In case you missed it, @iamjohnoliver hosted an episode Sunday night on gender and racial bias in medicine. Here are a few of the studies on racial disparities he highlighted on the episode. 1/
https://twitter.com/LastWeekTonight/status/1163456495524167681
@iamjohnoliver In a study of patients admitted to trauma centers in PA, authors found that patients admitted to hospitals with high concentrations of blacks had a 43% higher odds of death compared with patients admitted to hospitals treating low proportions of blacks. 2/
onlinelibrary.wiley.com/doi/full/10.11…
onlinelibrary.wiley.com/doi/full/10.11…
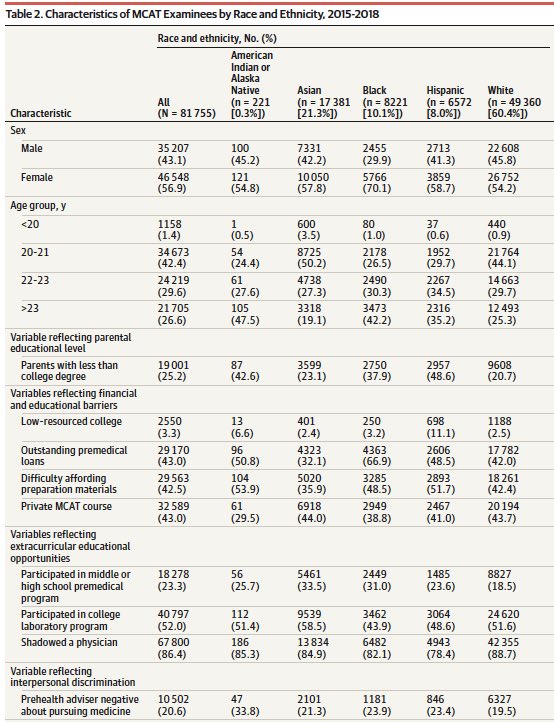
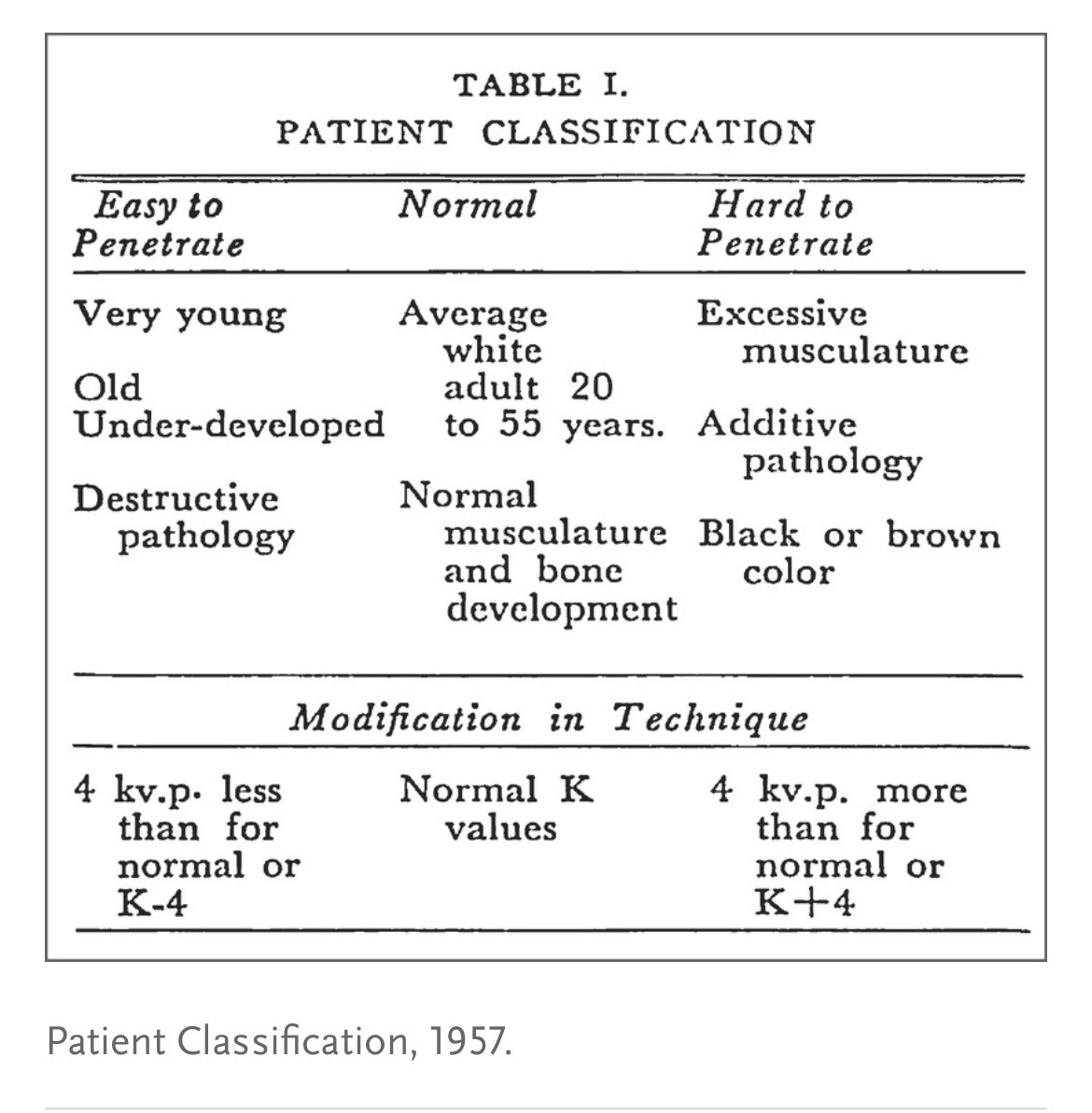
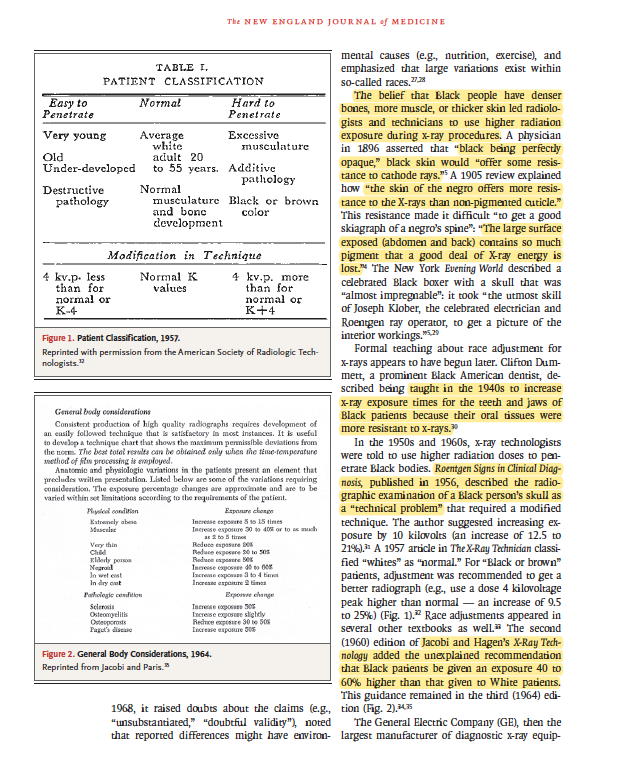
@iamjohnoliver In a well-cited 2016 paper, researchers found ~50% of medical students and residents surveyed reported at least one false belief about biological differences between blacks and whites (e.g. “black people’s skin is thicker than white people’s skin”). 3/
pnas.org/content/113/16…
pnas.org/content/113/16…
@iamjohnoliver In this systematic review, the authors reviewed 20 years of data and found black vs. white disparities in “traumatic/surgical” and "non-traumatic/nonsurgical” pain management across all several settings; black patients were less likely to be treated. 4/
academic.oup.com/painmedicine/a…
academic.oup.com/painmedicine/a…
@iamjohnoliver Finally, the show blended gender and racial disparities by sharing the hugely important work of @ByNinaMartin @propublica and so many others on maternal health disparities. cc @neel_shah @priskaneely @doccrearperry @LizHowellMD @RRHDr @Rose_L_Molina 5/5
propublica.org/series/lost-mo…
propublica.org/series/lost-mo…
• • •
Missing some Tweet in this thread? You can try to
force a refresh