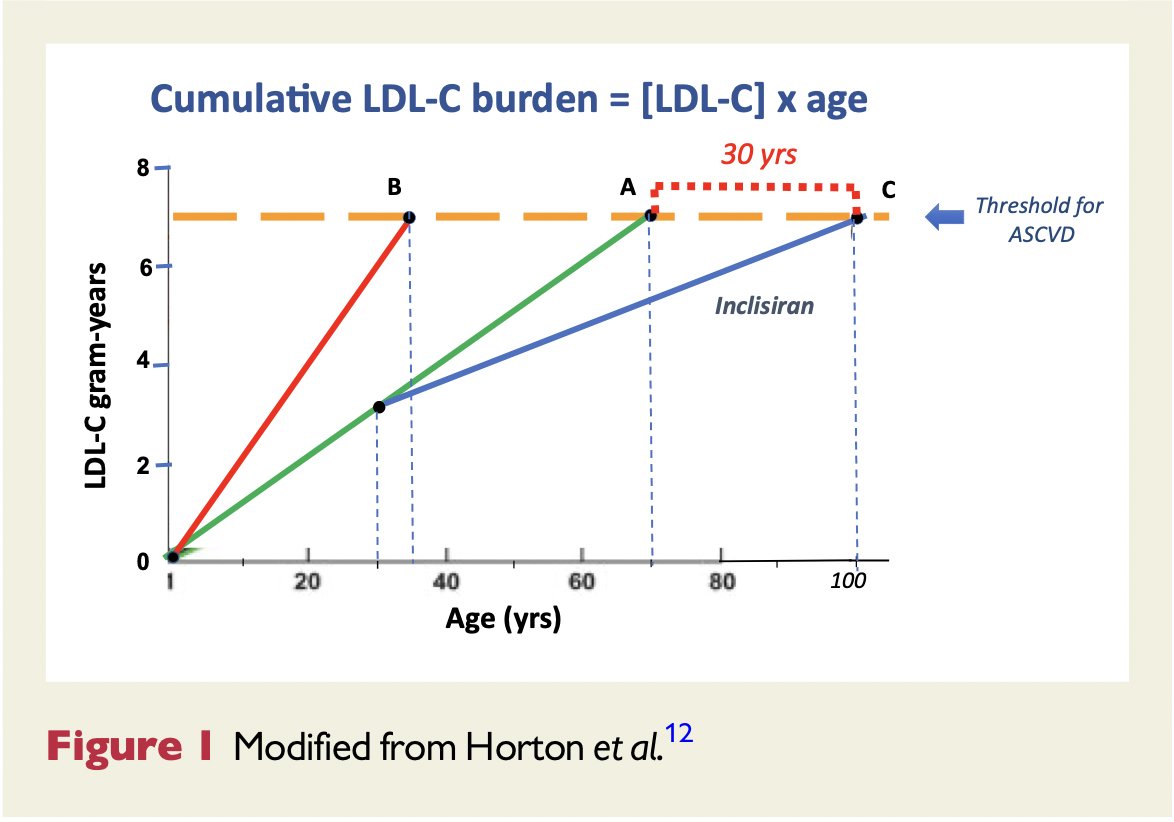 1. "general agreement that LDL-C is the most important risk factor for atherosclerosis & causal role in the development of ASCVD."
1. "general agreement that LDL-C is the most important risk factor for atherosclerosis & causal role in the development of ASCVD."
 A most surprising finding:
A most surprising finding:


 What's happening with this treatment to lead to potent, durable LDL lowering?
What's happening with this treatment to lead to potent, durable LDL lowering?


 (LDL, 2005) thelancet.com/action/showPdf…
(LDL, 2005) thelancet.com/action/showPdf…


 And look at all the metabolic benefits of the weight loss:
And look at all the metabolic benefits of the weight loss:


 evinacumab targeting ANGPTL3, IV infusion q4 wks
evinacumab targeting ANGPTL3, IV infusion q4 wks
 @broadinstitute @MassGeneralNews @MGHHeartHealth @VerveTx 2010 👇🏽
@broadinstitute @MassGeneralNews @MGHHeartHealth @VerveTx 2010 👇🏽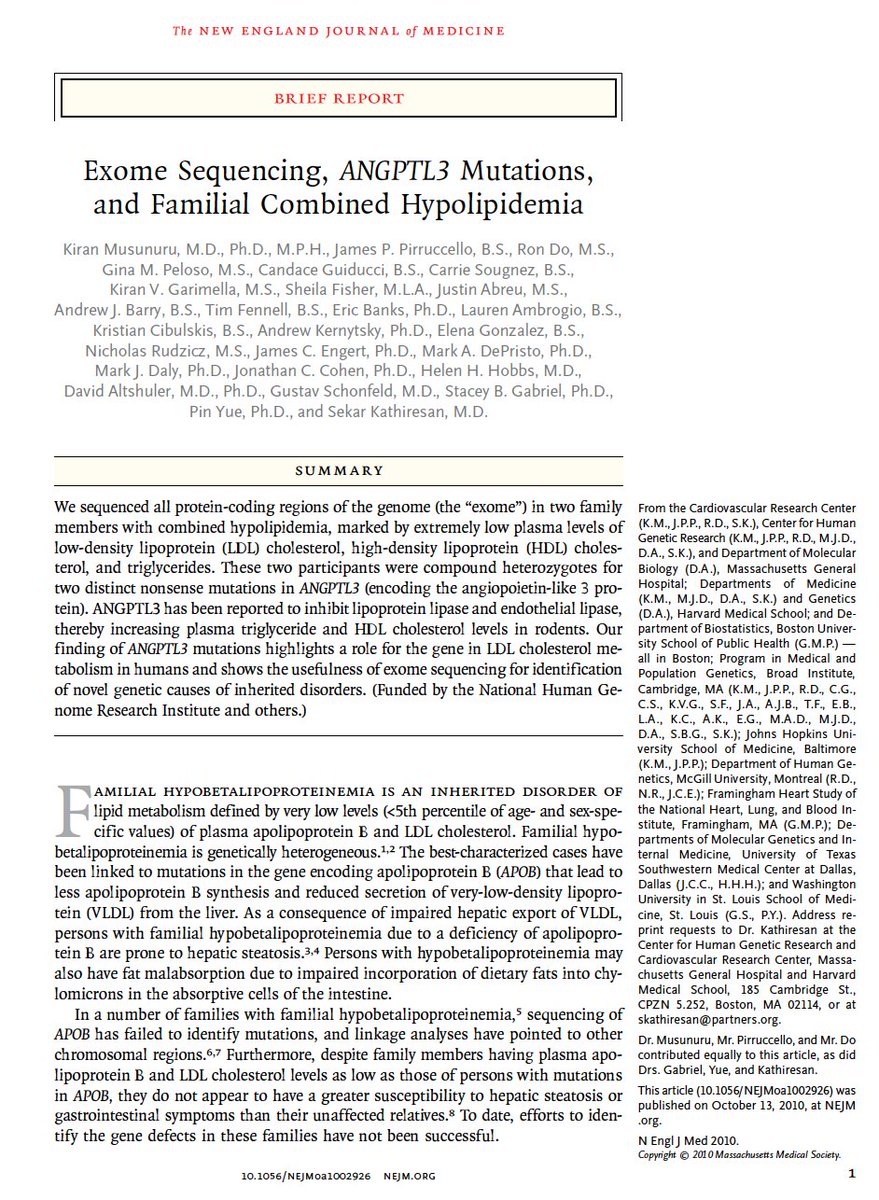


 @medrxivpreprint @amitvkhera @Color @broadinstitute @MassGeneralNews For breast cancer, polygenic background:
@medrxivpreprint @amitvkhera @Color @broadinstitute @MassGeneralNews For breast cancer, polygenic background:
https://twitter.com/JACCJournals/status/1183012877235609600Recently studied 2,081 pts (66%♀️) who had suffered a heart attack age <= 55 yo

 @VerveTx has been built to address one problem - heart attack
@VerveTx has been built to address one problem - heart attack

 Here's the story of the discovery:
Here's the story of the discovery:
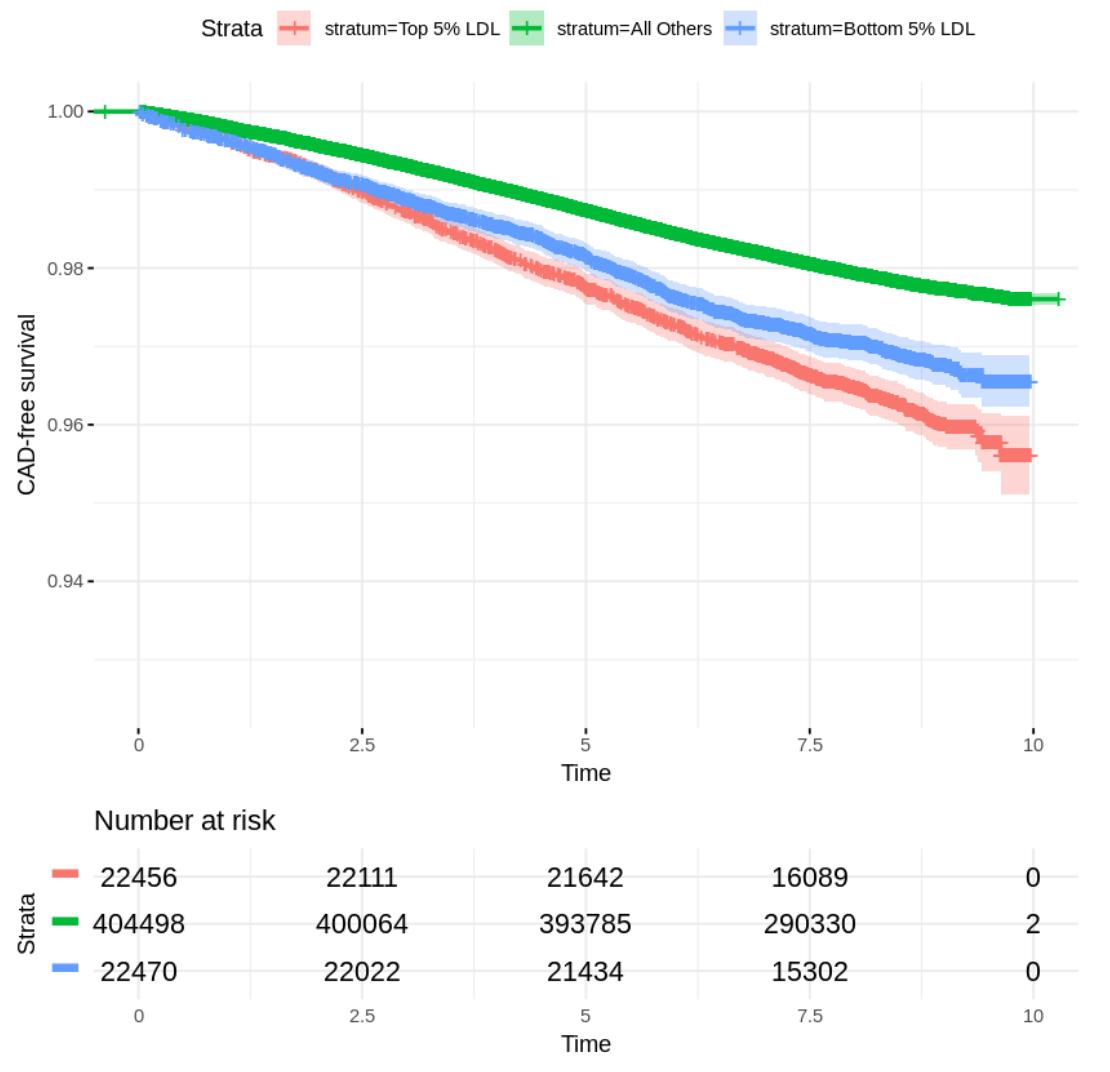
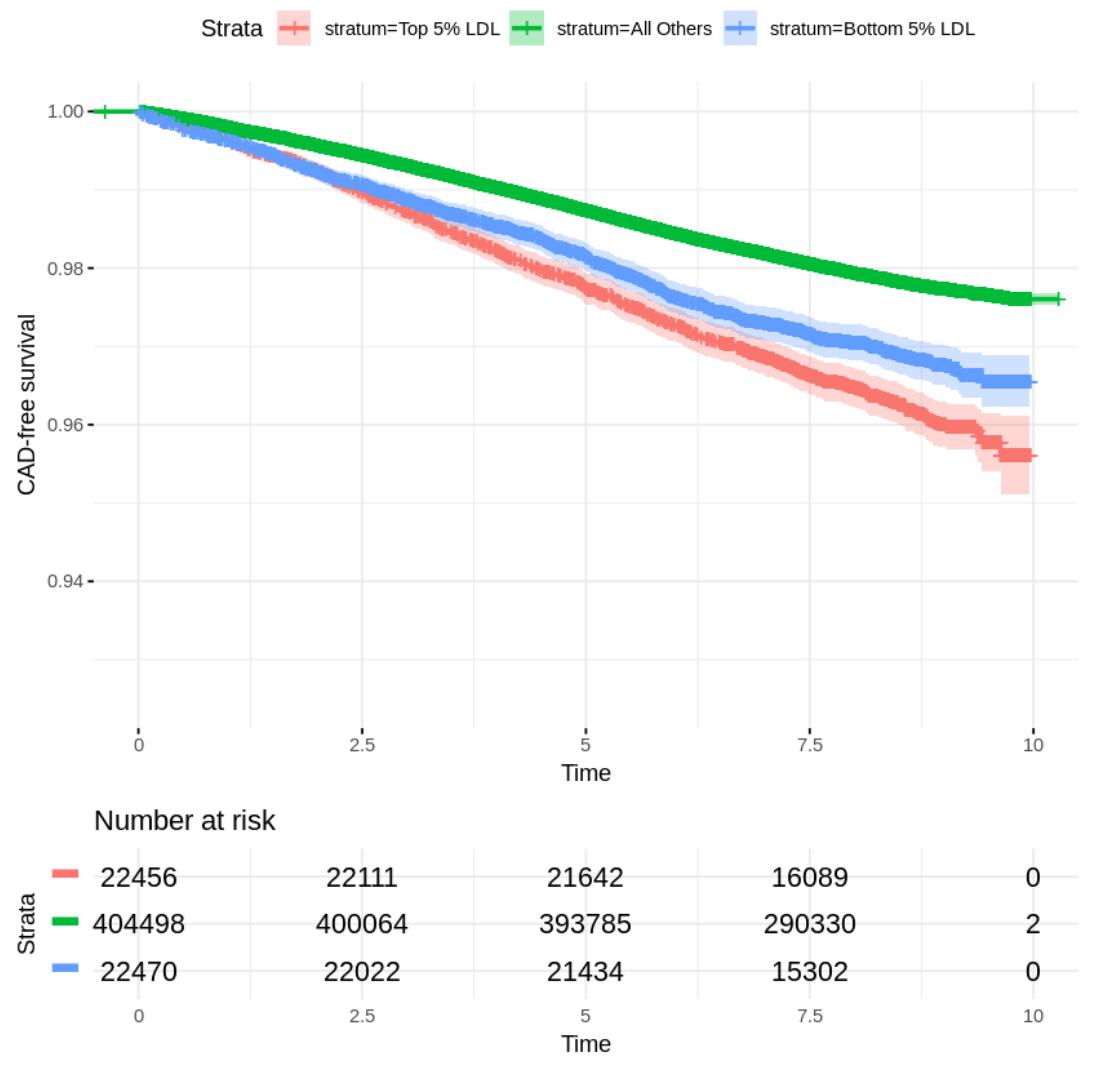
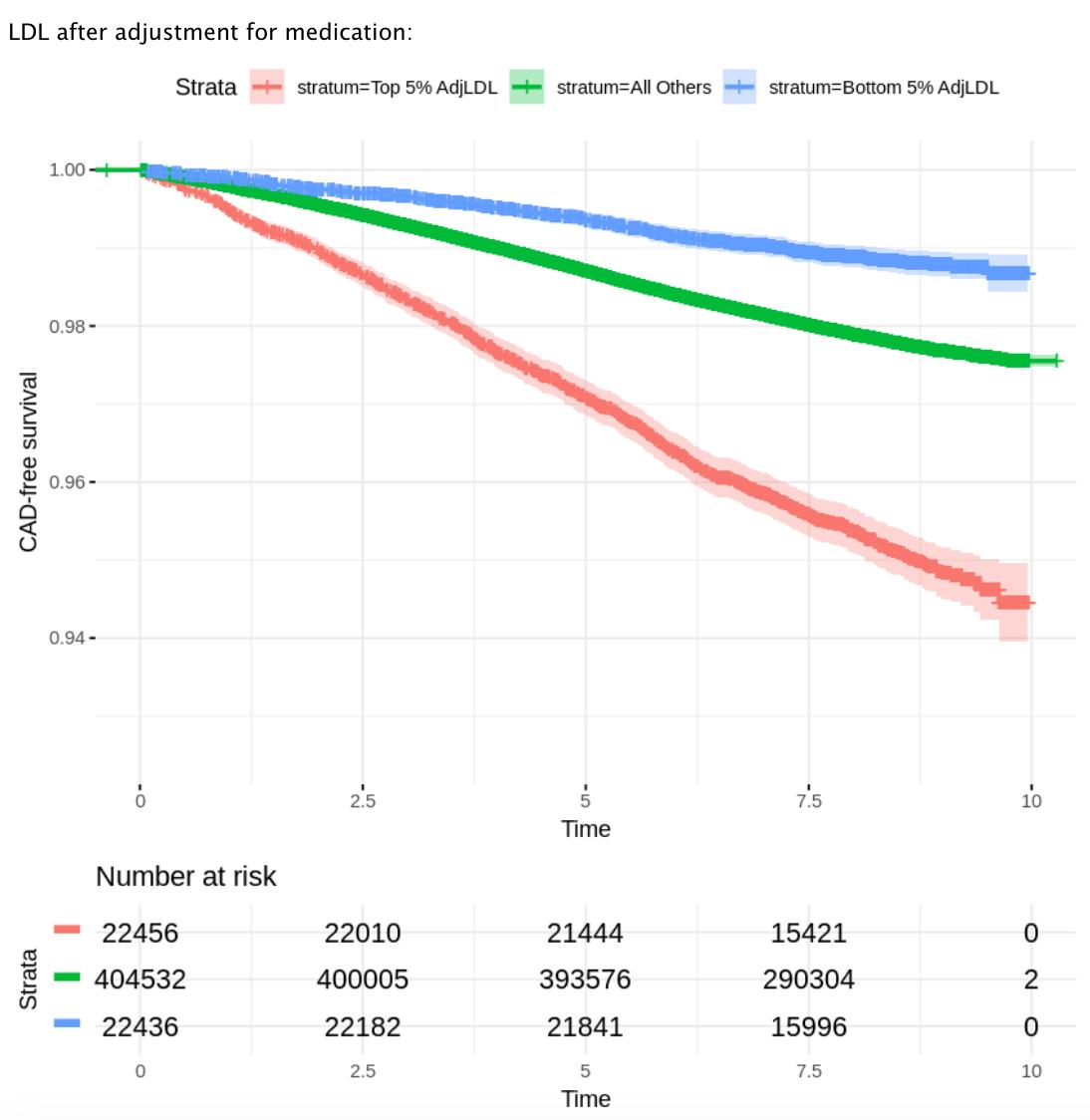
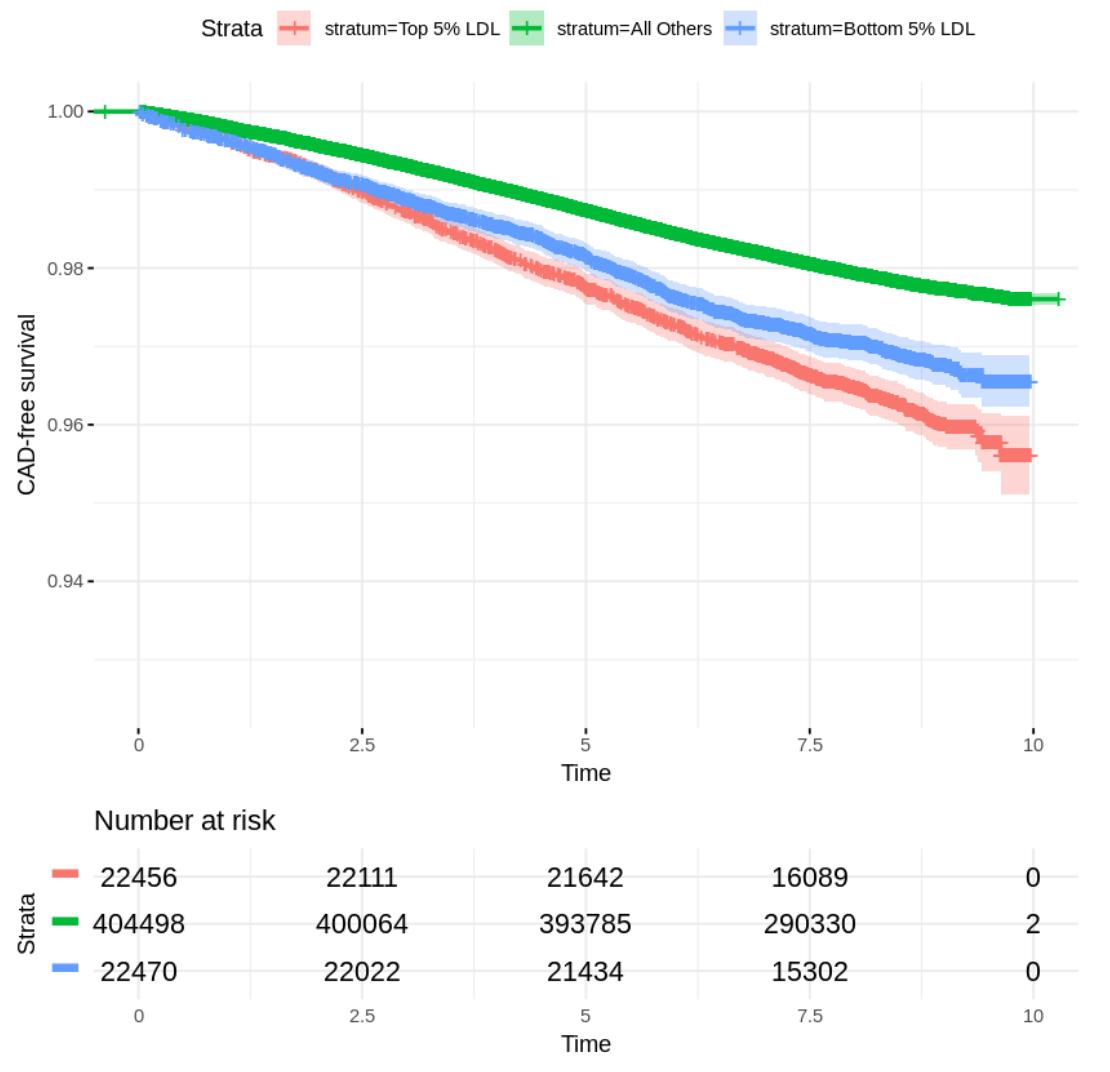 Answer: confounding based on LDL-lowering treatment at entry into @uk_biobank
Answer: confounding based on LDL-lowering treatment at entry into @uk_biobank