Grand Rounds day; it's here: bit.ly/2WW49bH
Three segments: a) two @UCSF ICU docs returning from NYC; b) community-based studies in SF’s Mission District & rural Bolinas; and c) a deep dive into antibody testing. Summaries below.
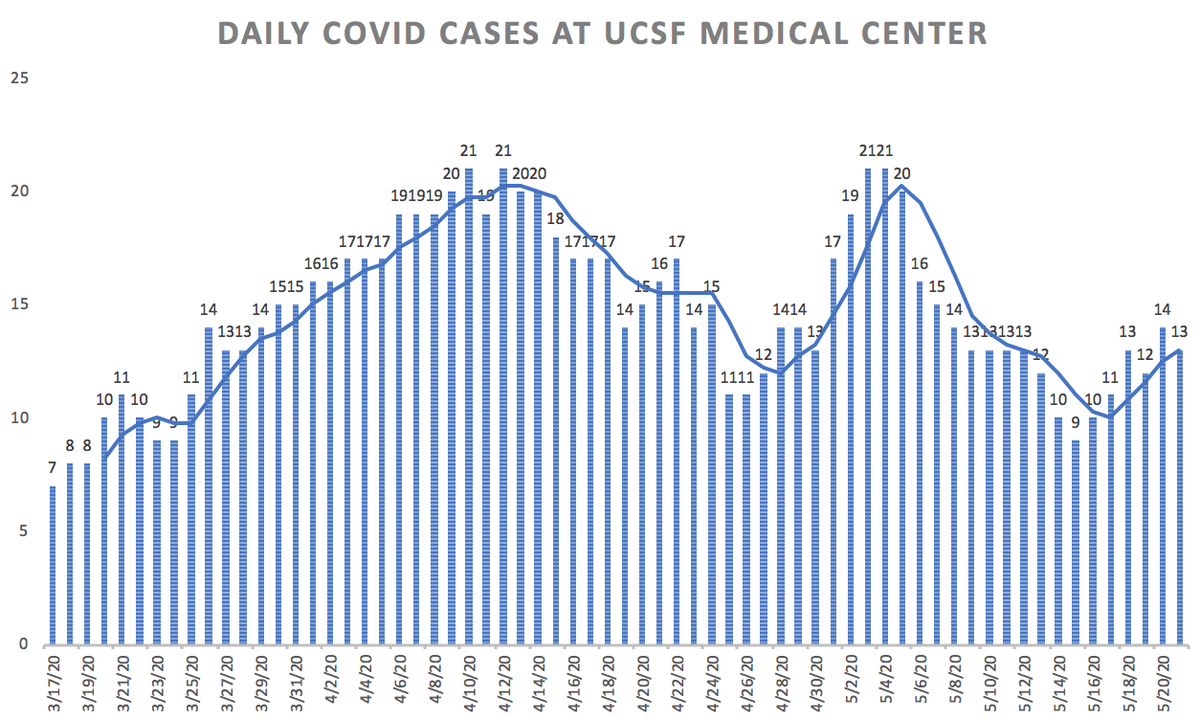
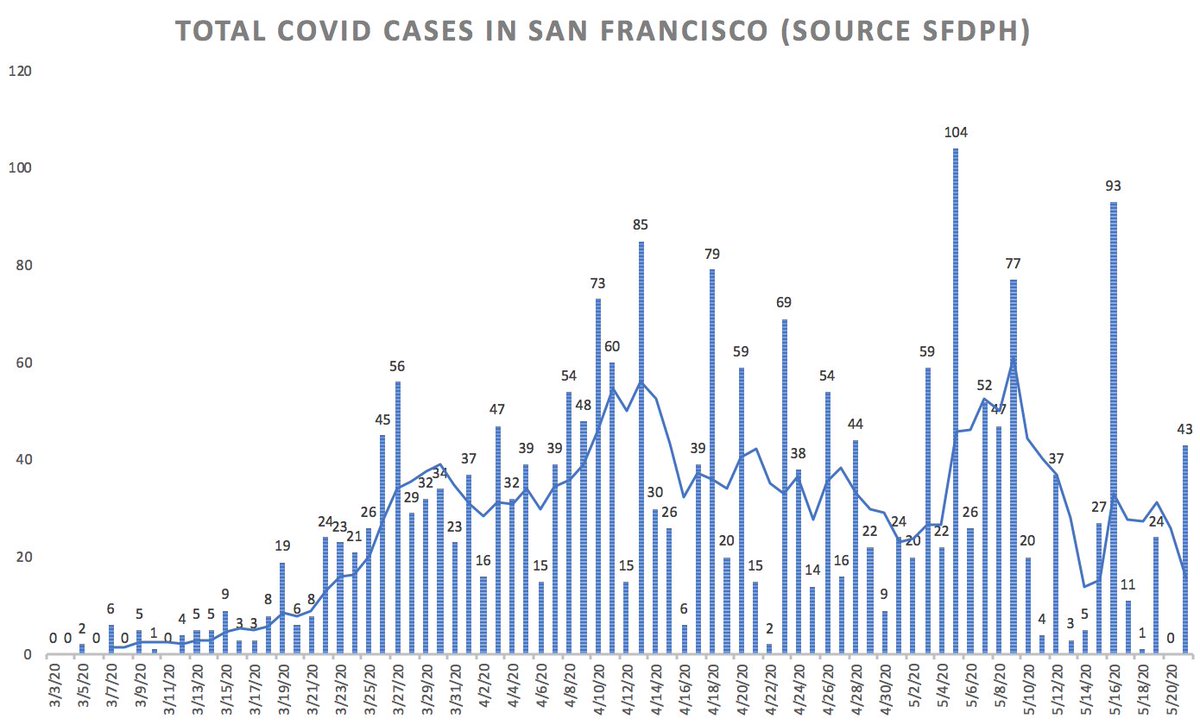
San Francisco data terrific: new cases (top R) & hospitalizations (bottom R) falling fast. Over last 5 days, average of 14 new cases/day in SF and zero new deaths.



So grateful to our NYC team.





Back tomorrow with tweets. Next Grand Rounds next Thursday. Stay well...