ISCHEMIA-CKD: Among patients w/ stable ischemic heart disease & stage 4-5 CKD (53% were on dialysis), an initial invasive strategy of cardiac cath. did not lead to a ⬇️ in clinical outcomes vs an initial conservative strategy #AHA19 #Nephpearls
👉🏼 professional.heart.org/idc/groups/aha…



👉🏼 professional.heart.org/idc/groups/aha…



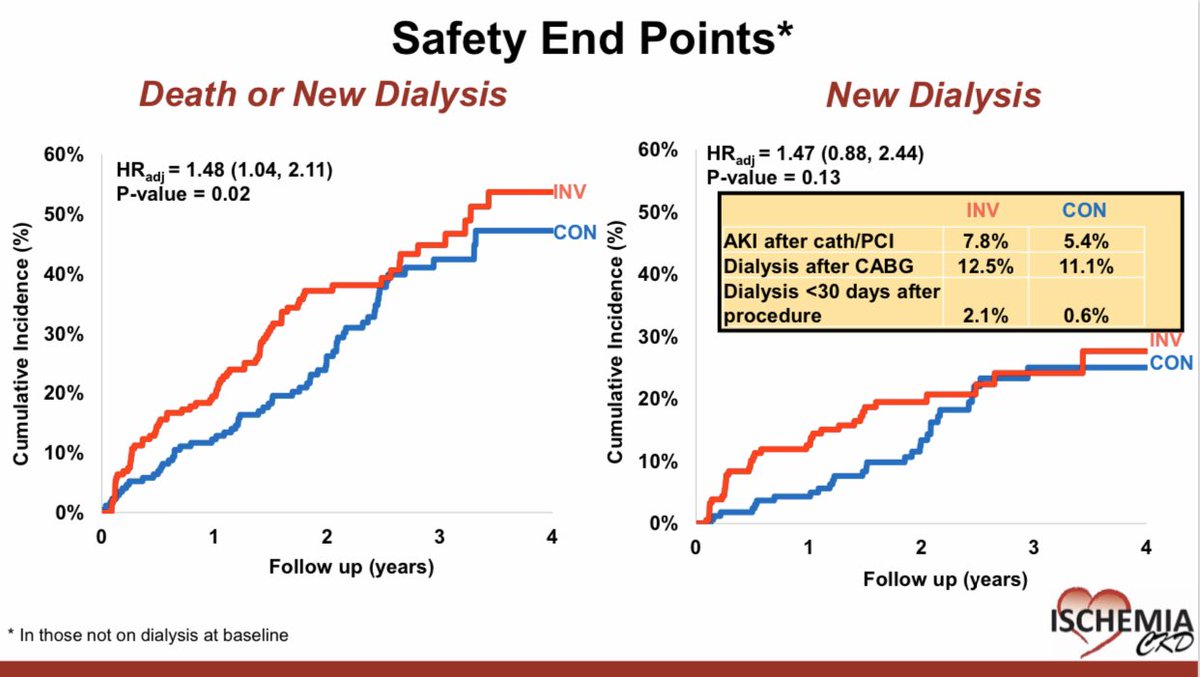
ISCHEMIA-CKD: Some caveats 🤔 to consider:
📌 The results do not apply to patients with recent ACS, unacceptable angina despite maximal medical therapy, or significant heart failure because they were excluded
#AHA19 #Nephpearls
📌 The results do not apply to patients with recent ACS, unacceptable angina despite maximal medical therapy, or significant heart failure because they were excluded
#AHA19 #Nephpearls

ISCHEMIA-CKD: Among patients with stable coronary disease, advanced CKD, and moderate or severe ischemia, an initial invasive strategy (vs initial conservative strategy), did not reduce the risk of death or nonfatal MI ca. 2020 from @NEJM #Nephpearls
👉🏼 nejm.org/doi/pdf/10.105…



👉🏼 nejm.org/doi/pdf/10.105…
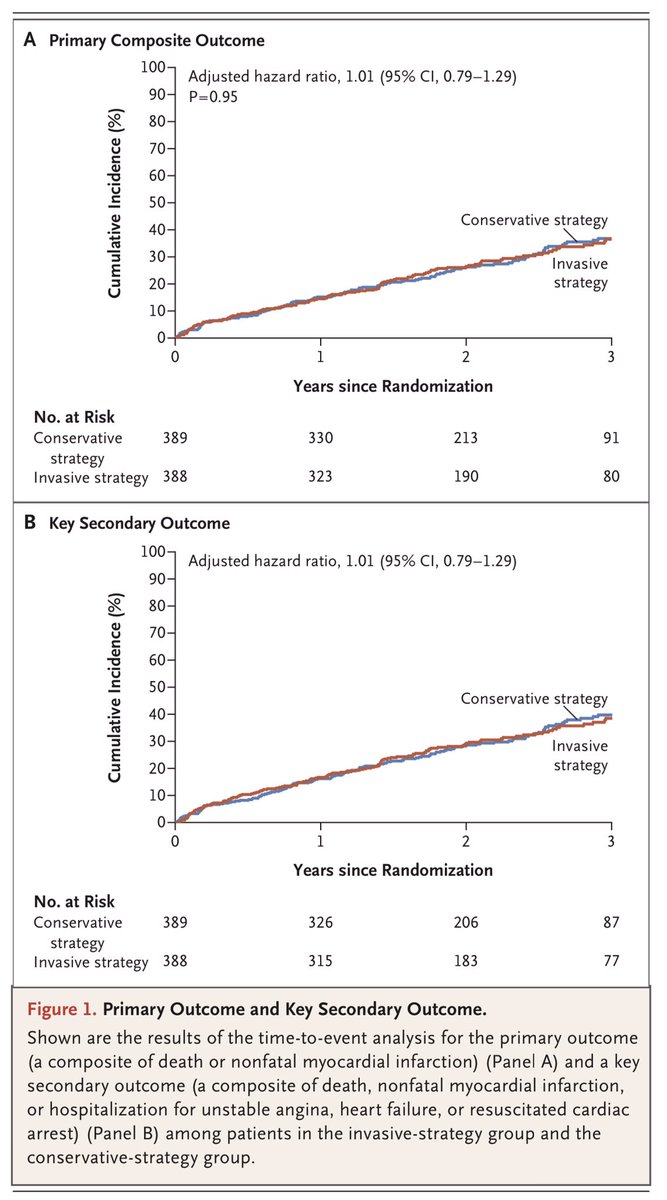



ISCHEMIA-CKD: Among patients with stable coronary disease, advanced CKD, and moderate or severe ischemia, an initial invasive strategy (vs initial conservative strategy), did not reduce the risk of death or nonfatal MI ca. 2020 from @NEJM #Nephpearls
👉🏼 nejm.org/doi/full/10.10…

👉🏼 nejm.org/doi/full/10.10…


• • •
Missing some Tweet in this thread? You can try to
force a refresh