
#TRAUMA: #medthread on the coagulopathic changes in severe trauma.
This is the WHY behind trauma resuscitation efforts.
#traumaanesthesia #damagecontrol #resuscitation
@UABSurgery @UAB_Anesthesia @uabmedicine 1/
This is the WHY behind trauma resuscitation efforts.
#traumaanesthesia #damagecontrol #resuscitation
@UABSurgery @UAB_Anesthesia @uabmedicine 1/

Post-trauma hemorrhage and hypotension leads to a unique physiologic derangement called Acute Traumatic Coagulopathy. Resuscitation requires management of both hemodynamics and coagulation status. 2/ 
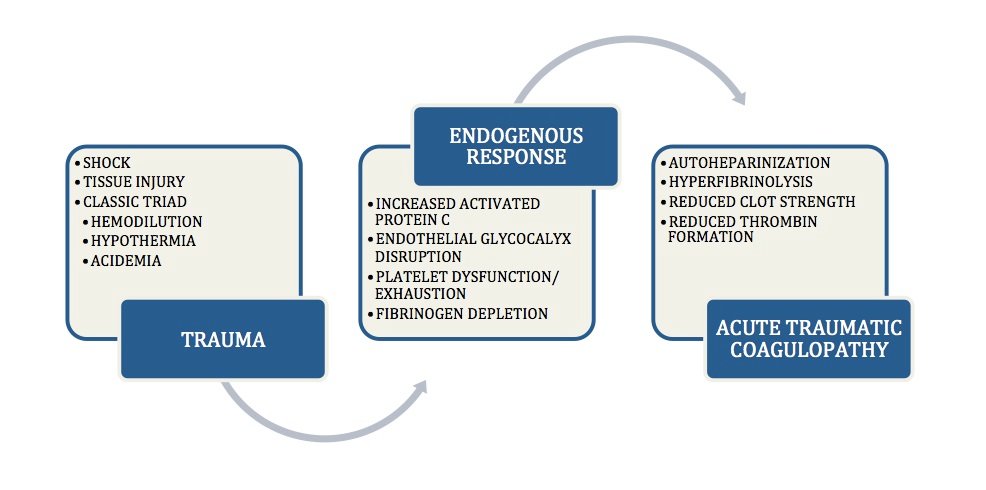
Why does this happen? If you were to simply cut your finger, your body would sense the injury and begin clot formation (platelet>factor signaling>fibrin net>more platelets). But to restore blood flow, it would need to break down that clot. 3/ 

We break down a clot through fibrinolysis (tPa stored in the glycocalyx of blood vessel walls activates plasminogen). But, we also need to slow down clot formation (activation of Protein C) and ensure the blood vessel is free flowing (heparin coating). 4/ 

Imagine massive trauma. 👉Platelets and fibrinogen go to work and are rapidly depleted. 👉Heparin and tPa is released into our system. 👉Activated protein C slows thrombin (⬇️FV and VII) formation and fails to inhibit plasminogen (⬇️PAI). =MASSIVE BLEED 5/
To make things worse. Hypothermia and acidemia from massive blood loss make platelets not work. Fibrinogen is stored in minute amounts and is rapidly depleted. Fibrin + Platelets = Clot Strength. 6/ 

This explains why we resuscitate massive traumas the way we do. (Damage Control Resuscitation) 7/
1⃣Rapidly Rewarm
2⃣Limit Crystalloids
3⃣Damage Control Surgery
4⃣Ratio Based Transfusion Early
5⃣Maintain MAP 65mmHg
6⃣Antifibrinolytics
1⃣Rapidly Rewarm
2⃣Limit Crystalloids
3⃣Damage Control Surgery
4⃣Ratio Based Transfusion Early
5⃣Maintain MAP 65mmHg
6⃣Antifibrinolytics
Rapid Rewarm every way you can. Room temp, fluids, limit surgery time. Rewarming helps coagulation.
ncbi.nlm.nih.gov/pubmed/27101496 8/
ncbi.nlm.nih.gov/pubmed/27101496 8/
Limit Crystalloid to reduce hemodilution. This does not mean eliminate, but reduce. ncbi.nlm.nih.gov/pubmed/17214989 9/ 

Damage control surgery aims to limit surgical time, control contamination, stop bleeding, stabilize fractures. Here is where you want to avoid the lethal triad. 10/ 

Early ratio based 1:1 blood transfusion + platelets + cryoprecipitate attempts to provide whole blood to rapidly bleeding patients. SWITCH to Goal-Directed hemotherapy as soon as you have labs (TEG, ROTEM). ncbi.nlm.nih.gov/pubmed/23757468 11/
Maintain MAP=65 mmHg (unless there is head injury, then aim higher 80 mmHg). If lower, give blood.
Why? reduce bleeding and clot disruption while perfusing vital organs. ncbi.nlm.nih.gov/pubmed/27015578 12/
Why? reduce bleeding and clot disruption while perfusing vital organs. ncbi.nlm.nih.gov/pubmed/27015578 12/
Tranexamic Acid is given to inhibit fibrinolysis early (within 3 hours of the trauma). Read Crash2 Trial. ncbi.nlm.nih.gov/pubmed/23477634 13/
So in trauma resuscitation we are restoring hemodynamics with RBC transfusion. These people are not deficient in phenylephrine. Don't do it. Just don't. 14/
So, how do you know if a patient needs this type of managment? 16/
Look for these 👇:
✔️BD<-6 (ischemia from blood loss)
✔️MAP < 90 mmHg (hypotension from blood loss)
✔️INR >1.5 (acute traumatic coagulopathy)
✔️Temp < 35.5 C (cold from blood loss)
Look for these 👇:
✔️BD<-6 (ischemia from blood loss)
✔️MAP < 90 mmHg (hypotension from blood loss)
✔️INR >1.5 (acute traumatic coagulopathy)
✔️Temp < 35.5 C (cold from blood loss)

A few more tips: 17/
1. Don't forget calcium chloride
2. Get labs frequently
3. 2 large bore IVs are really all you need most times
4. Assume neck injury
5. IV better than Volatile (Versed, Ketamine, Fentanyl, Rocuronium are great for traumas.)
1. Don't forget calcium chloride
2. Get labs frequently
3. 2 large bore IVs are really all you need most times
4. Assume neck injury
5. IV better than Volatile (Versed, Ketamine, Fentanyl, Rocuronium are great for traumas.)
Review Article: 18/
Acute traumatic coagulopathy: pathophysiology and resuscitation
academic.oup.com/bja/article/11…
Acute traumatic coagulopathy: pathophysiology and resuscitation
academic.oup.com/bja/article/11…
• • •
Missing some Tweet in this thread? You can try to
force a refresh









