Tweetorial on carcinoid tumor of the lung. I’ll add to it little by little every week 😊
#pathology #pulmpath
1/
Carcinoid tumor is the lower grade end of the spectrum of neuroendocrine tumors in the lung.
Caution: lung terminology is different from GI tract terminology
#pathology #pulmpath
1/
Carcinoid tumor is the lower grade end of the spectrum of neuroendocrine tumors in the lung.
Caution: lung terminology is different from GI tract terminology
2/
In the lung, the terminology is
✴️ Typical carcinoid tumor
✴️ Atypical carcinoid tumor
✴️ Small cell carcinoma
✴️ Large cell neuroendocrine carcinoma
We don’t terms such as “well differentiated NET” because...this is #pulmpath and we are special 😜
In the lung, the terminology is
✴️ Typical carcinoid tumor
✴️ Atypical carcinoid tumor
✴️ Small cell carcinoma
✴️ Large cell neuroendocrine carcinoma
We don’t terms such as “well differentiated NET” because...this is #pulmpath and we are special 😜
3/
Carcinoid tumors are very similar on H&E to low grade NE tumors in the GI tract or pancreas. Nesting, odd patterns, bland cytology, granular chromatin (“salt and pepper”)
Carcinoid tumors are very similar on H&E to low grade NE tumors in the GI tract or pancreas. Nesting, odd patterns, bland cytology, granular chromatin (“salt and pepper”)
https://twitter.com/smlungpathguy/status/780943116714979328?s=21
4/
✴️ Most carcinoid tumors in the lung are typical carcinoids
✳️ you can’t tell typical from atypical carcinoids on cytology or in small biopsies
✴️ In these specimens, calling them “carcinoid tumor” is fine
✳️ In resections, you can tell typical from atypical
✴️ Most carcinoid tumors in the lung are typical carcinoids
✳️ you can’t tell typical from atypical carcinoids on cytology or in small biopsies
✴️ In these specimens, calling them “carcinoid tumor” is fine
✳️ In resections, you can tell typical from atypical
5/
Criteria for typical vs. atypical carcinoid tumor:
✴️ Mitoses (2/10 HPF is the cutoff)
✳️ Necrosis (none in typical, “punctate” in atypical)
✴️ Either one of these is sufficient for the label of atypical carcinoid
Do NOT differentiate these based on atypia or mets
Criteria for typical vs. atypical carcinoid tumor:
✴️ Mitoses (2/10 HPF is the cutoff)
✳️ Necrosis (none in typical, “punctate” in atypical)
✴️ Either one of these is sufficient for the label of atypical carcinoid
Do NOT differentiate these based on atypia or mets
6/
Grossly, carcinoid tumors often look a bit yellow and tend to be located within a bronchus or adjacent to a bronchus. Post-obstructive mucus plugs are common.
However, carcinoid tumors can also occur in the periphery of the lung.
Grossly, carcinoid tumors often look a bit yellow and tend to be located within a bronchus or adjacent to a bronchus. Post-obstructive mucus plugs are common.
However, carcinoid tumors can also occur in the periphery of the lung.
https://twitter.com/smlungpathguy/status/731720827008258048?s=21
7/
One of the best reviews of neuroendocrine lung tumors was written in 2010 by my friend Dr. Natasha Rekhtman in @ArchivesPath
It’s a must-read. Here’s the link:
ncbi.nlm.nih.gov/m/pubmed/21043…

One of the best reviews of neuroendocrine lung tumors was written in 2010 by my friend Dr. Natasha Rekhtman in @ArchivesPath
It’s a must-read. Here’s the link:
ncbi.nlm.nih.gov/m/pubmed/21043…

8/
Atypical carcinoid tumors are more aggressive clinically than typical carcinoids. Both can metastasize to hilar/mediastinal nodes (even rarely to distant sites) but this is more common with atypical carcinoids. So this is why we count mitoses...
Atypical carcinoid tumors are more aggressive clinically than typical carcinoids. Both can metastasize to hilar/mediastinal nodes (even rarely to distant sites) but this is more common with atypical carcinoids. So this is why we count mitoses...
https://twitter.com/konzult_/status/817274100569804800?s=21
9/
What do typical and atypical carcinoids have in common?
✳️ Low grade cytology
✴️ Absence of extensive necrosis
✳️ Almost always positive for synaptophysin and chromogranin
✴️ Less than 10 mitoses per high power fields (usually far less!)
✳️ Treated surgically
What do typical and atypical carcinoids have in common?
✳️ Low grade cytology
✴️ Absence of extensive necrosis
✳️ Almost always positive for synaptophysin and chromogranin
✴️ Less than 10 mitoses per high power fields (usually far less!)
✳️ Treated surgically
10/
What is the #ihcpath profile of a typical carcinoid tumor?
Synaptophysin +
Chromogranin +
CD56 +
Cytokeratin + (try CAM5.2 if AE1/AE3 is neg)
TTF-1 weakly + or neg
p40 neg
Do you need to do #ihcpath in every case? No, but I get synaptophysin and chromogranin in most 😅
What is the #ihcpath profile of a typical carcinoid tumor?
Synaptophysin +
Chromogranin +
CD56 +
Cytokeratin + (try CAM5.2 if AE1/AE3 is neg)
TTF-1 weakly + or neg
p40 neg
Do you need to do #ihcpath in every case? No, but I get synaptophysin and chromogranin in most 😅
11/
What else can look like typical carcinoid tumor in the lung?
✳️ Glomus tumor
✳️ Sclerosing pneumocytoma
Both are negative for NE markers
✳️ Small cell carcinoma
Here you need morphology!pulmonarypath.org/cotm/2017/sep/…
pulmonarypath.org/cotm/2017/jul/…
ncbi.nlm.nih.gov/m/pubmed/15644…
What else can look like typical carcinoid tumor in the lung?
✳️ Glomus tumor
✳️ Sclerosing pneumocytoma
Both are negative for NE markers
✳️ Small cell carcinoma
Here you need morphology!pulmonarypath.org/cotm/2017/sep/…
pulmonarypath.org/cotm/2017/jul/…
ncbi.nlm.nih.gov/m/pubmed/15644…
12/
Another tumor that many worry about but shouldn’t: paraganglioma
✅ Yes, they can look like carcinoid tumors
✅ But primary paraganglioma of the lung is vanishingly rare. Carcinoid is common. When your hear hoofbeats, think 🐎not 🦓
✅ if in doubt, get a pankeratin
Another tumor that many worry about but shouldn’t: paraganglioma
✅ Yes, they can look like carcinoid tumors
✅ But primary paraganglioma of the lung is vanishingly rare. Carcinoid is common. When your hear hoofbeats, think 🐎not 🦓
✅ if in doubt, get a pankeratin
13/
Back to atypical carcinoids. Since punctuate necrosis is such a key criterion, you should know what it looks like. It can be very focal and easy to miss. It usually contains necrotic nuclei, kind of like a florid form of apoptosis
@chriszioga @pathnoob



Back to atypical carcinoids. Since punctuate necrosis is such a key criterion, you should know what it looks like. It can be very focal and easy to miss. It usually contains necrotic nuclei, kind of like a florid form of apoptosis
@chriszioga @pathnoob



14/
What is the prognostic difference between typical and atypical carcinoid tumors? Per WHO:
5y survival 90% for typical carcinoid tumor, 60% for atypical carcinoid tumor
Remember: both can metastasize to nodes, although more with atypical
Data from our center are similar:



What is the prognostic difference between typical and atypical carcinoid tumors? Per WHO:
5y survival 90% for typical carcinoid tumor, 60% for atypical carcinoid tumor
Remember: both can metastasize to nodes, although more with atypical
Data from our center are similar:



15/
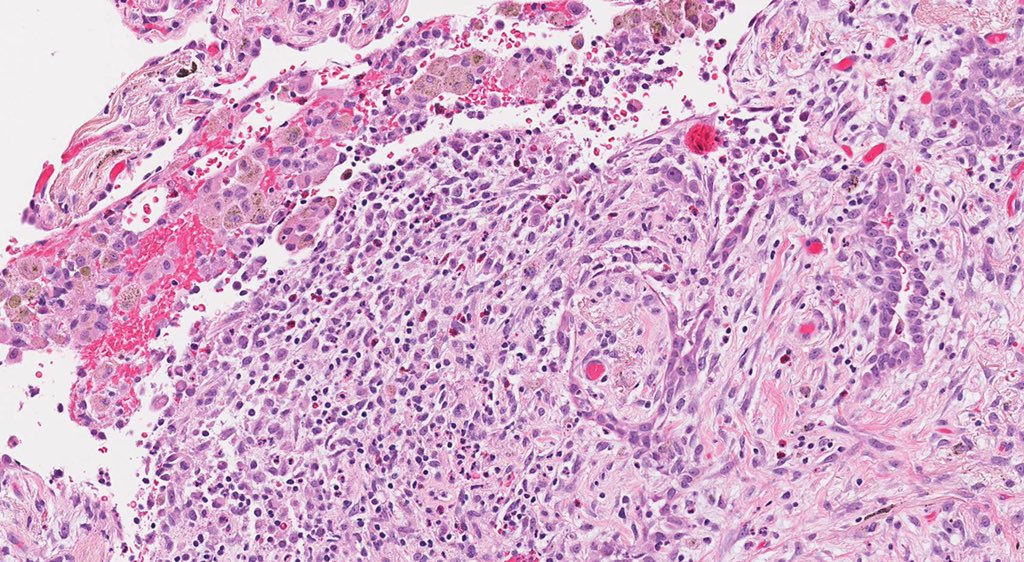
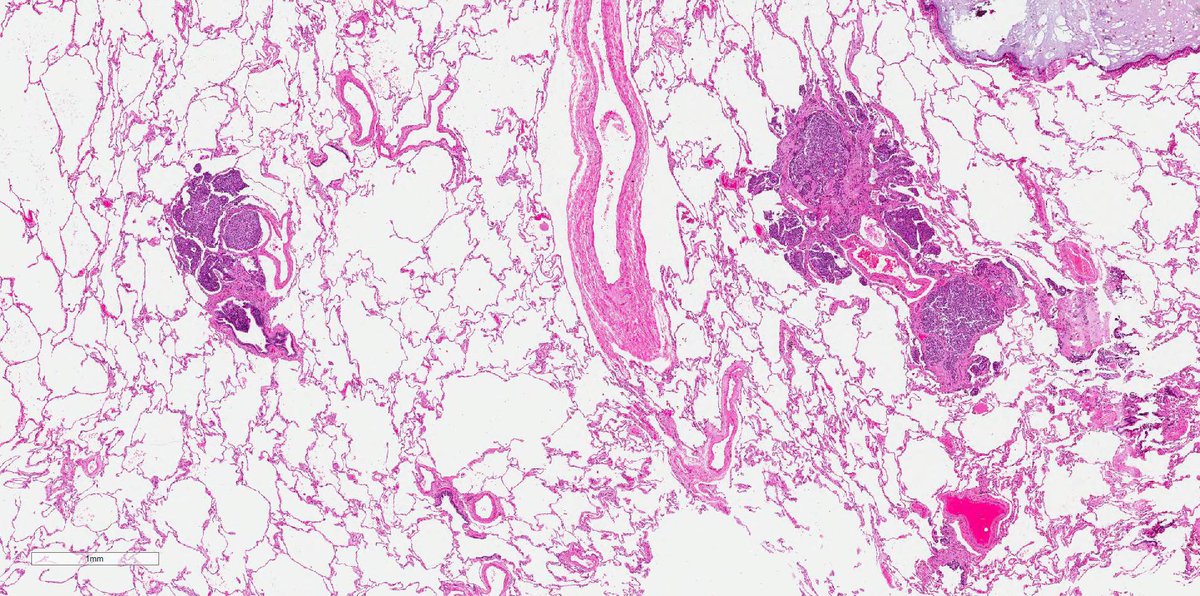
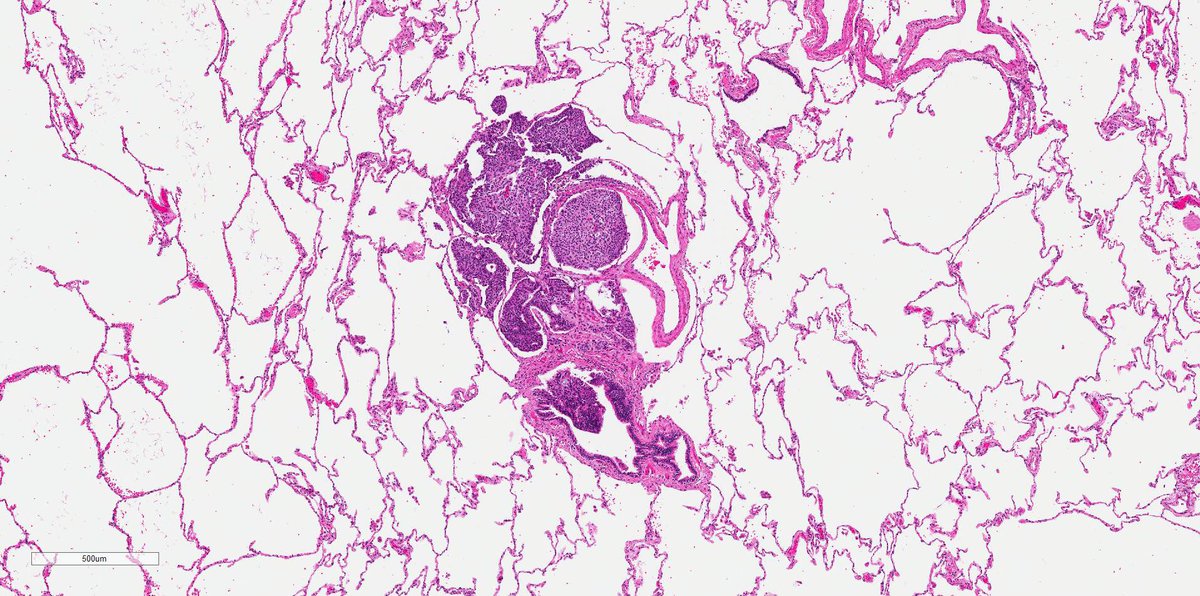
Here’s an example of a lymph node metastasis from an atypical carcinoid tumor. Nodal involvement is a significant adverse prognostic factor.
References: PMID 14698535 and 11296182
@virenkaul @leticiakawano
Here’s an example of a lymph node metastasis from an atypical carcinoid tumor. Nodal involvement is a significant adverse prognostic factor.
References: PMID 14698535 and 11296182
@virenkaul @leticiakawano

Sorry for typo: “punctate”
16/
Now let’s address baby carcinoids also known as “carcinoid tumorlets”. Defined by an arbitrary size cutoff of 5mm, these are identical to carcinoid tumors except they are very tiny and completely benign
They are invariably located in the walls of bronchioles.
Now let’s address baby carcinoids also known as “carcinoid tumorlets”. Defined by an arbitrary size cutoff of 5mm, these are identical to carcinoid tumors except they are very tiny and completely benign
They are invariably located in the walls of bronchioles.
17/
As expected, carcinoid tumorlets are positive for synaptophysin, chromogranin and the nuclear neuroendocrine marker INSM1 (we were the first to report this).
The nuclei look neuroendocrine. No mitoses. No necrosis.
They are often seen in context of small airway disease
As expected, carcinoid tumorlets are positive for synaptophysin, chromogranin and the nuclear neuroendocrine marker INSM1 (we were the first to report this).
The nuclei look neuroendocrine. No mitoses. No necrosis.
They are often seen in context of small airway disease

18/
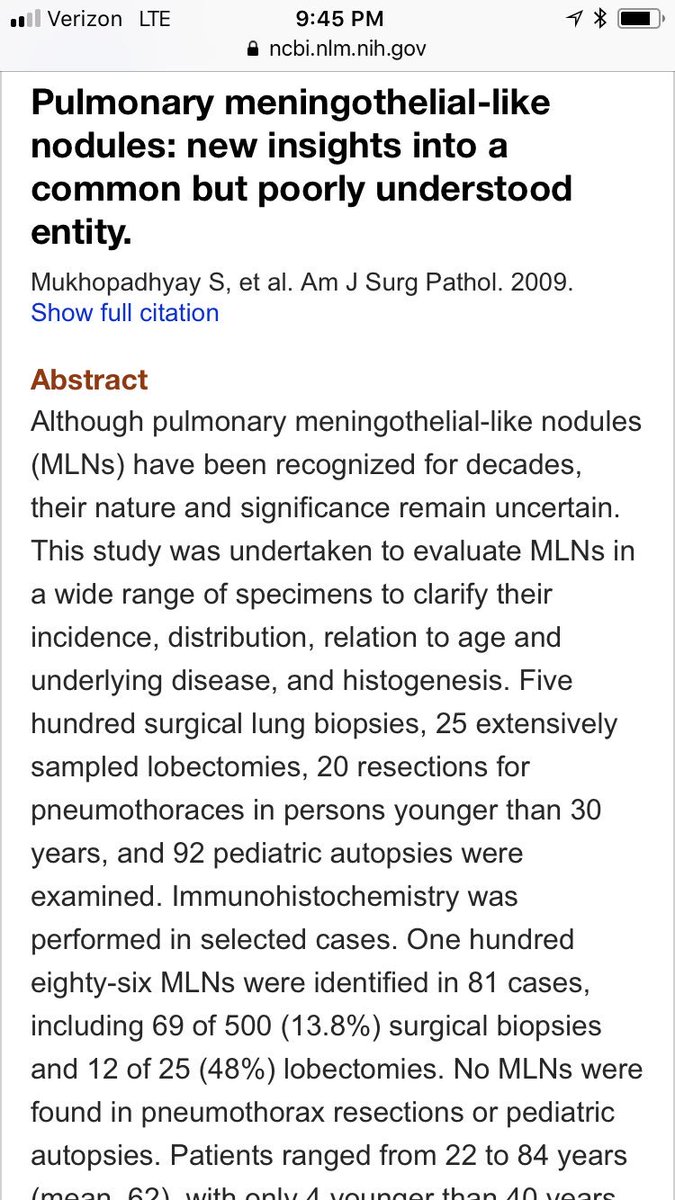
Carcinoid tumorlets are commonly confused with meningothelial-like nodules. The latter are NOT neuroendocrine but instead resemble meningeal cells. They are positive for EMA, PR, vimentin (🙄) and CD56. We were the first to report CD56 in these lesions, a pitfall


Carcinoid tumorlets are commonly confused with meningothelial-like nodules. The latter are NOT neuroendocrine but instead resemble meningeal cells. They are positive for EMA, PR, vimentin (🙄) and CD56. We were the first to report CD56 in these lesions, a pitfall

19/
More about meningothelial-like nodules here. Remember: NOT tumorlets & NOT neuroendocrine
Follow the thread to learn about DIPNECH, a very controversial entity. It stands for “diffuse idiopathic pulmonary neuroendocrine cell hyperplasia”
More about meningothelial-like nodules here. Remember: NOT tumorlets & NOT neuroendocrine
Follow the thread to learn about DIPNECH, a very controversial entity. It stands for “diffuse idiopathic pulmonary neuroendocrine cell hyperplasia”
https://twitter.com/smlungpathguy/status/869614926905704449?s=21
20/
Most would agree that the term DIPNECH is appropriate if:
✅ innumerable tiny bilateral lung nodules
+
✅ pathology: numerous tumorlets and neuroendocrine “hyperplasia” undermining bronchiolar epithelium
+
✅ no inflammation or scarring
+
✅ obstructive PFTs
Most would agree that the term DIPNECH is appropriate if:
✅ innumerable tiny bilateral lung nodules
+
✅ pathology: numerous tumorlets and neuroendocrine “hyperplasia” undermining bronchiolar epithelium
+
✅ no inflammation or scarring
+
✅ obstructive PFTs
21/
There is no agreement on what to call lesions that don’t meet all the criteria in previous tweet. For example, multiple carcinoid tumorlets commonly occur in the background lung of carcinoid tumors. No obstructive PFTs. Is this DIPNECH? There is no agreement among experts
There is no agreement on what to call lesions that don’t meet all the criteria in previous tweet. For example, multiple carcinoid tumorlets commonly occur in the background lung of carcinoid tumors. No obstructive PFTs. Is this DIPNECH? There is no agreement among experts
22/
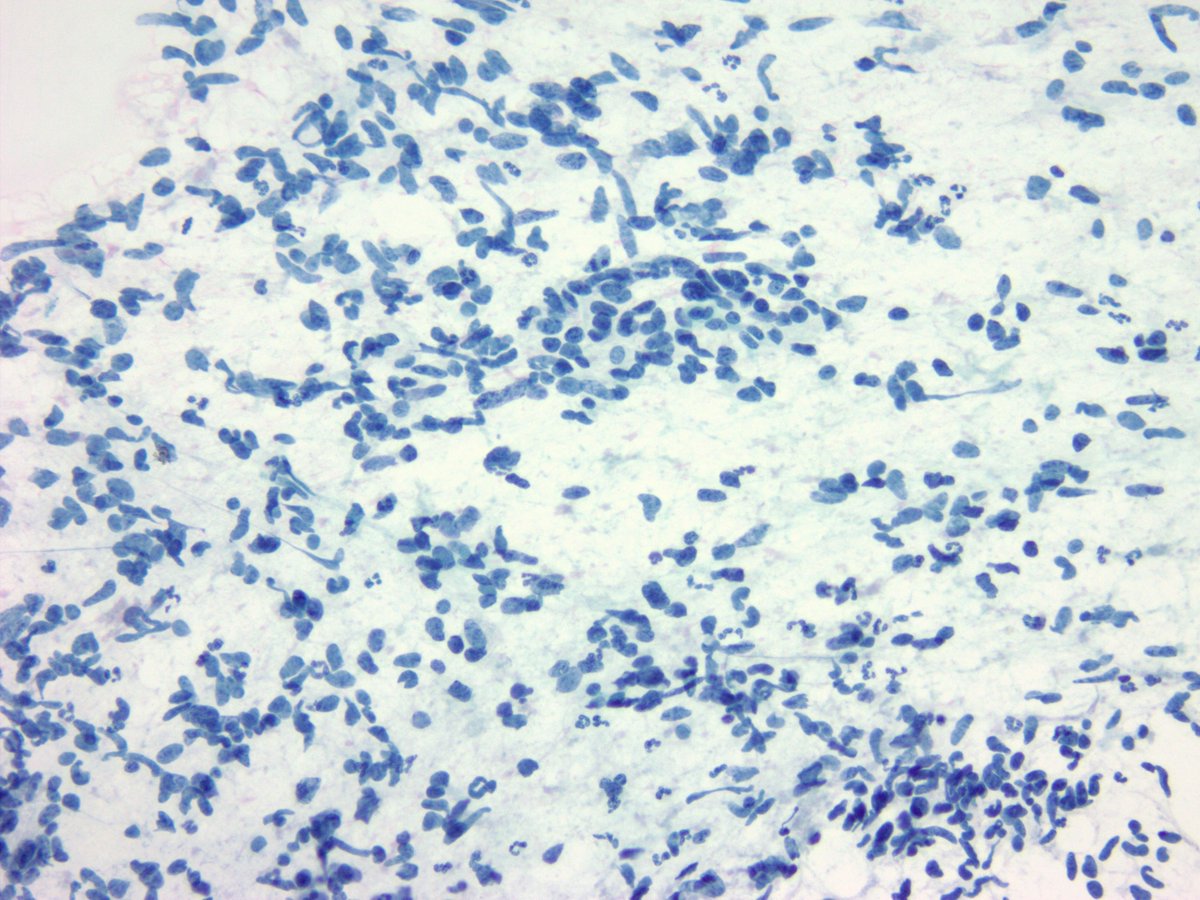
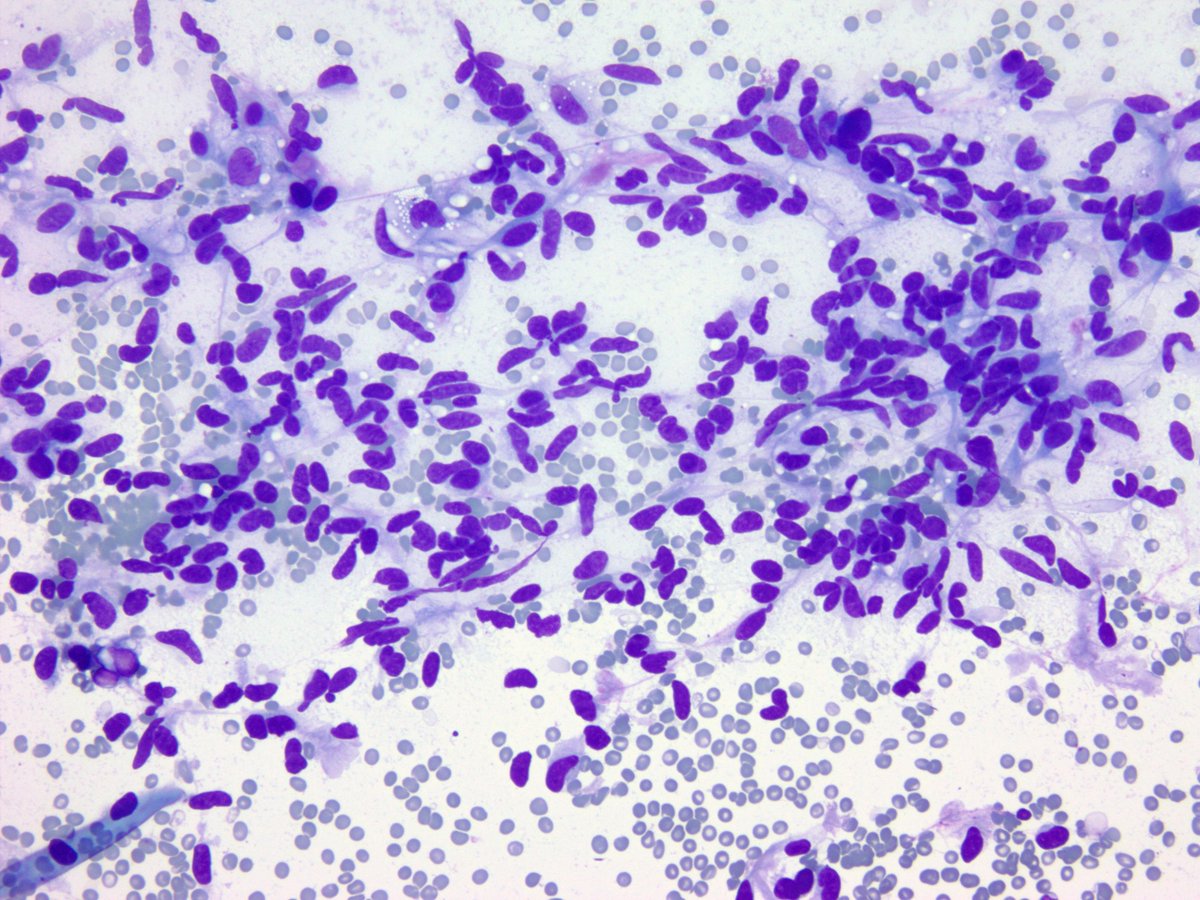
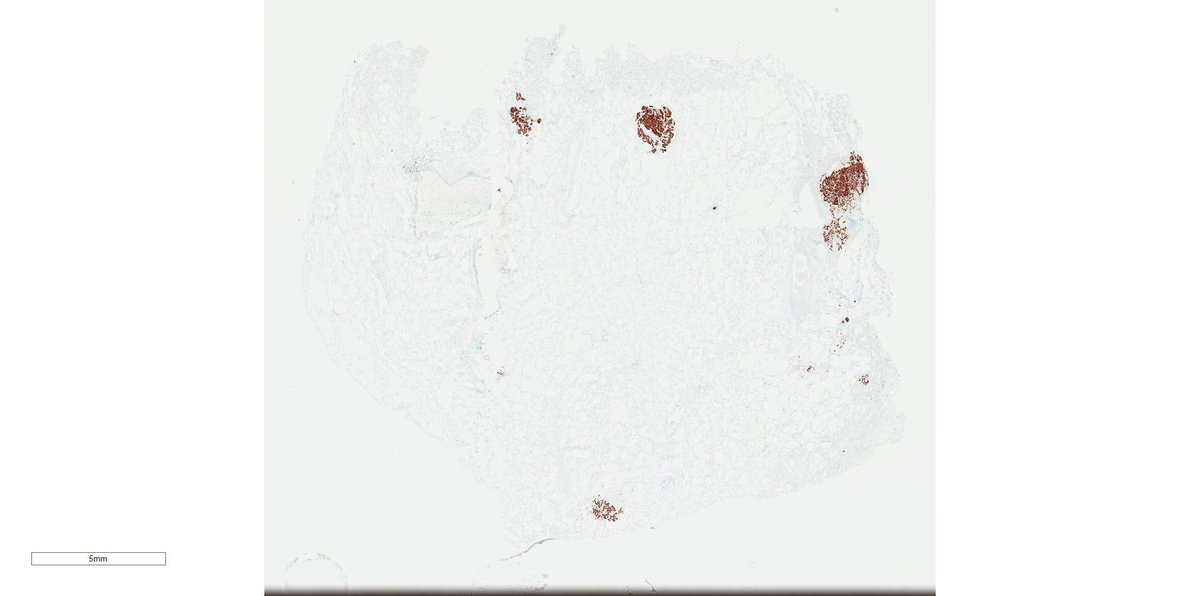
Here’s what DIPNECH looks like. Tiny neuroendocrine nodules all over the place. The #ihcpath is synaptophysin. I like the strict definition that includes no inflammation and obstructive PFTs. Anything less and I describe.




Here’s what DIPNECH looks like. Tiny neuroendocrine nodules all over the place. The #ihcpath is synaptophysin. I like the strict definition that includes no inflammation and obstructive PFTs. Anything less and I describe.

23/
Both carcinoid tumorlets and meningothelial-like nodules can be mistaken for granulomas. Especially by first year residents 😉 . You can always blame anything on a PGY1 😂
See pics for comparison at identical magnification


Both carcinoid tumorlets and meningothelial-like nodules can be mistaken for granulomas. Especially by first year residents 😉 . You can always blame anything on a PGY1 😂
See pics for comparison at identical magnification


24/
Now, some pics from the slide collection donated by @yro854 to this carcinoid #tweetorial
Chest radiograph, round shadow = carcinoid tumor. On a copy of the original, I’ve circled the areas I think show the lesion. Am I right @leticiakawano ?
#yalerosenslidecollection


Now, some pics from the slide collection donated by @yro854 to this carcinoid #tweetorial
Chest radiograph, round shadow = carcinoid tumor. On a copy of the original, I’ve circled the areas I think show the lesion. Am I right @leticiakawano ?
#yalerosenslidecollection


25/
This lovely gross pic by @yro854 shows post-obstructive bronchiectasis caused by a carcinoid tumor #pathtweetorial #grosspath
On a copy of the original, I’ve circled the areas I think show the tumor. Am I right @yro854 ?
#yalerosenslidecollection


This lovely gross pic by @yro854 shows post-obstructive bronchiectasis caused by a carcinoid tumor #pathtweetorial #grosspath
On a copy of the original, I’ve circled the areas I think show the tumor. Am I right @yro854 ?
#yalerosenslidecollection


26/
For a recent update on metastatic lung carcinoids see this #pathtweetorial 👇🏾
For a recent update on metastatic lung carcinoids see this #pathtweetorial 👇🏾
https://twitter.com/smlungpathguy/status/1116623723199467520?s=21
• • •
Missing some Tweet in this thread? You can try to
force a refresh