All credit goes to @AvrahamCooperMD; the following tweetorial is his brainchild. Thanks, Avi!
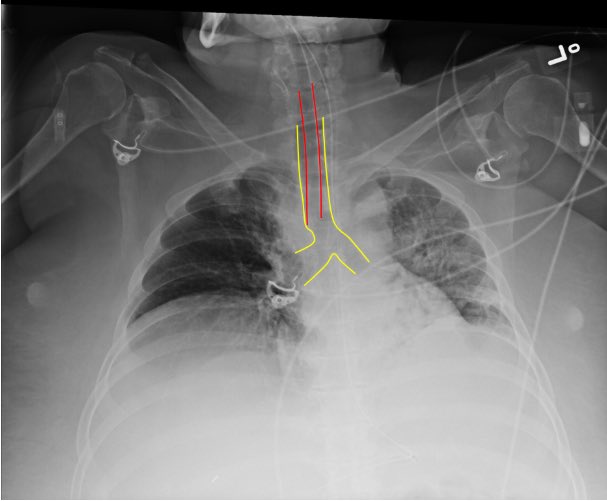
- Did capnography confirm tracheal placement?
- Are breath sounds bilateral?
- Is the tube placed appropriately on CXR? (typically 2-5 cm from carina)
Pic from SAEM bit.ly/3bJrTpa
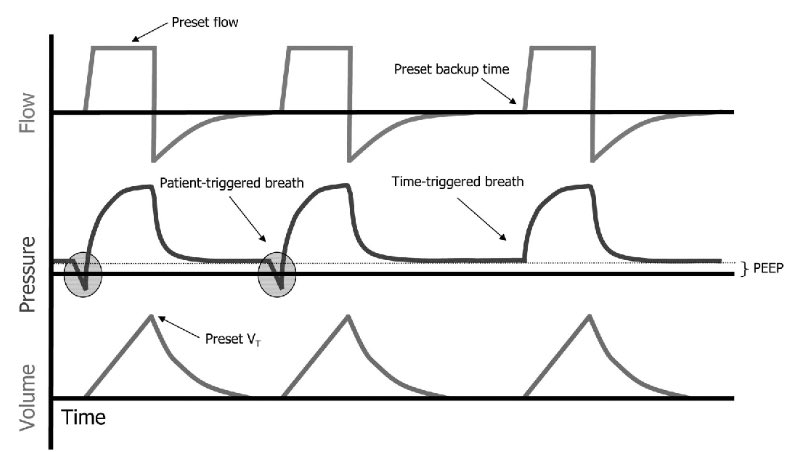
Typically this will be assist control/volume control (AC/VC) which allows you to:
✔️ Maintain low tidal volume ventilation
✔️ Guarantee a respiratory rate
Pic from bit.ly/3462mny
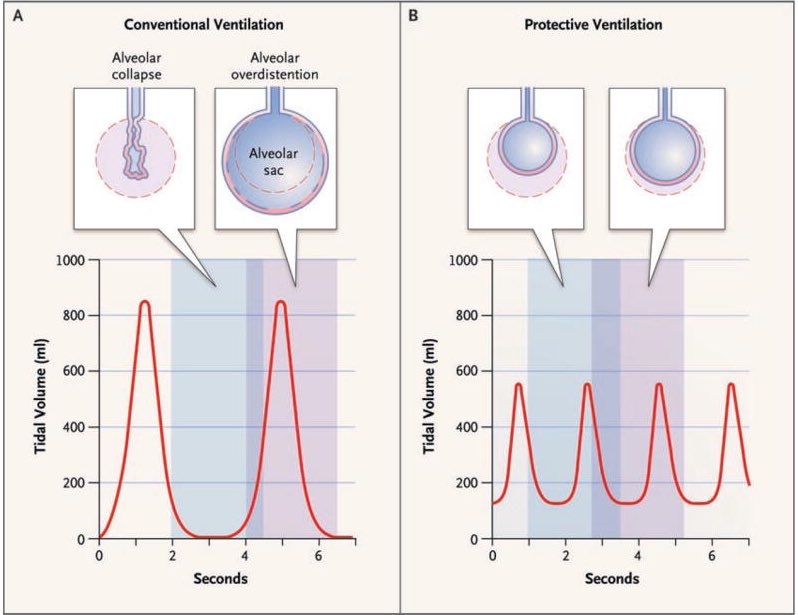
-Try to approximate pre-intubation MV (not always possible)
-Use low tidal volume ventilation (4-8 ml/kg ideal body weight)
-Goal plateau pressure < 30 mmHg
-Goal pH > 7.2
ncbi.nlm.nih.gov/pubmed/17855672
- Avoid O2 sats of 100% (hyperoxia is bad), aim for 92%-95%
- Set adequate PEEP, typically >10 mmHg in ARDS
COVID19 patients are PEEP-sensitive. In general aim for higher PEEP and lower FiO2.
ebmedicine.net/topics/infecti…
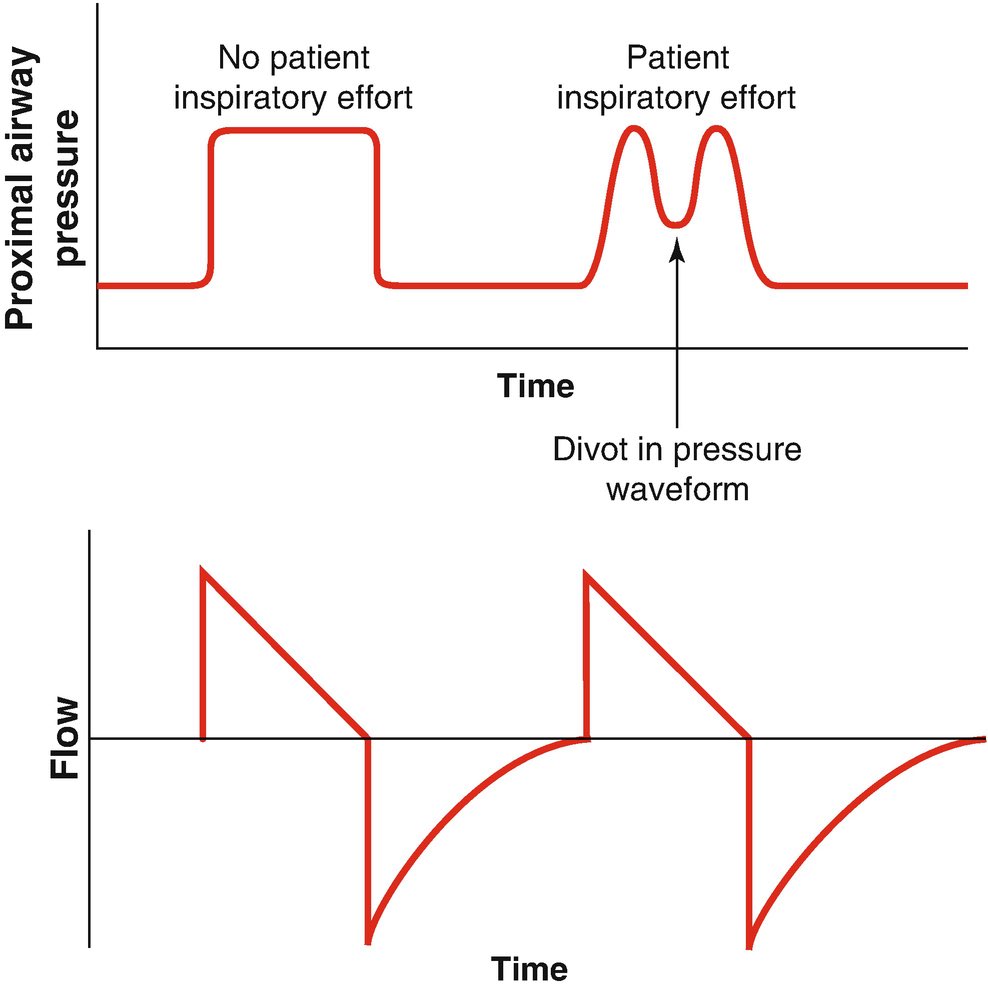
- Patients with moderate to severe ARDS usually need sedation to ensure vent synchrony
- Vent Dyssynchrony ⬇️ oxygenation and ⬆️ lung injury
- Whatever sedation you choose, achieve synchrony
link.springer.com/chapter/10.100…
Others will require additional therapies. Let's briefly review:
😑Paralysis
🙃Proning
😮Inhaled pulmonary vasodilators
Those patients that remain dyssynchronous/hypoxemic despite sedation.
Paralysis does not improve mortality in severe ARDS but individual patients may benefit.
nejm.org/doi/full/10.10…
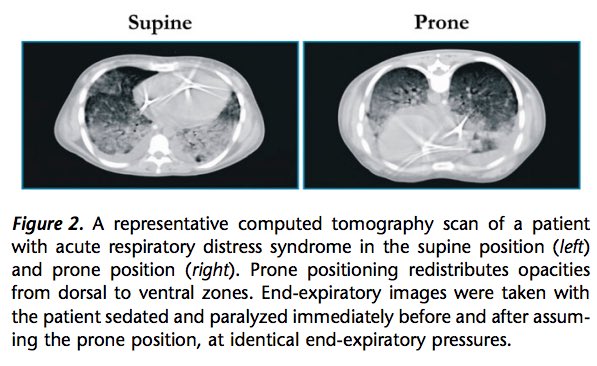
✔️Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.
✔️It has been shown to reduce mortality in those with PaO2:FiO2 < 150.
ncbi.nlm.nih.gov/pubmed/24134414
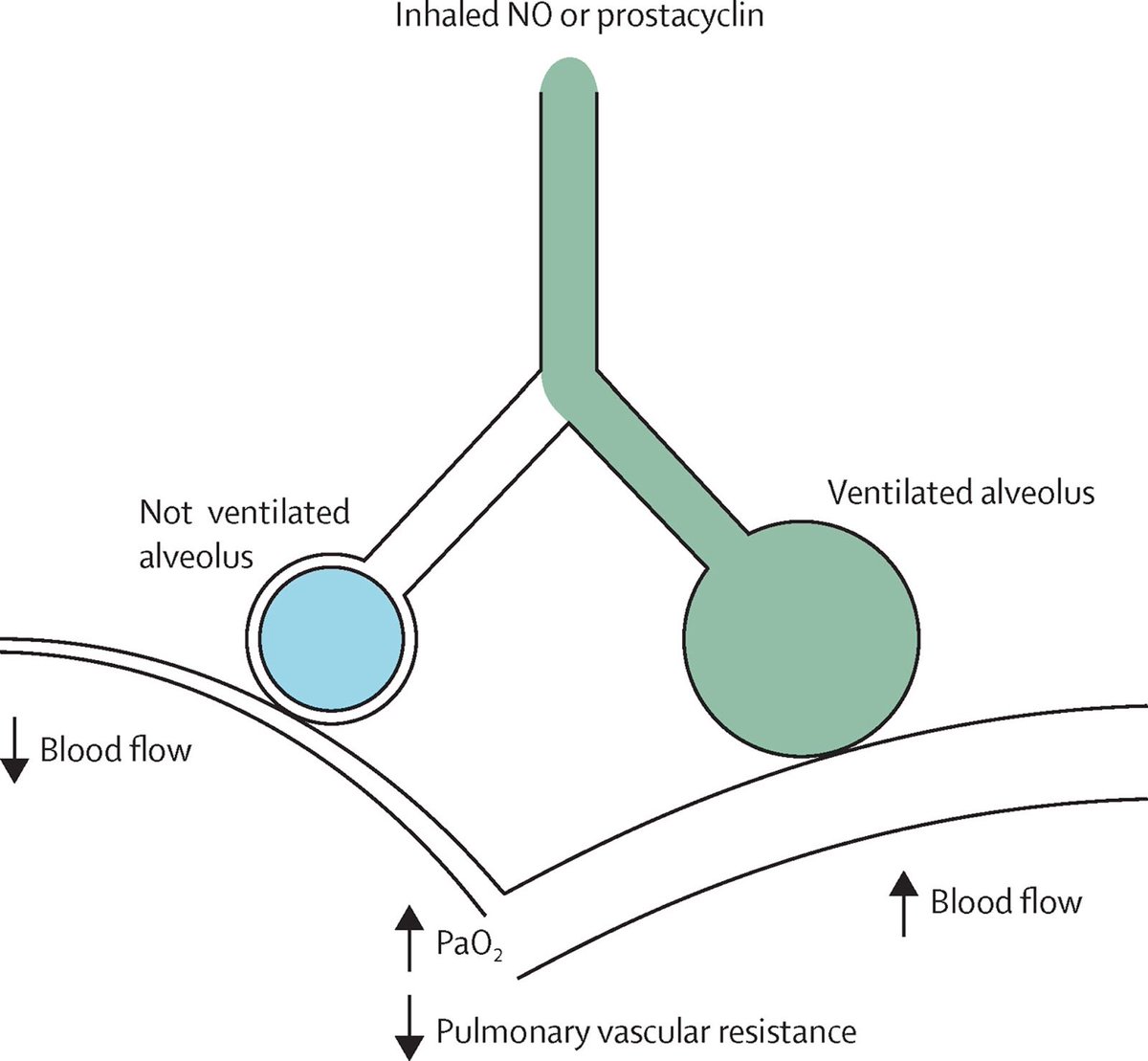
1️⃣Epoprostenol or
2️⃣nitric oxide
- Preferentially vasodilate aerated lung units, ⬆️ V/Q matching and ⬆️ SpO2
- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia
ncbi.nlm.nih.gov/pubmed/27203510
✔️ Confirm tube position
✔️Low tidal volumes, adequate PEEP
✔️Tolerate respiratory acidosis
✔️ Sedate for synchrony
✔️ If still hypoxemic, prone and probably paralyze, inhaled vasodilators if refractory
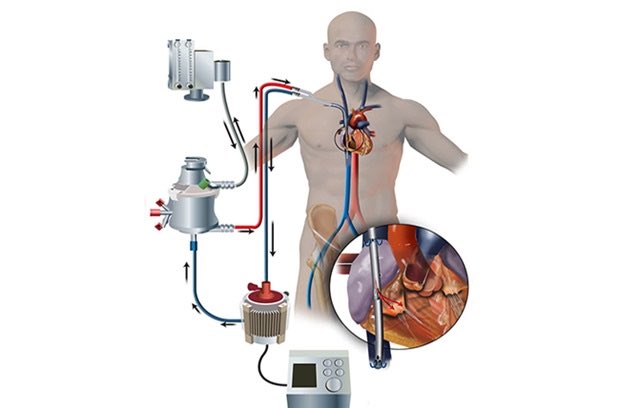
✔️ Better to call for ECMO too early than too late