Inspired by yesterday’s @CPSolvers case + last week’s NEJM case, reprising this thread with 5 more real case examples of this take-home point:
In acute presentations, eosinophilia is often a pivot point: it dramatically shifts/narrows the ddx.
1/11
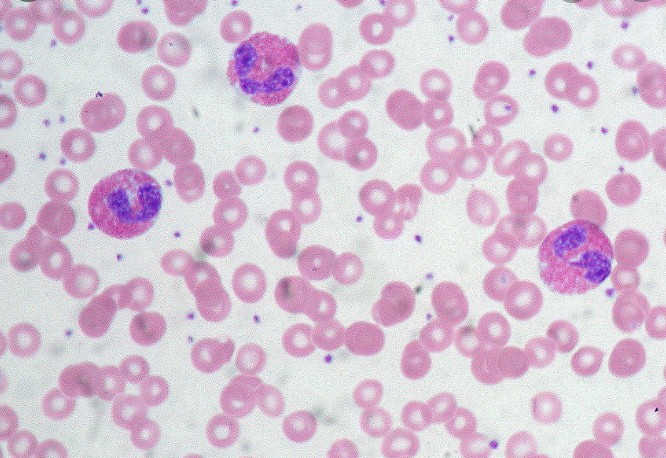
If you're acutely ill and have eosinophilia, the eos are probably related to why you're sick.
2/
Total WBC 2K with 15% eos? AEC is 300 (normal)
Total WBC 20K with 3% eos? AEC is 600 (elevated)
3/
Neoplasm: heme > solid
Allergy: drugs or atopy
Adrenal insuff: (loss of tonic suppression of eos)
Collagen-vascular dz: vasculitis, lupus
Parasites (helminths) & some fungi (cocci, aspergillus)
+ primary hypereo syndromes (eosin. X-itis)
4/
Now on to brief summaries of 5 recent cases where eosinophilia changed everything.
5/
clinicalproblemsolving.com/dx-schema-eosi…
Would have pursued only usual considerations and workup... but 700 eos in the blood.
Dx: eosinophilic myocarditis (needs steroids!)
6/
Dx: drug hypersensitivity
Pearl: NEW onset eos while in hospital? Probably drugs
7/
Breathing initially better, but admitted to hospital with severe sepsis, blood growing GNRs. 500 eos.
Dx. disseminated strongyloidiasis
8/
Dx: rectal cancer with mets to spine
9/
Dx: eosinophilic granulomatosis with polyangiitis
10/
But especially in acutely ill patients, it's often the key. Consider its differential, and how it may fit with the patient's presentation.
11/11



