
Health Economist and Associate Professor @Yale @YaleSPH @YaleEconomics @YaleTobinCenter @nberpubs
How to get URL link on X (Twitter) App


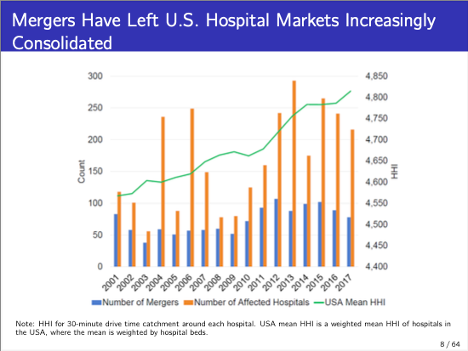
https://twitter.com/AEAjournals/status/1783212077768732746From 2002 to 2020, there were over 1,000 hospital mergers and the US. During that period, the @ftc only took action against 13 🏥 deals. Our paper asks if the @FTC has historically done enough.


https://twitter.com/_melaevans/status/1804890329352401165TLDR Summary: Employer-sponsored health insurance creates a link between what happens in health care markets and what happens in labor markets. We show that when hospitals merge and prices go up, low- and middle-class workers lose their job. Along with job losses, we see a loss in tax revenue collected by the federal government.


https://twitter.com/AEAjournals/status/1783212077768732746We posted the paper @YaleTobinCenter webpage and have also included a 1-pager on the paper tobin.yale.edu/sites/default/…

https://twitter.com/jasondebruyn/status/1542888035070656512Often, this academic work is hard to access & written opaquely. There's an intuitive appeal of price transparency, but unfortunately, the evidence (and theory) doesn't suggest we should be optimistic. Hopefully, this thread helps highlight what research says on these issues
https://twitter.com/Freakonomics/status/1380115563125563393ESRD is on the rise in the US. In part, this is driven by the rise in diabetes in the US, which leads to ESRD. So, poor health management --> downstream problems.



https://twitter.com/FrankPallone/status/1337560369678708736The bipartisan proposal includes a hold harmless provision that requires patients, if treated by an out-of-network doctor at an in-network facility, only be subject to in-network cost-sharing & no balance billing (eg MDs/staffing companies can't go after them for charges). 2/n
https://twitter.com/nytopinion/status/1076197835287261184The Gupta study is really good. Below is a summary and some thoughts. He notes that hospitals could respond to readmissions penalties in two ways: 1) by improving quality or 2) by changing composition of patients they admit (e.g. not admitting patients