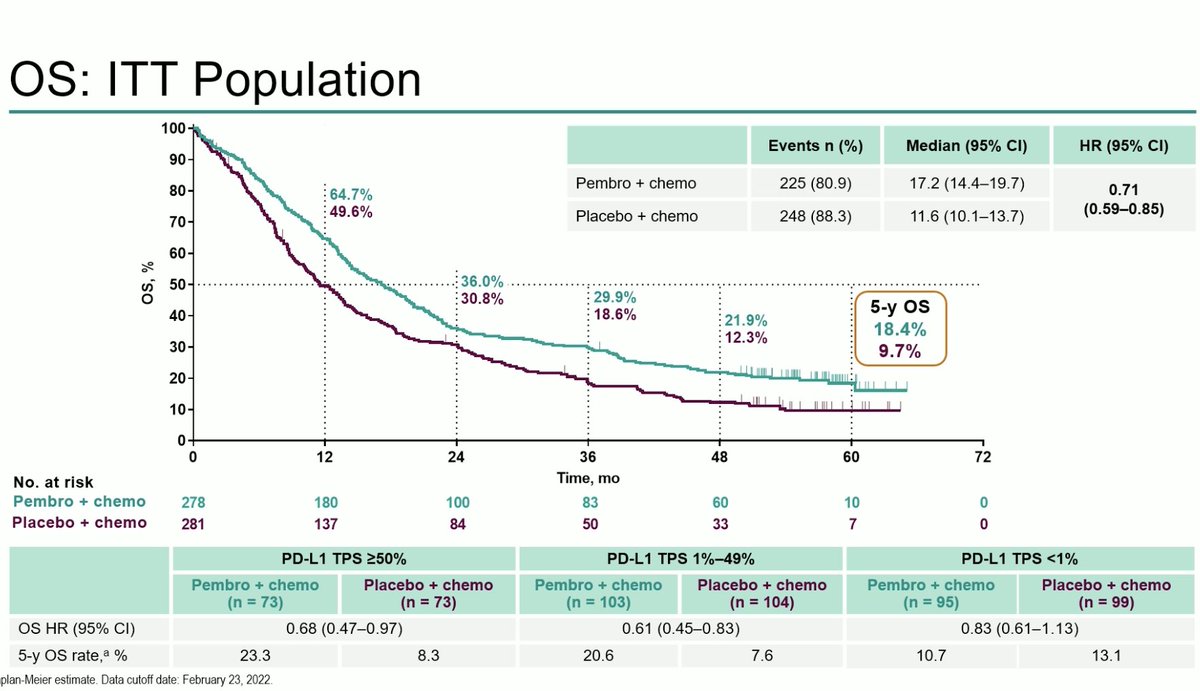
#OncoAlert Report @JTOonline on PDL1 variability in metastatic #NSCLC. A lot of intriguing information on this increasingly imperfect biomarker. Important to understand what's driving the heterogeneity and how it impacts treatment. @IASLC #LCSM
jto.org/article/S1556-…
jto.org/article/S1556-…
#OncoAlert In an analysis of 1398 patients with NSCLC they looked at patterns of PD-L1 expression and the impact of disease site and prior therapy. In a subset who received checkpoint inhibitors, they also looked at outcomes. Could influence how we look at PDL1 IHC. #LCSM
Lesson 1: PD-L1 varies by site. Previously reported. If the biopsy is from liver or adrenal, PDL1 runs higher. Brain and bone, PDL1 tends to be low. Some sets have small numbers but interesting trends and may reflect differences in the immune microenvironment #OncoAlert #LCSM 

Lesson 2: High PDL1 more common in tumors w/ #ALK fusions, #MET amp, #BRAF V600E, #RET fusions. We have to remember that PDL1 in the context of a driver alteration means something different. Since PDL1 IHC comes back quickly, we have to be patient and wait for NGS results! #LCSM
Lesson 3: Treatment may influence PDL1. 77 patients had paired biopsies with interval treatment. Half had a major change in PDL1. Prior IO therapy led to a major decrease in PDL1 in ~40% of patients. Trends persist even when same organ biopsied. #OncoAlert #LCSM
Lesson 4: Predictive value of PDL1 may vary by site. This is interesting: high PDL1 expression in biopsies from lung or distant metastases correlate with response (left) and survival (right). High PDL1 from lymph node biopsy was NOT associated with RR, PFS or OS! #OncoAlert #LCSM 


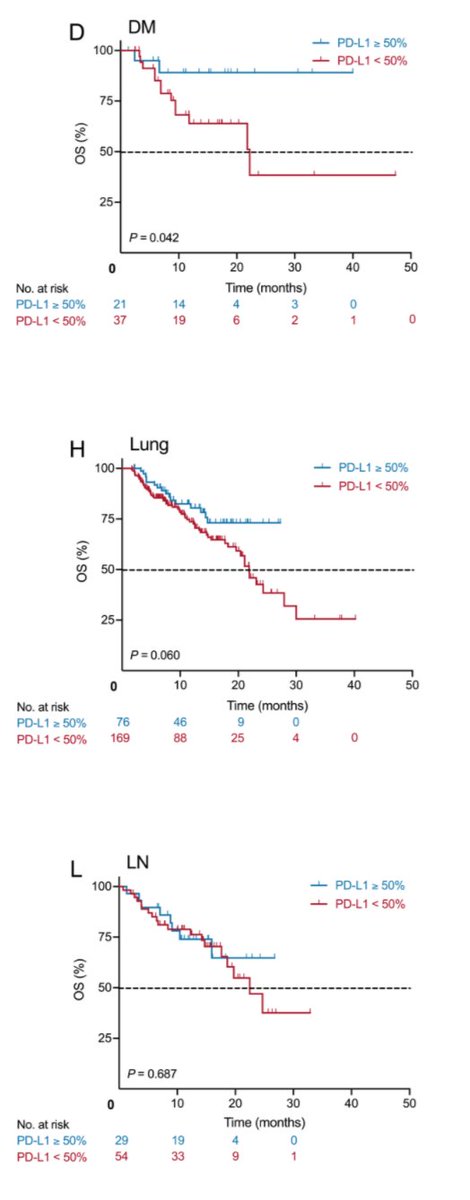
Perhaps we need to consider source of tissue when interpreting PDL1? If I have tissue from lung and lymph nodes, should I be testing the lung biopsy for PDL1? Perhaps send nodal tissue for NGS and save lung tissue for PDL1? Yet another variable to consider! #LCSM @IASLC 

• • •
Missing some Tweet in this thread? You can try to
force a refresh