Tried to channel my inner @tony_breu when presenting 3 hospitalist controversies yesterday:
- Normal saline vs Lactated Ringer's
- Risk of contrast-associated nephropathy?
- Routine K+ supplementation
GIANT THREAD (& poem).... #medtwitter @midwesthospmed #midwesthospmed 1/
- Normal saline vs Lactated Ringer's
- Risk of contrast-associated nephropathy?
- Routine K+ supplementation
GIANT THREAD (& poem).... #medtwitter @midwesthospmed #midwesthospmed 1/
NS vs Balanced IVF (e.g. usu LR as cheaper):
FYI LR has lactate, not lactic acid. quickly metabolized by liver to HCO3. caveat - cirrhosis pts can't metabolize as effectively so measured serum lactate can ⬆️(not harmful, not lactic acid). Can use D5W+3ampNaHCO3 if want buffer./2
FYI LR has lactate, not lactic acid. quickly metabolized by liver to HCO3. caveat - cirrhosis pts can't metabolize as effectively so measured serum lactate can ⬆️(not harmful, not lactic acid). Can use D5W+3ampNaHCO3 if want buffer./2
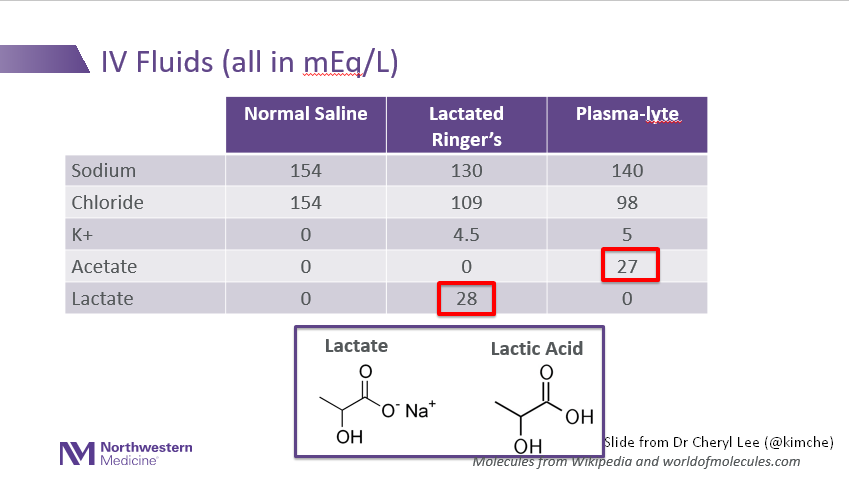
NS vs LR: the SALT-ED and SMART ICU trials:
- ⬇️rate of major adverse kidney events (persistent renal dysfxn, new dialysis, death) with LR/plasmalyte. NNT around 100 for both floor and ICU pts
- Trend towards ⬇️ inpatient mortality in ICU with LR
- avoid LR in TBI 3/
- ⬇️rate of major adverse kidney events (persistent renal dysfxn, new dialysis, death) with LR/plasmalyte. NNT around 100 for both floor and ICU pts
- Trend towards ⬇️ inpatient mortality in ICU with LR
- avoid LR in TBI 3/
Contrast:
- old studies problematic (uncontrolled, observational, high osmolar constrast, most cardiac cath)
- animal models used higher doses >> used in clinical care
- hospitalized pts have other reasons that might be to blame (sepsis, dehydration, cardiac) at same time /4
- old studies problematic (uncontrolled, observational, high osmolar constrast, most cardiac cath)
- animal models used higher doses >> used in clinical care
- hospitalized pts have other reasons that might be to blame (sepsis, dehydration, cardiac) at same time /4
Contrast nephropathy:
- Only option to study is retrospective cohort, of which there are 2 groups with differing results, poss 2/2:
-different populations, different admit dx's
-GFR<30 group smallest = sample bias
-unclear rate of IVF prophy
/5
- Only option to study is retrospective cohort, of which there are 2 groups with differing results, poss 2/2:
-different populations, different admit dx's
-GFR<30 group smallest = sample bias
-unclear rate of IVF prophy
/5

Contrast nephropathy:
-But at least we can agree that IV contrast exposure for GFR>30 doesn't appear to increase risk of AKI.
-In GFR>30, if you have AKI after a contrast study, think of other causes for AKI instead of the contrast alone
-I'd still use IVF prophy /6
-But at least we can agree that IV contrast exposure for GFR>30 doesn't appear to increase risk of AKI.
-In GFR>30, if you have AKI after a contrast study, think of other causes for AKI instead of the contrast alone
-I'd still use IVF prophy /6
Routine K+ supplementation:
We know:
- chronic hypo/hyperK+ is prognostic in heart failure (HR 2.35, HR 1.55).
- keeping normoK inpatient important in prognosis for Acute MI.
BUT
Not as clear whether chasing the daily K to 4 (versus a more liberal goal) helpful for all pts
/7
We know:
- chronic hypo/hyperK+ is prognostic in heart failure (HR 2.35, HR 1.55).
- keeping normoK inpatient important in prognosis for Acute MI.
BUT
Not as clear whether chasing the daily K to 4 (versus a more liberal goal) helpful for all pts
/7

For inpatient admissions for HF (higher risk for arrhythmias in hypoK), 2 studies saw no hazard to being hypoK during hospitalization either at 1 year or during admission.
BUT... /8
BUT... /8
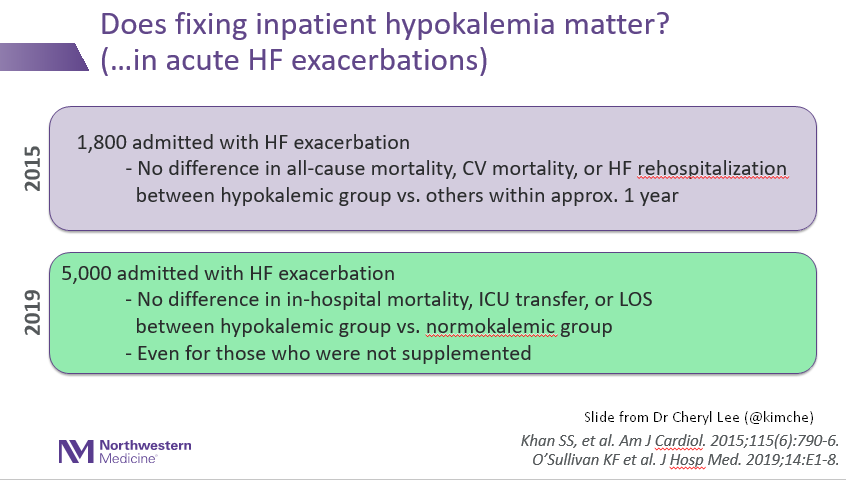
Important caveats, including:
- wide severity of illness (is there subgrp that benefits most?)
- not clear rate of beta blocker use which would imagine be protective
- providers in both studies treated pts, aiming for K>4
-2019 study determined hypoK grp on 1st 72 hrs
/9
- wide severity of illness (is there subgrp that benefits most?)
- not clear rate of beta blocker use which would imagine be protective
- providers in both studies treated pts, aiming for K>4
-2019 study determined hypoK grp on 1st 72 hrs
/9
Routine K supplementation takeaway:
- Acute MI - still stands. Keep normokalemic.
- In heart failure - chronic hypoK/hyperK is prognostic
- In Acute HF exacerbations, unclear who benefits or how aggressive to be, but maybe somewhat reassuring data....?
/10
- Acute MI - still stands. Keep normokalemic.
- In heart failure - chronic hypoK/hyperK is prognostic
- In Acute HF exacerbations, unclear who benefits or how aggressive to be, but maybe somewhat reassuring data....?
/10
Routine K supplementation takeaways:
At least, with my noncardiac pts who are at low risk for arrythmia, this gives me reassurance to avoid torturing them with K supplementation (and daily labs!) for K>3ish, esp K 3.5-5 which defines normoK in studies. /fin
At least, with my noncardiac pts who are at low risk for arrythmia, this gives me reassurance to avoid torturing them with K supplementation (and daily labs!) for K>3ish, esp K 3.5-5 which defines normoK in studies. /fin
• • •
Missing some Tweet in this thread? You can try to
force a refresh





