
Burnout: a work-related constellation of signs/symptoms, often without prior psychiatric history. Marked by existential crisis, emotional exhaustion, and depersonalization. That’s academic. I described what it looks & feels like at @MassGeneralNews @acgme @TheIHI [THREAD] 

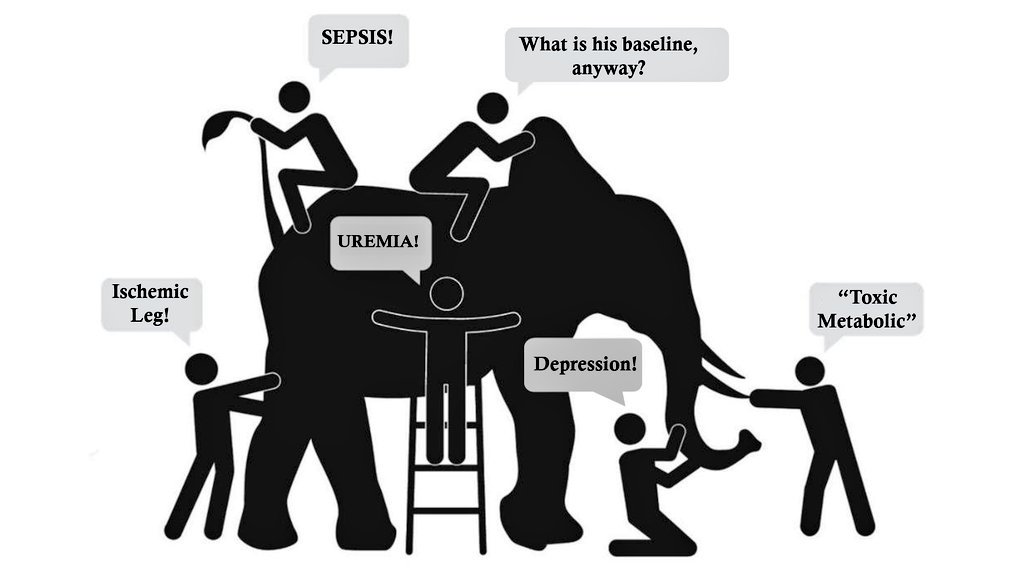
Early in intern year, I was caring for Mr. V, an elderly HD patient. 1mo earlier, he was living independently & working at HR block. Now, he was admitted with delirium. I couldn't figure out why. I couldn't fix it. Weeks went by. He floundered on the service, sicker by the day.
After 14 inpatient days, we finally diagnosed Mr. V. Months before, PCP prescribed Morphine CR- normally cleared by the kidneys, but his didn't work. It made him sleepy enough that he missed HD once, the start of a downward spiral. Perhaps an error was made that day by his PCP... 

But the real error was that morphine was still on the ACTIVE MED LIST, given 2x/day for 2 WEEKS. I was poisoning him. I fixed it & Mr. V was lucid... but it was too late. He had chest pain. I stepped out to get an EKG. When I returned to the room, I was alone. He was gone. 

This hit me hard. Really hard. I had just started as an MD and I felt singularly responsible for a medical error that killed a man.
I worried it would happen again, that I was the problem. It was the beginning of an EXISTENTIAL CRISIS- starting with the imposter syndrome.
I worried it would happen again, that I was the problem. It was the beginning of an EXISTENTIAL CRISIS- starting with the imposter syndrome.

Took a long time to shake off "I'm not good enough for this work."
... but 5 services were involved including renal & palliative, pharmacists & RNs who deal w this every day- EVERYONE missed it. A systems error led to my 'reduced sense of accomplishment,' to existential crisis.
... but 5 services were involved including renal & palliative, pharmacists & RNs who deal w this every day- EVERYONE missed it. A systems error led to my 'reduced sense of accomplishment,' to existential crisis.
What about EMOTIONAL EXHAUSTION? As an intern, @paullongMD cared for a man w osteomyelitis 2/2 IVDU. MRI showed extensive bony destruction, unclear acuity. Needed recent scan from hospital nearby to compare images. No problem, right? Paul makes the calls, sends a request... 

Gets report, no disk. Calls again, disk made, but not mailed. He sees pt daily, ashamed, asks for more time. Pt is itching to use. 5am one dark winter AM, Paul bikes to the other hospital, effortlessly gets the disk. We review images. Plan: surgery. Paul goes to patient's room... 

…only to find an empty bed. Pt eloped, never seen again. Soul crushing for intern who "moves mountains" to get things done only to fail. Repeat all year and you get EMOTIONAL EXHAUSTION. You stop trying. You CAN'T try anymore. Broken systems lead to emotional exhaustion. 

Depersonalization, now, that’s a strange word. Let me explore it with a story from the amazing & inspirational @RanaAwdish. Rana was 7mo pregnant when she presented to L&D at her hospital with excruciating abdominal pain. She is terrified and on the verge of hemorrhagic shock... 

The OB resident is at her bedside to ultrasound baby. Rana is an intensivist & ultrasonogropher, so she makes the diagnosis first. “there’s no heartbeat.” The resident, staring at the ultrasound display, says, “can you show me where you see that?"
She had just realized that her child had died in her womb- while critically ill. The resident was entirely oblivious.
Soon after, she is a patient in her own ICU (!)
Resident visits, plans to apologize... but ends up in tears, complaining about how hard the night was on him!
Soon after, she is a patient in her own ICU (!)
Resident visits, plans to apologize... but ends up in tears, complaining about how hard the night was on him!
I can imagine how he felt: ashamed. When I've felt that degree of shame, I withdraw. No one understands it, so I pull away. Relationships wither with patients, colleagues & family. Everything is replaced with cynicism-- that's DEPERSONALIZATION, a consequence of broken systems. 

So that's burnout - existential crisis, emotional exhaustion, depersonalization.
Or, to put it more simply, "the light inside is broken but I still work," (for now) - - thanks @psirides for the photo.
Or, to put it more simply, "the light inside is broken but I still work," (for now) - - thanks @psirides for the photo.

When our systems fail us, they wound us, and that wound can fester. It isn't an accident, because "every system is perfectly designed to get the results it gets” - Paul Batalden & Arthur Jones 

Burnout has an impact on everyone, not just the clinician. Patients have lower satisfaction & increased harm, especially increased nosocomial infections & medical errors (more errors w higher burnout scores) and higher mortality rates. #ptsafety nam.edu/clinicianwellb…
For more info check out the @theNAMedicine resources on wellness. More coming soon as I begin my research at the intersection of burnout and #ptsafety in the ICU! nam.edu/burnout-among-…
• • •
Missing some Tweet in this thread? You can try to
force a refresh





