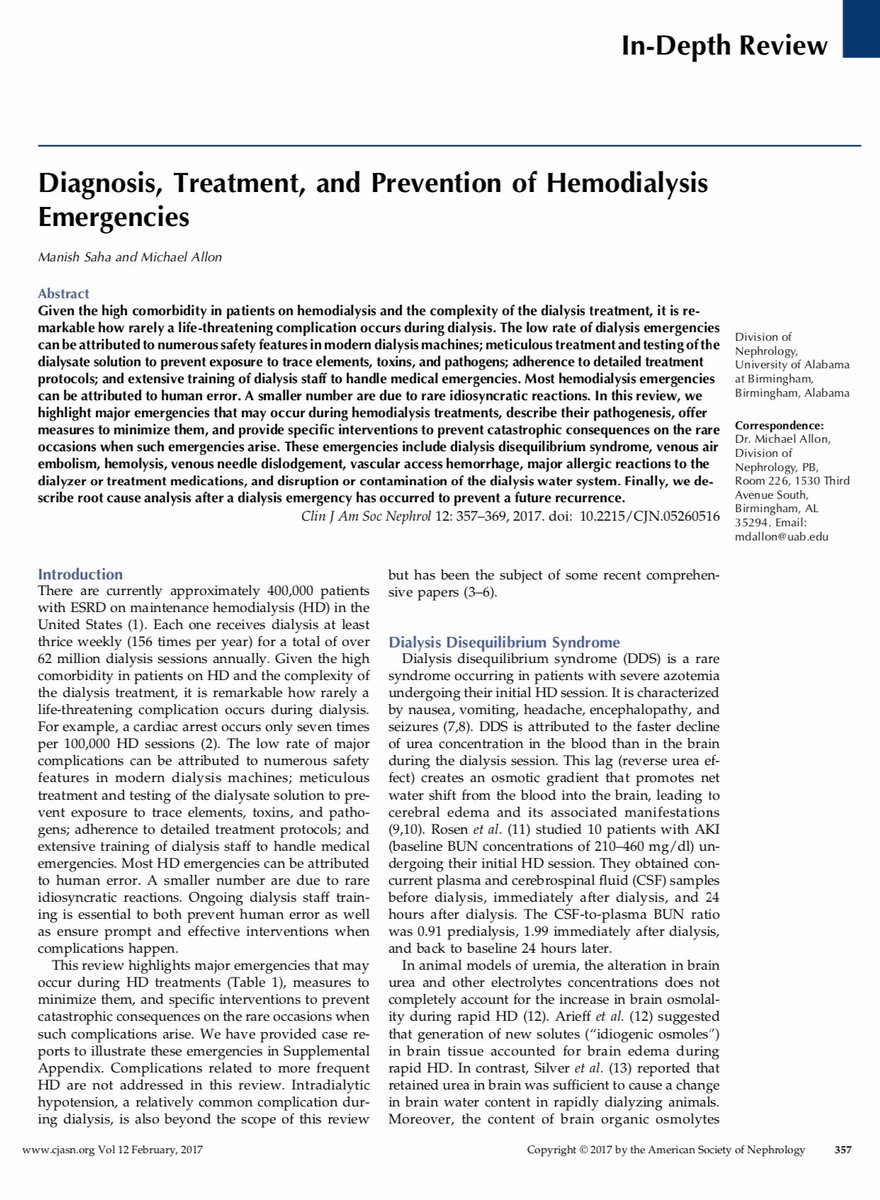
Hemodialysis 101: Complications
📌 Intradialytic Hypotension
📌 Muscle Cramps
📌 Nausea and Vomiting
📌 Pruritus
📌 Dysequilibrium Syndrome
📌 Dialyzer Reactions
📌 Hemolysis
📌 Air Embolism
#Nephpearls #DialysisDirector
📌 Intradialytic Hypotension
📌 Muscle Cramps
📌 Nausea and Vomiting
📌 Pruritus
📌 Dysequilibrium Syndrome
📌 Dialyzer Reactions
📌 Hemolysis
📌 Air Embolism
#Nephpearls #DialysisDirector

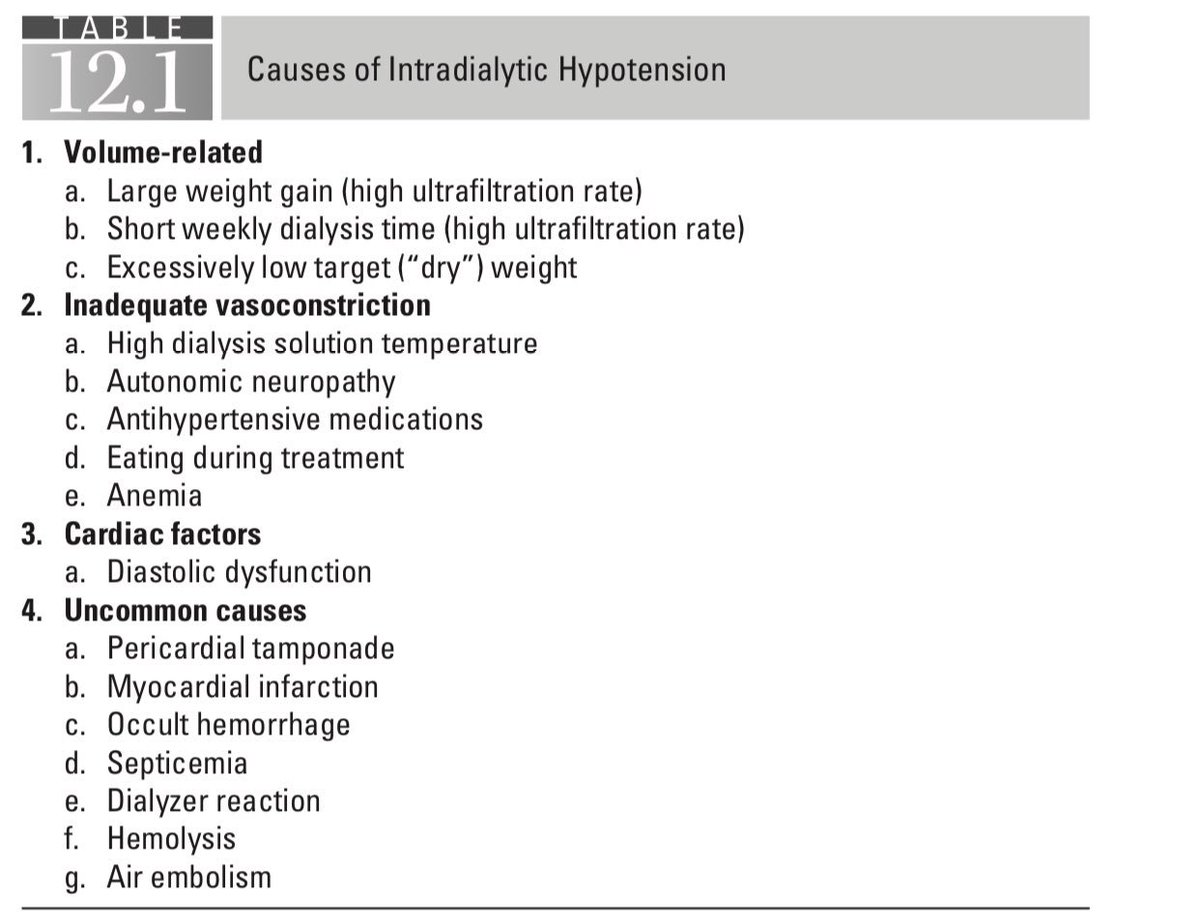
Intradialytic Hypotension (IDH): Nadir SBP < 90 👉🏼 strongest association with ⬆️ mortality
📌 Poor long-term Outcomes
📌 ⬆️ mortality
📌 Myocardial stunning
📌 Incidence is highest in those with low pre-HD BP
📌 ⬆️ risk of access thrombosis
#Nephpearls #DialysisDirector

📌 Poor long-term Outcomes
📌 ⬆️ mortality
📌 Myocardial stunning
📌 Incidence is highest in those with low pre-HD BP
📌 ⬆️ risk of access thrombosis
#Nephpearls #DialysisDirector

Intradialytic Hypotension (IDH): Strategies to help prevent Hypotension during dialysis #Nephpearls #DialysisDirector 

Muscle Cramps with hemodialysis
📌 More common during 1st month of dialysis
📌 More common in those with low cardiac index
📌 Consider ⬇️ Mg, ⬇️ Ca, ⬇️ K
📌 Risks: Hypotension, Hypovolemia, ⬆️ UF rate, ⬇️ Dialysate Na
#Nephpearls #DialysisDirector
👉🏼 google.com/amp/s/www.huff…
📌 More common during 1st month of dialysis
📌 More common in those with low cardiac index
📌 Consider ⬇️ Mg, ⬇️ Ca, ⬇️ K
📌 Risks: Hypotension, Hypovolemia, ⬆️ UF rate, ⬇️ Dialysate Na
#Nephpearls #DialysisDirector
👉🏼 google.com/amp/s/www.huff…

Quinine sulfate before dialysis, though effective in preventing intradialytic cramps, is now considered inadvisable because of its association with -
📌 Thrombocytopenia
📌 Hypersensitivity reactions
📌 QT prolongation
#Nephpearls #DialysisDirector
📌 Thrombocytopenia
📌 Hypersensitivity reactions
📌 QT prolongation
#Nephpearls #DialysisDirector

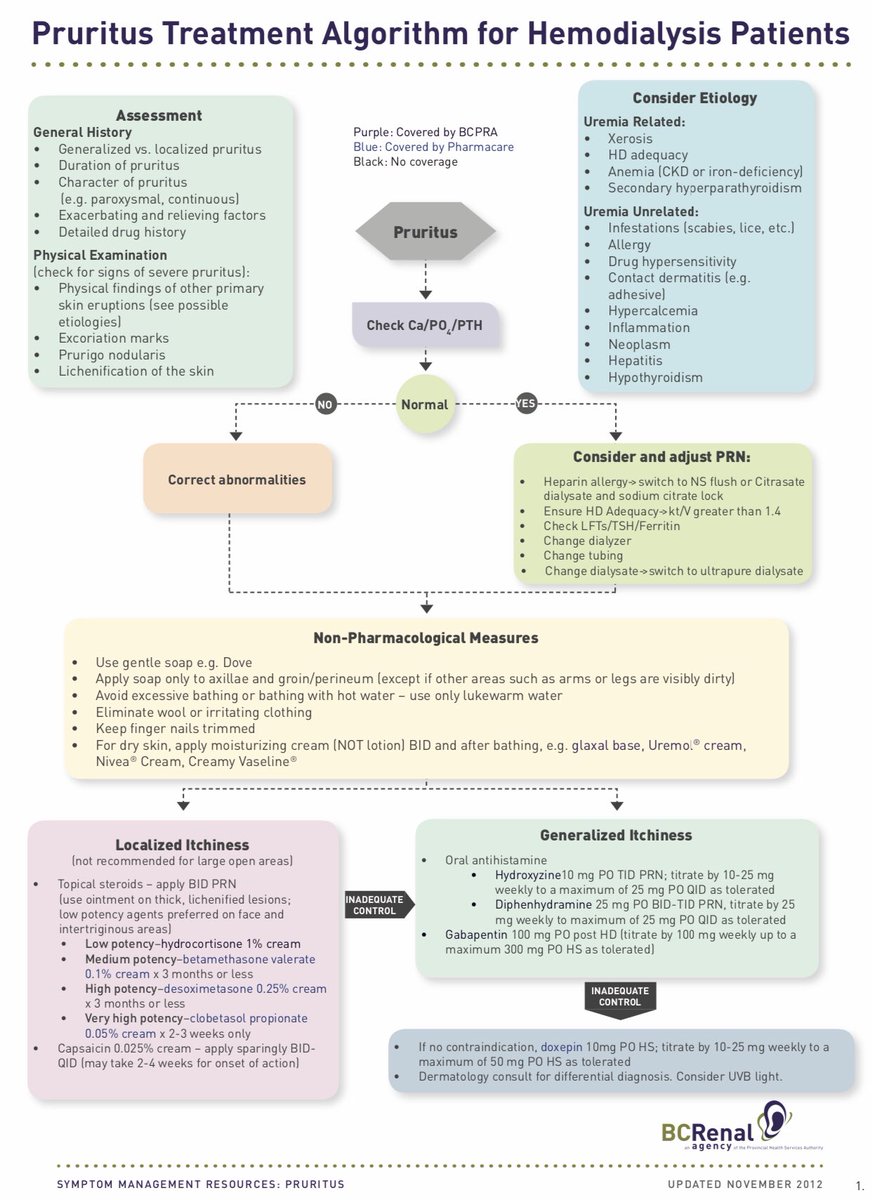
Pruritus Treatment algorithm for patients on hemodialysis from @BCRenalAgency
#Nephpearls #DialysisDirector
👉🏼 bcrenalagency.ca/resource-galle…
#Nephpearls #DialysisDirector
👉🏼 bcrenalagency.ca/resource-galle…
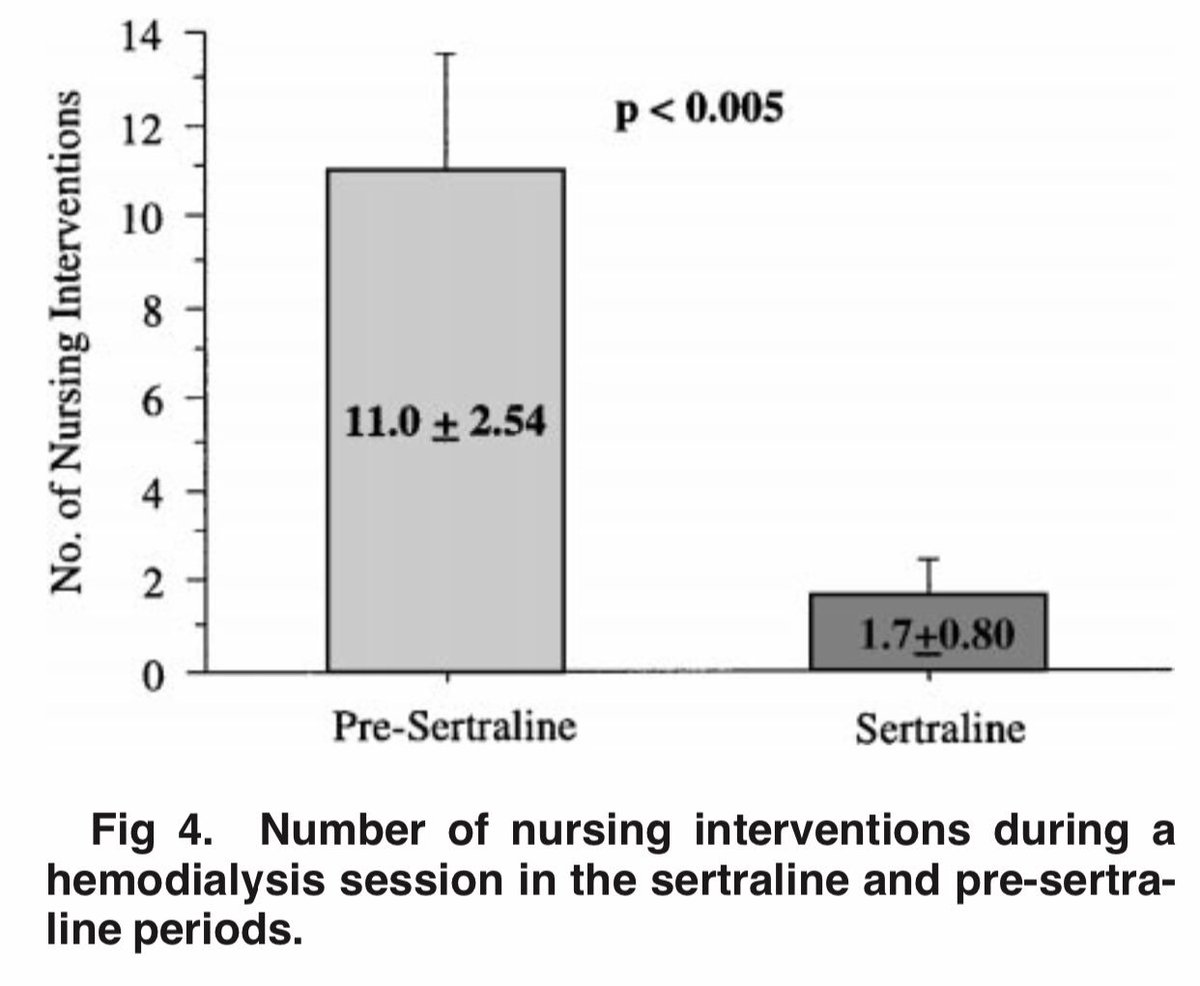
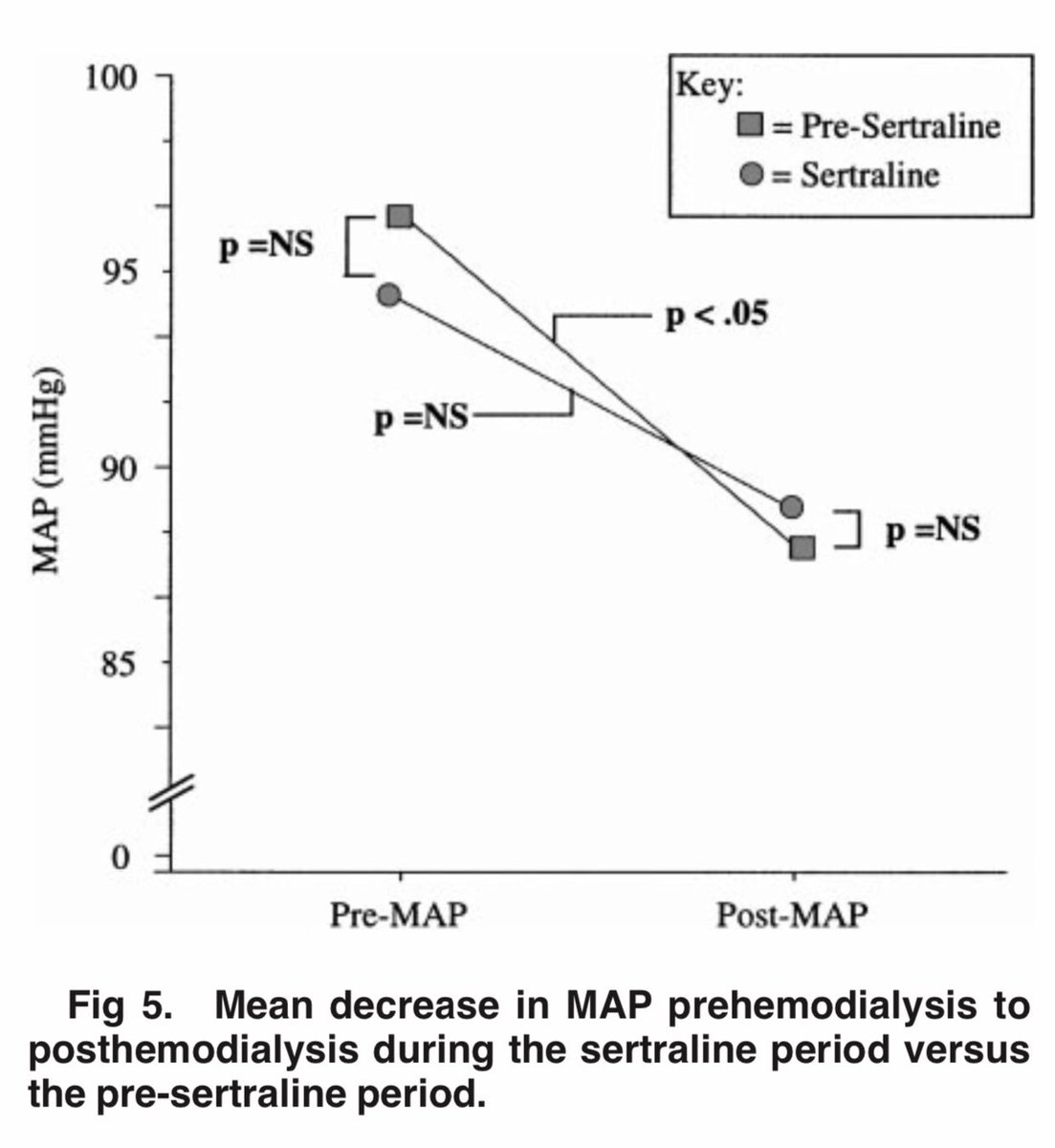
Short-term (6 weeks) use of sertraline reduces IDH in some patients
📌 “Possible” mechanism: Sertraline-induced attenuation of the paradoxical sympathetic withdrawal that may underlie IDH in some patients w/ ESKD
#Nephpearls #DialysisDirector
👉🏼 ajkd.org/article/S0272-…



📌 “Possible” mechanism: Sertraline-induced attenuation of the paradoxical sympathetic withdrawal that may underlie IDH in some patients w/ ESKD
#Nephpearls #DialysisDirector
👉🏼 ajkd.org/article/S0272-…


Therapeutic algorithm in CKD associated pruritus ca. 2013 from @Kidney_Int
#Nephpearls #DialysisDirector
👉🏼 kidney-international.org/article/S0085-…

#Nephpearls #DialysisDirector
👉🏼 kidney-international.org/article/S0085-…


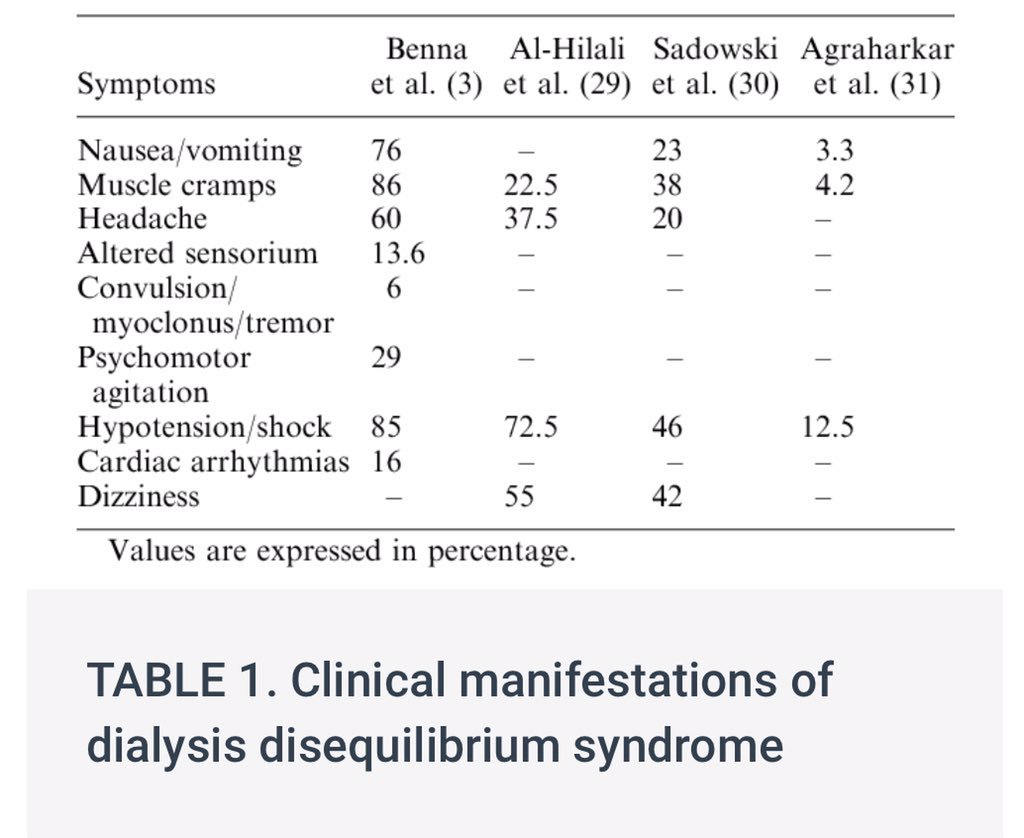
Dysequilbrium Syndrome
📌 Acute ⬆️ in brain water content
👉🏼 When plasma solute level is rapidly ⬇️ during HD, plasma becomes hypotonic relative to brain cells & water shifts from plasma into brain tissue
📌 Acute changes in CSF pH during dialysis
#Nephpearls #DialysisDirector

📌 Acute ⬆️ in brain water content
👉🏼 When plasma solute level is rapidly ⬇️ during HD, plasma becomes hypotonic relative to brain cells & water shifts from plasma into brain tissue
📌 Acute changes in CSF pH during dialysis
#Nephpearls #DialysisDirector

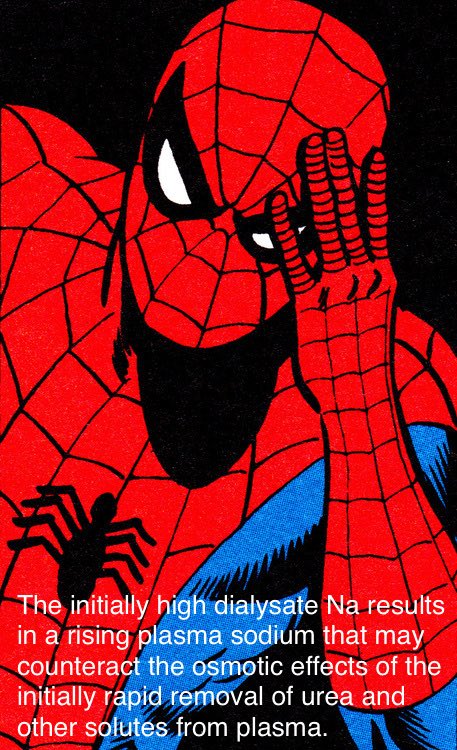
Preventing Dysequilibrium Syndrome in the setting of acute dialysis
📌 Target reduction in the BUN should initially be limited to about 40%
📌 Low Dialysate Na (more than 2–3 mmol < Serum Na) may exacerbate cerebral edema and should be avoided
#Nephpearls #DialysisDirector
📌 Target reduction in the BUN should initially be limited to about 40%
📌 Low Dialysate Na (more than 2–3 mmol < Serum Na) may exacerbate cerebral edema and should be avoided
#Nephpearls #DialysisDirector

Preventing Dysequilibrium Syndrome in the setting of chronic dialysis
📌 Use of dialysate Na at least 140 mmol
📌 Use of high dialysate Na (145–150 mmol) that declines over the course of treatment for patients has been advocated in this setting
#Nephpearls #DialysisDirector
📌 Use of dialysate Na at least 140 mmol
📌 Use of high dialysate Na (145–150 mmol) that declines over the course of treatment for patients has been advocated in this setting
#Nephpearls #DialysisDirector
Dialyzer reactions
📌 Type A - Anaplylactic
🔲 Ethylene oxide
🔲 AN69-associated
🔲 Contaminated dialysate
🔲 Reuse
🔲 Heparin
🔲 Complement fragment release
🔲 Eosinophilia
📌 Type B
🔲 Complement activation ⁉️
#Nephpearls #DialysisDirector
👉🏼 cjasn.asnjournals.org/content/clinja…

📌 Type A - Anaplylactic
🔲 Ethylene oxide
🔲 AN69-associated
🔲 Contaminated dialysate
🔲 Reuse
🔲 Heparin
🔲 Complement fragment release
🔲 Eosinophilia
📌 Type B
🔲 Complement activation ⁉️
#Nephpearls #DialysisDirector
👉🏼 cjasn.asnjournals.org/content/clinja…


Hemolysis with HD
📌 Obstruction or narrowing in the blood line, catheter, or needle - KINK⁉️
📌 Problem w/ dialysate
🔲 Overheated dialysate
🔲 Hypotonic dialysate
🔲 Contaminated dialysate (formaldehyde, bleach, Cu, etc)
#Nephpearls #DialysisDirector
👉🏼 cjasn.asnjournals.org/content/clinja…

📌 Obstruction or narrowing in the blood line, catheter, or needle - KINK⁉️
📌 Problem w/ dialysate
🔲 Overheated dialysate
🔲 Hypotonic dialysate
🔲 Contaminated dialysate (formaldehyde, bleach, Cu, etc)
#Nephpearls #DialysisDirector
👉🏼 cjasn.asnjournals.org/content/clinja…


Venous air embolism may arise from possible areas of air entry into the dialysis circuit
📌 Foam in the venous blood line
📌 If air has gone into the heart, a peculiar churning sound may be heard on auscultation
#Nephpearls #DialysisDirector
👉🏼 cjasn.asnjournals.org/content/clinja…

📌 Foam in the venous blood line
📌 If air has gone into the heart, a peculiar churning sound may be heard on auscultation
#Nephpearls #DialysisDirector
👉🏼 cjasn.asnjournals.org/content/clinja…
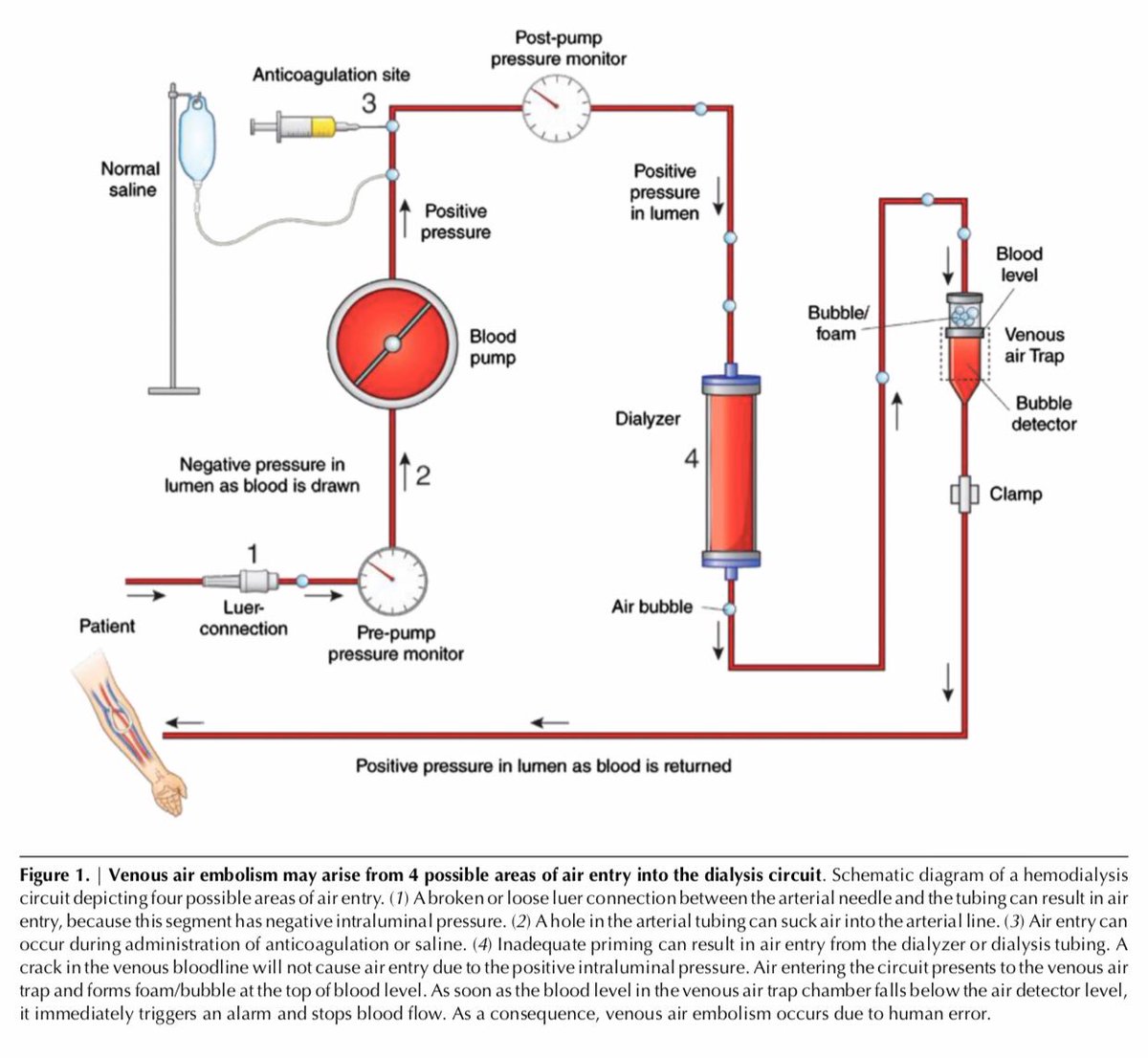
Management 🚨 of venous air embolism during HD
1️⃣ Clamp 🗜 the venous blood line & stop the blood pump‼️
2️⃣ Place patient in the recumbent position on the left side w/ the chest & head tilted downward
➡️ Cardiopulmonary support, 100% O2, etc.
#Nephpearls #DialysisDirector
1️⃣ Clamp 🗜 the venous blood line & stop the blood pump‼️
2️⃣ Place patient in the recumbent position on the left side w/ the chest & head tilted downward
➡️ Cardiopulmonary support, 100% O2, etc.
#Nephpearls #DialysisDirector

KALM-1: Efficacy and Safety of Difelikefalin in Patients Undergoing Hemodialysis with Pruritus: Results from a Phase 3 Randomized, Controlled Study
#KidneyWk #Nephpearls
👉🏼 nejm.org/doi/pdf/10.105…



#KidneyWk #Nephpearls
👉🏼 nejm.org/doi/pdf/10.105…




• • •
Missing some Tweet in this thread? You can try to
force a refresh