28/F fom Bolivia, no PMH, referred to you for a +Trypanosoma cruzi serology. No SSx, has normal EKG (w/ 30 sec strip), CXR & echo. Which of the following complications of Chagas’ disease has the most evidence to support treating her with benznidazole to reduce risk?
1/14
Only 1/3 got the correct answer: vertical transmission.
Although most patients with indeterminate Chagas are treated w/ benznidazole, there is limited data on the effect of Rx to progression to cardiomyopathy/GI involvement (partly because it requires decades of ffup).
Only 1/3 got the correct answer: vertical transmission.
Although most patients with indeterminate Chagas are treated w/ benznidazole, there is limited data on the effect of Rx to progression to cardiomyopathy/GI involvement (partly because it requires decades of ffup).
2/14
There is also limited data (& no broad consensus) in treating indeterminate Chagas in patients who are at risk for reactivation (e.g. HIV, those undergoing transplant). bit.ly/2z3p5Fs bit.ly/2z00jpM
There is also limited data (& no broad consensus) in treating indeterminate Chagas in patients who are at risk for reactivation (e.g. HIV, those undergoing transplant). bit.ly/2z3p5Fs bit.ly/2z00jpM
3/14
But there is stronger evidence that treatment of indeterminate Chagas among women of reproductive age PRIOR to pregnancy reduces the risk of vertical transmission by as much as 95%. bit.ly/3aYl3eE
But there is stronger evidence that treatment of indeterminate Chagas among women of reproductive age PRIOR to pregnancy reduces the risk of vertical transmission by as much as 95%. bit.ly/3aYl3eE
4/14
There are so many teaching points on Chagas disease but for this MCQ, I will highlight a few points on transmission, clinical manifestations, and treatment.
There are so many teaching points on Chagas disease but for this MCQ, I will highlight a few points on transmission, clinical manifestations, and treatment.
5/14
T. cruzi is transmitted 👇 by the triatome bug not directly from a bite but from its feces. The insect defecates as it bites; T. cruzi in the feces enters the blood through the bite wound or an intact mucosa like the conjunctiva (producing the classic Romana’s sign 👇).

T. cruzi is transmitted 👇 by the triatome bug not directly from a bite but from its feces. The insect defecates as it bites; T. cruzi in the feces enters the blood through the bite wound or an intact mucosa like the conjunctiva (producing the classic Romana’s sign 👇).


6/14
Refer again to the diagram☝️cyle 3️⃣4️⃣ explains the clinical manifestations of Chagas. Although it can infect a wide variety of cells, trypomastigotes predominantly infect the heart and the gut, causing pathology.
Refer again to the diagram☝️cyle 3️⃣4️⃣ explains the clinical manifestations of Chagas. Although it can infect a wide variety of cells, trypomastigotes predominantly infect the heart and the gut, causing pathology.
7/14
Cycle 4️⃣ also tells you why one of the ways to diagnose acute Chagas disease is looking at the blood smear which we’ve talked about in greater details before.
Review here 👇#spacedlearning #retrievalpractice
Cycle 4️⃣ also tells you why one of the ways to diagnose acute Chagas disease is looking at the blood smear which we’ve talked about in greater details before.
Review here 👇#spacedlearning #retrievalpractice
https://twitter.com/WuidQ/status/1036295858738868225
8/14
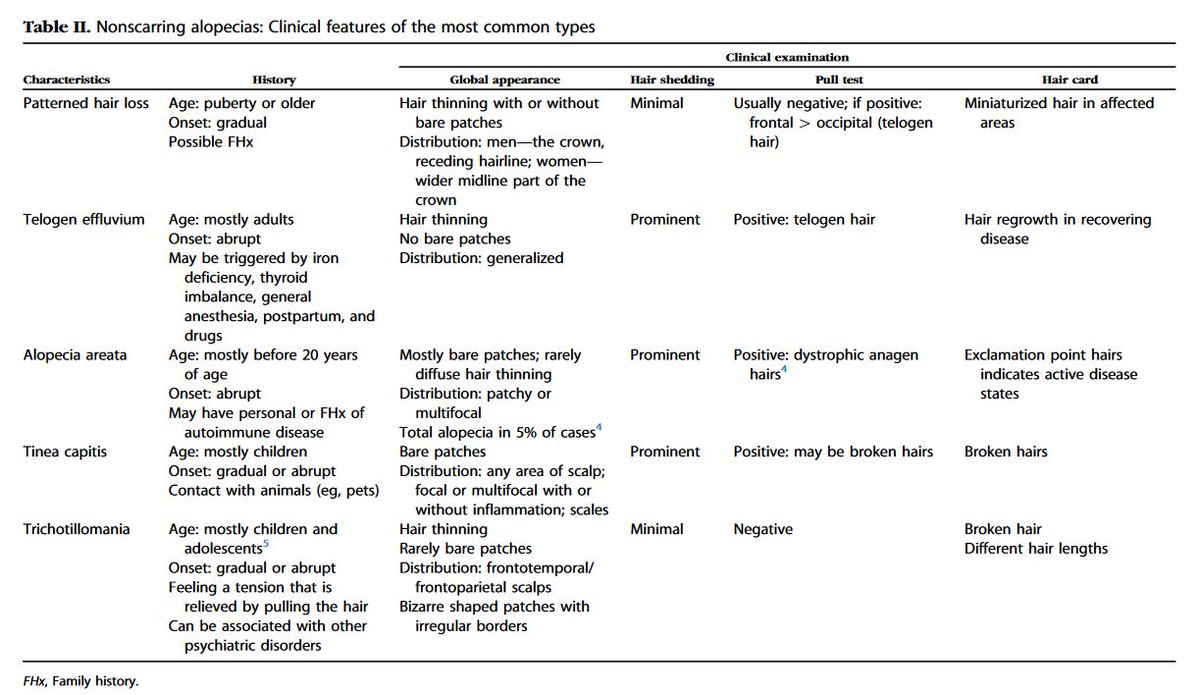
The table👇 attempts to summarize the spectrum of Chagas in adults.
W/o Tx, acute 👉 chronic Chagas. 1st 30 y, most will be indeterminate; 20-40% will progress to determinate.
Note: brain abscess and rash occur during reactivation but not so much in other forms.
The table👇 attempts to summarize the spectrum of Chagas in adults.
W/o Tx, acute 👉 chronic Chagas. 1st 30 y, most will be indeterminate; 20-40% will progress to determinate.
Note: brain abscess and rash occur during reactivation but not so much in other forms.
9/14
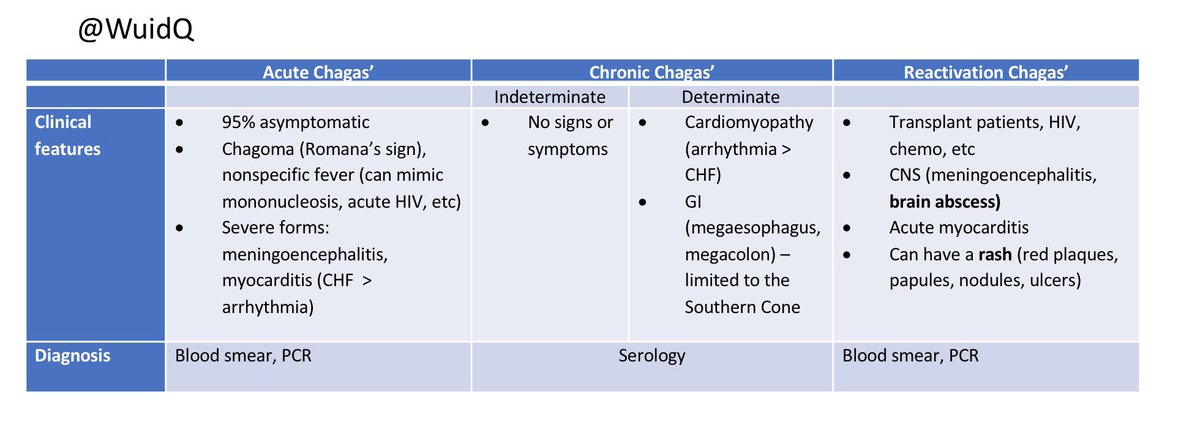
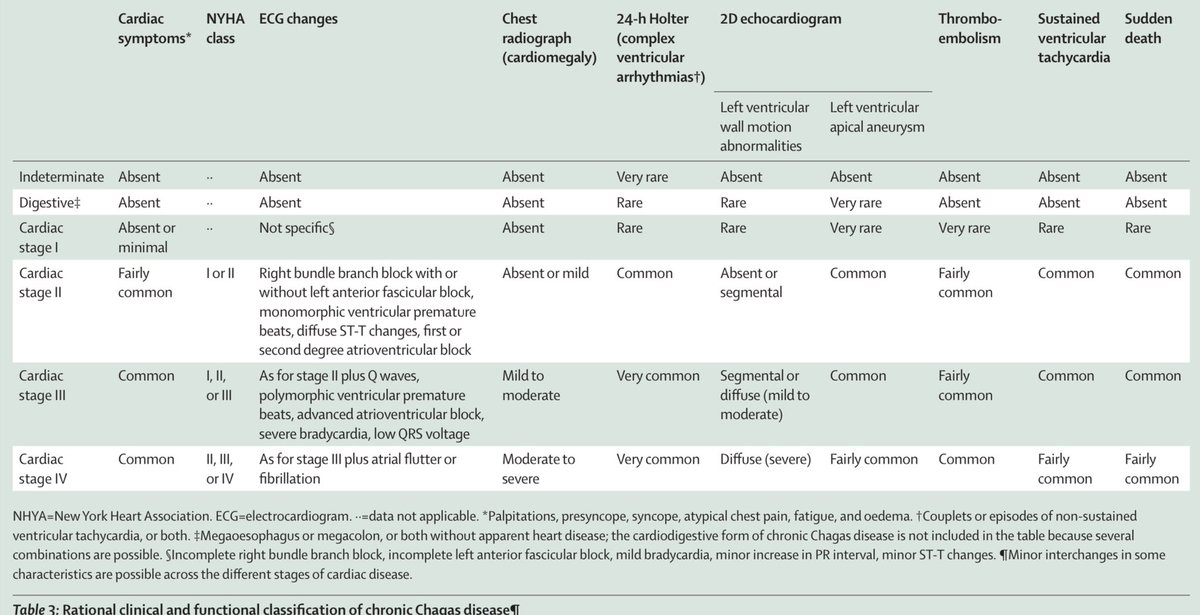
Image 1👇depicts the manifestations of chronic Chagas bit.ly/3fcMSU6
Image 2 👇depicts classification of chronic chagasic cardiomyopathy and GI disease bit.ly/3dasyAR

Image 1👇depicts the manifestations of chronic Chagas bit.ly/3fcMSU6
Image 2 👇depicts classification of chronic chagasic cardiomyopathy and GI disease bit.ly/3dasyAR

10/14
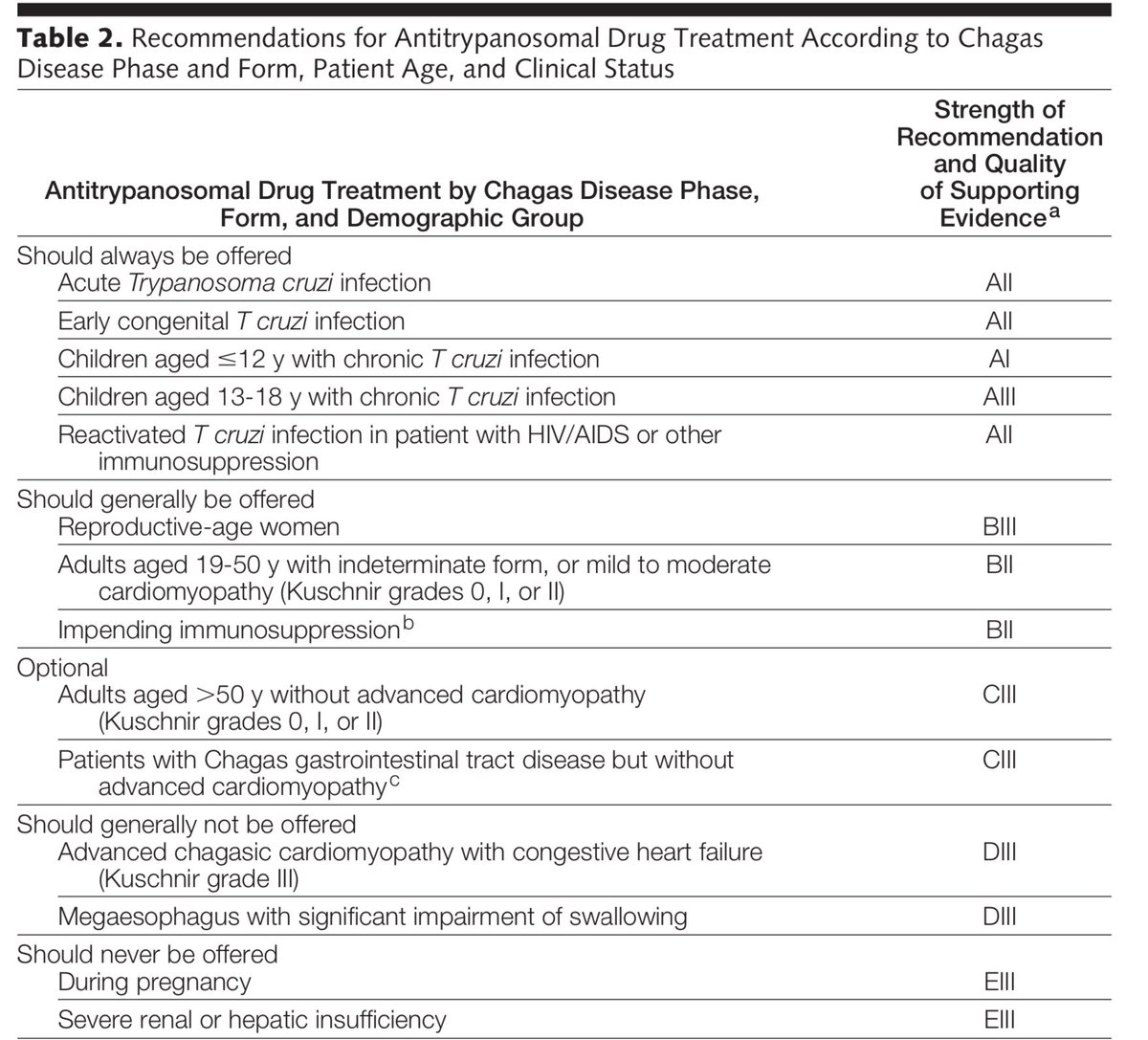
Which groups of patients benefit most from treatment? 👇bit.ly/3fcMSU6
There is broad consensus that the ff groups benefit the most & should be get tx (a/w high cure rates):
▪️Acute infxn
▪️Infants/congenital infxn
▪️Children <18 yrs
▪️Reactivation disease
Which groups of patients benefit most from treatment? 👇bit.ly/3fcMSU6
There is broad consensus that the ff groups benefit the most & should be get tx (a/w high cure rates):
▪️Acute infxn
▪️Infants/congenital infxn
▪️Children <18 yrs
▪️Reactivation disease
11/14
Patients w/ less advanced GI dx & cardiomyopathy may also benefit from Tx but the evidence is less robust.
As @CrystalZhengMD pointed, no discussion of Chagas is complete w/o bringing up the BENEFIT trial bit.ly/2xsifsG (benefit w/ prasitemia, none clinically).
Patients w/ less advanced GI dx & cardiomyopathy may also benefit from Tx but the evidence is less robust.
As @CrystalZhengMD pointed, no discussion of Chagas is complete w/o bringing up the BENEFIT trial bit.ly/2xsifsG (benefit w/ prasitemia, none clinically).
12/14
Chagas is a zoonosis and humans are incidental hosts. Normally involved in a cycle between vector and its vast animal hosts.
Humans only become involved when land is opened up for farming. The natural habitat of the vector is disrupted and it becomes domiciliary.
Chagas is a zoonosis and humans are incidental hosts. Normally involved in a cycle between vector and its vast animal hosts.
Humans only become involved when land is opened up for farming. The natural habitat of the vector is disrupted and it becomes domiciliary.
13/14
This life cycle between the vector, animals, & humans as incidental hosts has been going on since the dawn of history👇. bit.ly/2Wk7XmL
Illustrates One Health, a concept that once again is brought to the fore in light of COVID-19. #COVID19 bit.ly/2Yw2njZ
This life cycle between the vector, animals, & humans as incidental hosts has been going on since the dawn of history👇. bit.ly/2Wk7XmL
Illustrates One Health, a concept that once again is brought to the fore in light of COVID-19. #COVID19 bit.ly/2Yw2njZ

14/14
28 autochthonous Chagas (1955-2015) despite the many sp of triatomes in the US that carry T. cruzi. Apart from better housing in the US, triatomes here are more sylvatic than domiciliary, & don’t defecate as they bite unlike South American bugs. bit.ly/2ybZpqj
28 autochthonous Chagas (1955-2015) despite the many sp of triatomes in the US that carry T. cruzi. Apart from better housing in the US, triatomes here are more sylvatic than domiciliary, & don’t defecate as they bite unlike South American bugs. bit.ly/2ybZpqj
• • •
Missing some Tweet in this thread? You can try to
force a refresh