
Welcome to my first #tweetorial! Inspired by @NnekaUfereMD's talk @AASLDtweets to give back as a trainee
There are many things to discuss with #cirrhosis patients.
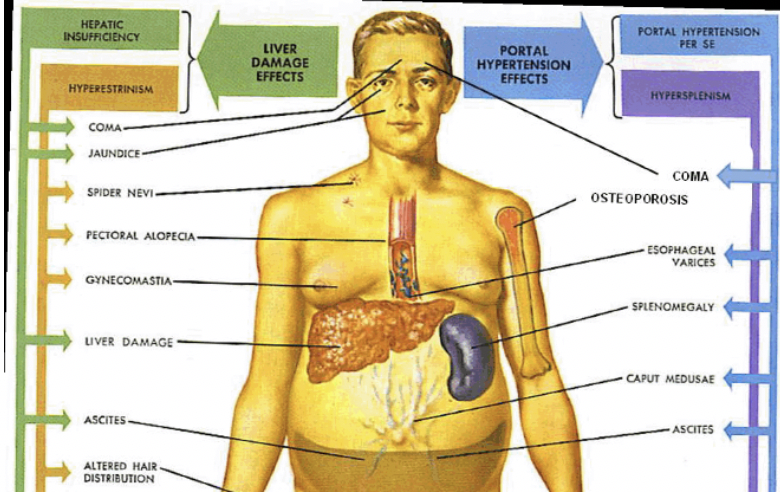
Ascites, HE, varices, HCC, transplant, GOC, rehab: the list goes on.
#Nutrition needs to be part of that routine!
There are many things to discuss with #cirrhosis patients.
Ascites, HE, varices, HCC, transplant, GOC, rehab: the list goes on.
#Nutrition needs to be part of that routine!
Why is this such a big deal?
Independent of severity of liver dysfxn, poor nutrition, sarcopenia leads to:
1⃣Lowers survival (HR 2.18)
2⃣Increased risk of infxn
3⃣Increased HE, ascites ➡️ lower QOL
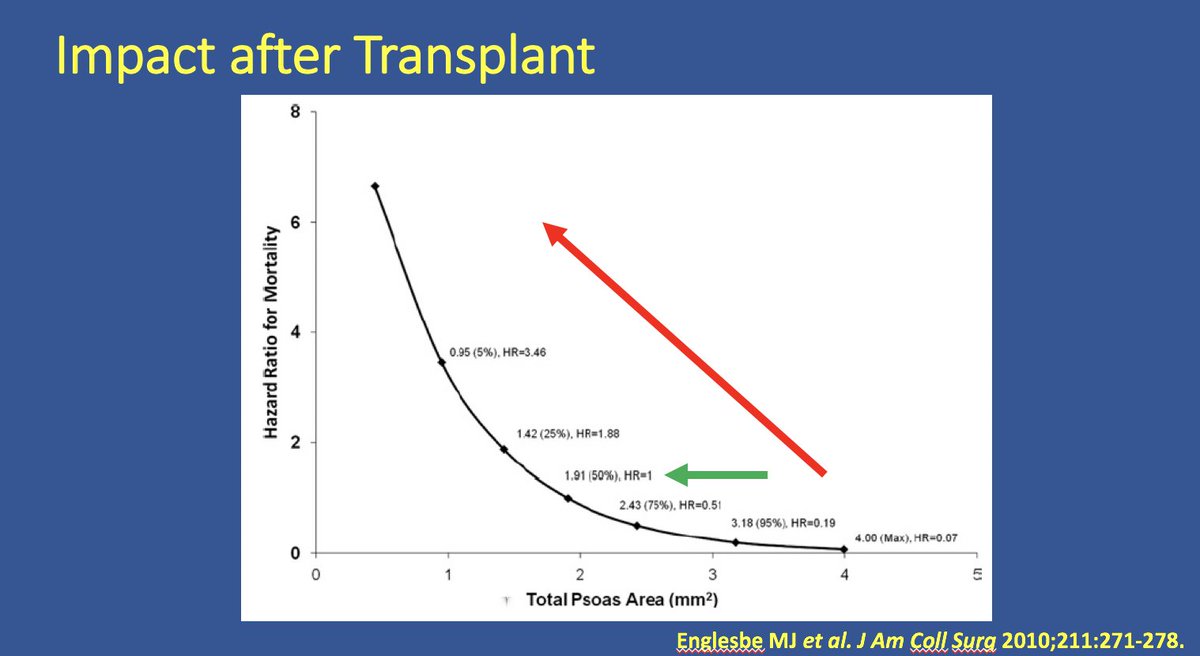
4⃣Lower survival in post-transplant setting



Independent of severity of liver dysfxn, poor nutrition, sarcopenia leads to:
1⃣Lowers survival (HR 2.18)
2⃣Increased risk of infxn
3⃣Increased HE, ascites ➡️ lower QOL
4⃣Lower survival in post-transplant setting



But what’s so special about nutrition in #cirrhosis?
For that we have to do a VERY BRIEF return to med school and the 1953 Nobel Prize winning work on energy extraction (citric acid cycle) 3/

For that we have to do a VERY BRIEF return to med school and the 1953 Nobel Prize winning work on energy extraction (citric acid cycle) 3/


Cirrhosis is a state of ACCELERATED STARVATION.
Shifts away from glucose utilization towards fatty acid use in cirrhotic patients occur very soon after meals end ➡️ less efficient energy production.
This change in metabolism is only achieved in healthy patients after 2-3 days
Shifts away from glucose utilization towards fatty acid use in cirrhotic patients occur very soon after meals end ➡️ less efficient energy production.
This change in metabolism is only achieved in healthy patients after 2-3 days

Another way to feed TCA cycle is through amino acids (PROTEIN)….specifically BRANCH-CHAIN AA in the skeletal muscle.
Liver dysfxn can deplete the BCAA in part due to their use in ammonia metabolism ➡️ muscle breakdown


Liver dysfxn can deplete the BCAA in part due to their use in ammonia metabolism ➡️ muscle breakdown



Let’s find the ways to apply this to our patients….
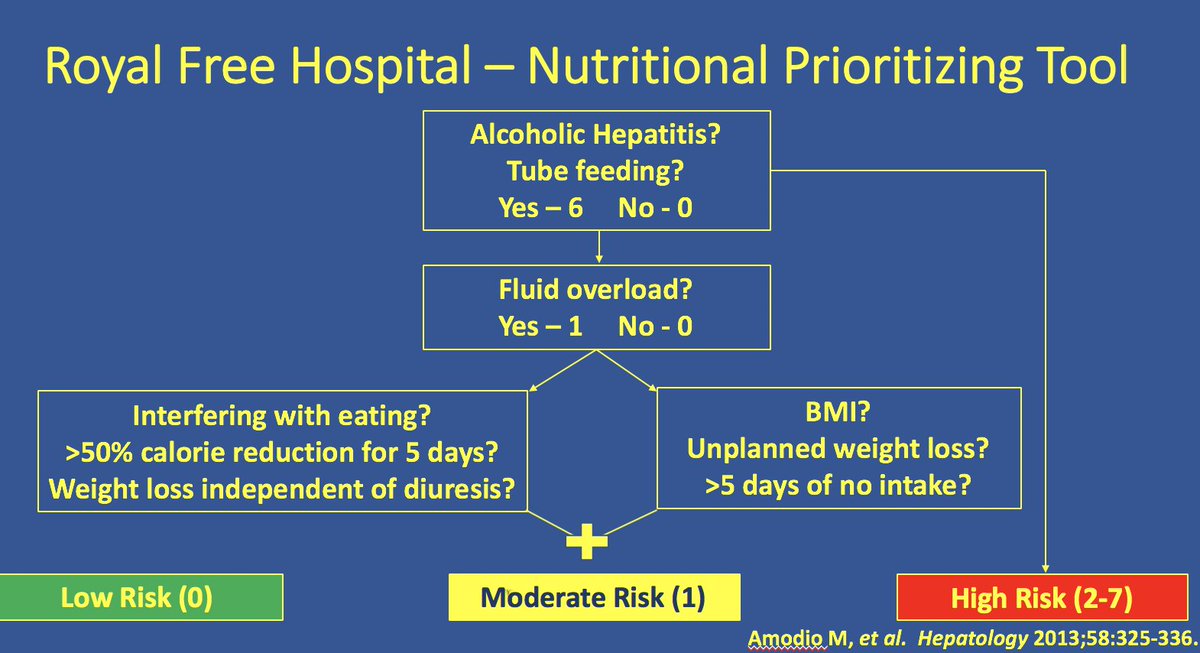
Check all cirrhotic patients with nutrition screening and high-risk patients (BMI<18.5 or CTP Class C) should be assessed with dietary assessment and check for sarcopenia
Otherwise, use a tool like RFH-NPT!

Check all cirrhotic patients with nutrition screening and high-risk patients (BMI<18.5 or CTP Class C) should be assessed with dietary assessment and check for sarcopenia
Otherwise, use a tool like RFH-NPT!

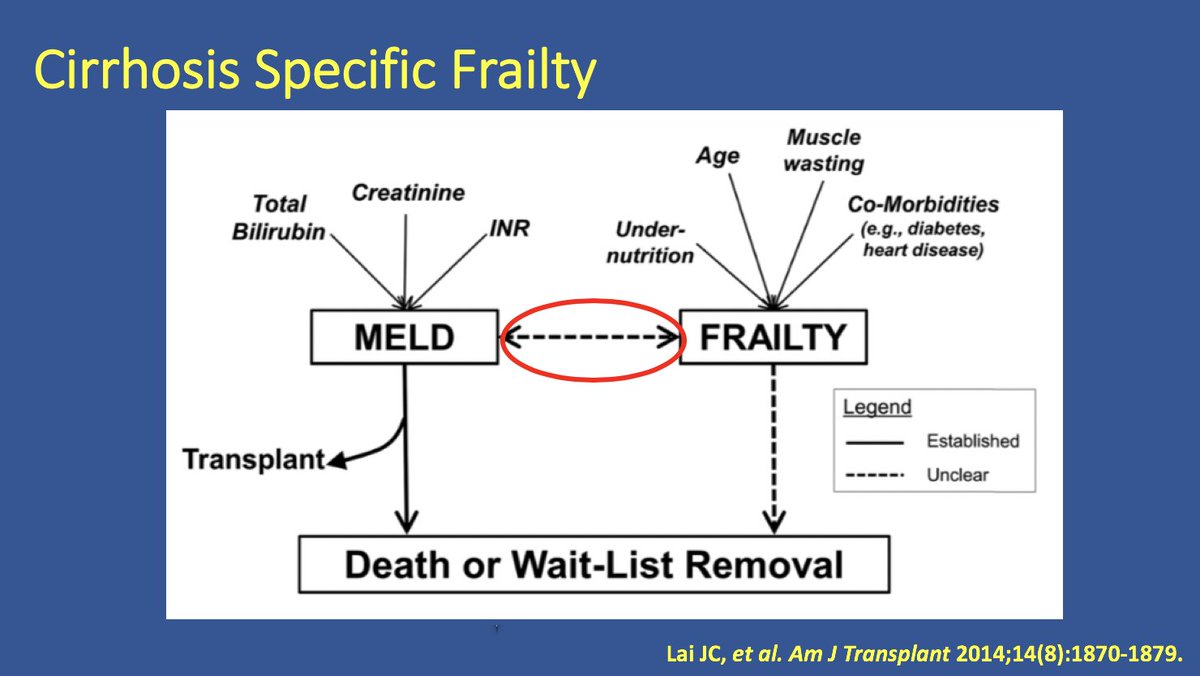
Cirrhotic patients are higher rates of frailty (physiologic vulnerability) than their chronological age would dictate.
This makes a huge difference. 7/
Ref: ncbi.nlm.nih.gov/pmc/articles/P…


This makes a huge difference. 7/
Ref: ncbi.nlm.nih.gov/pmc/articles/P…


Now what?
Core recommendations that can be applied to clinical practice:
1.Don't recommend a low protein diet (1.2-1.5 gm/kg/d)
2.Supplements throughout the day
3.Night time snack to prevent prolonged fast (#fourthmeal….just hold off on the salt)
4. Don't wait to assess.

Core recommendations that can be applied to clinical practice:
1.Don't recommend a low protein diet (1.2-1.5 gm/kg/d)
2.Supplements throughout the day
3.Night time snack to prevent prolonged fast (#fourthmeal….just hold off on the salt)
4. Don't wait to assess.


Plenty of more out there on frailty from Dr. Lai and others but for now we will close out.
Hope you enjoyed my first attempt at #livertwitter #MedEd! Feedback, additions, clarifications are WELCOME (public or DM)
Addie (the great distractor) says see you next time!
Hope you enjoyed my first attempt at #livertwitter #MedEd! Feedback, additions, clarifications are WELCOME (public or DM)
Addie (the great distractor) says see you next time!

• • •
Missing some Tweet in this thread? You can try to
force a refresh



