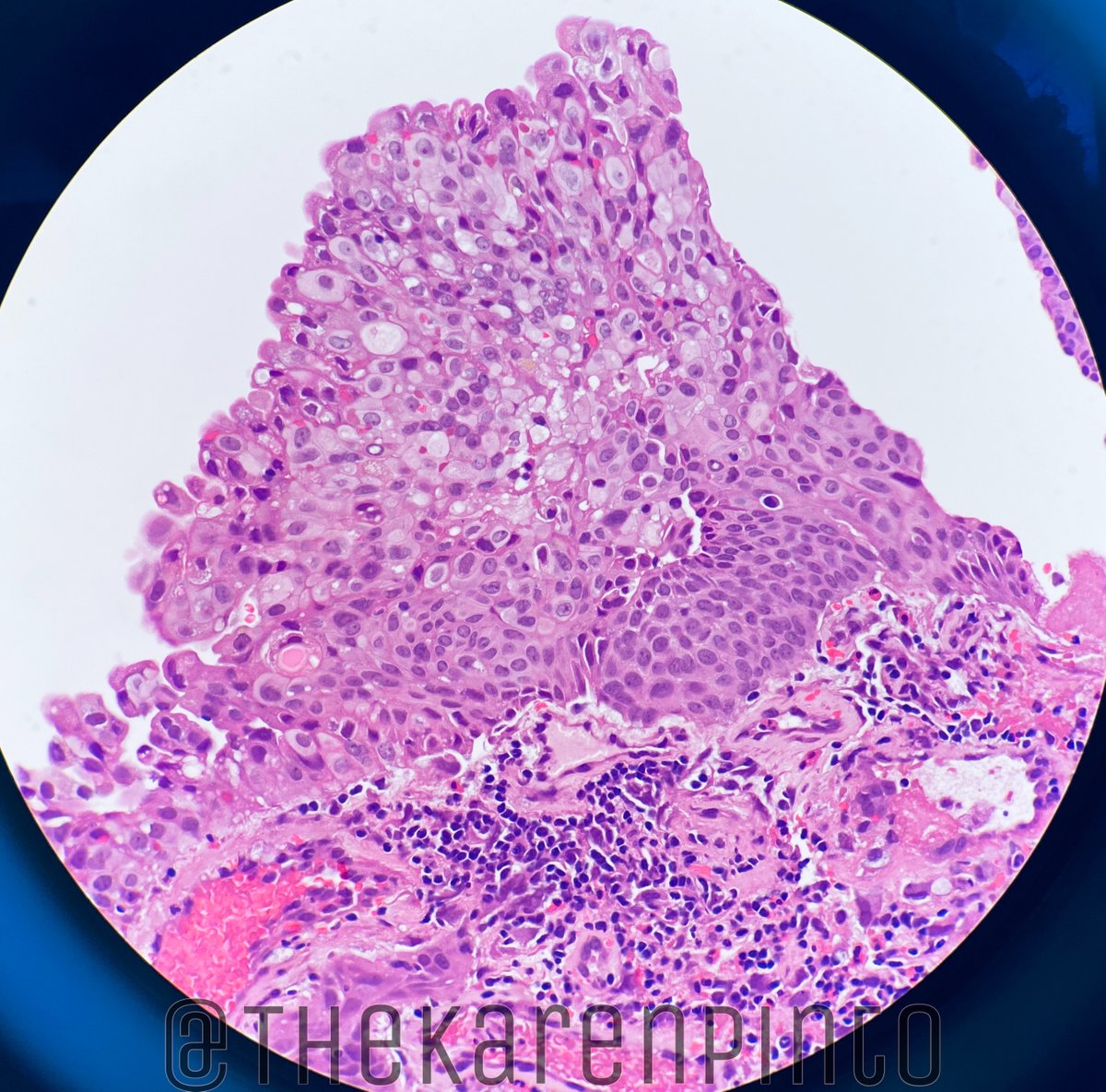
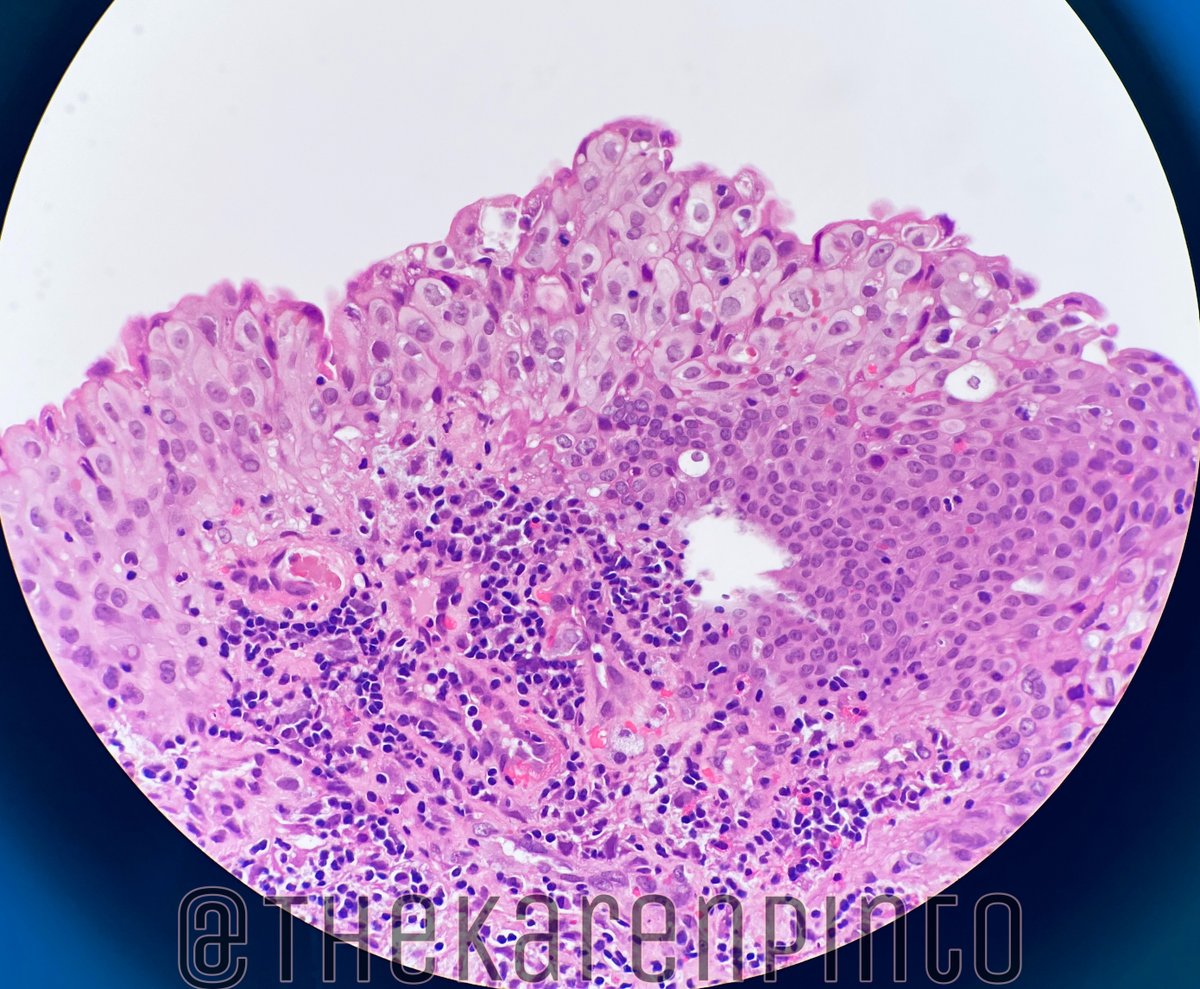
Cystoscopy: Congested mucosa with bleeding ulcers
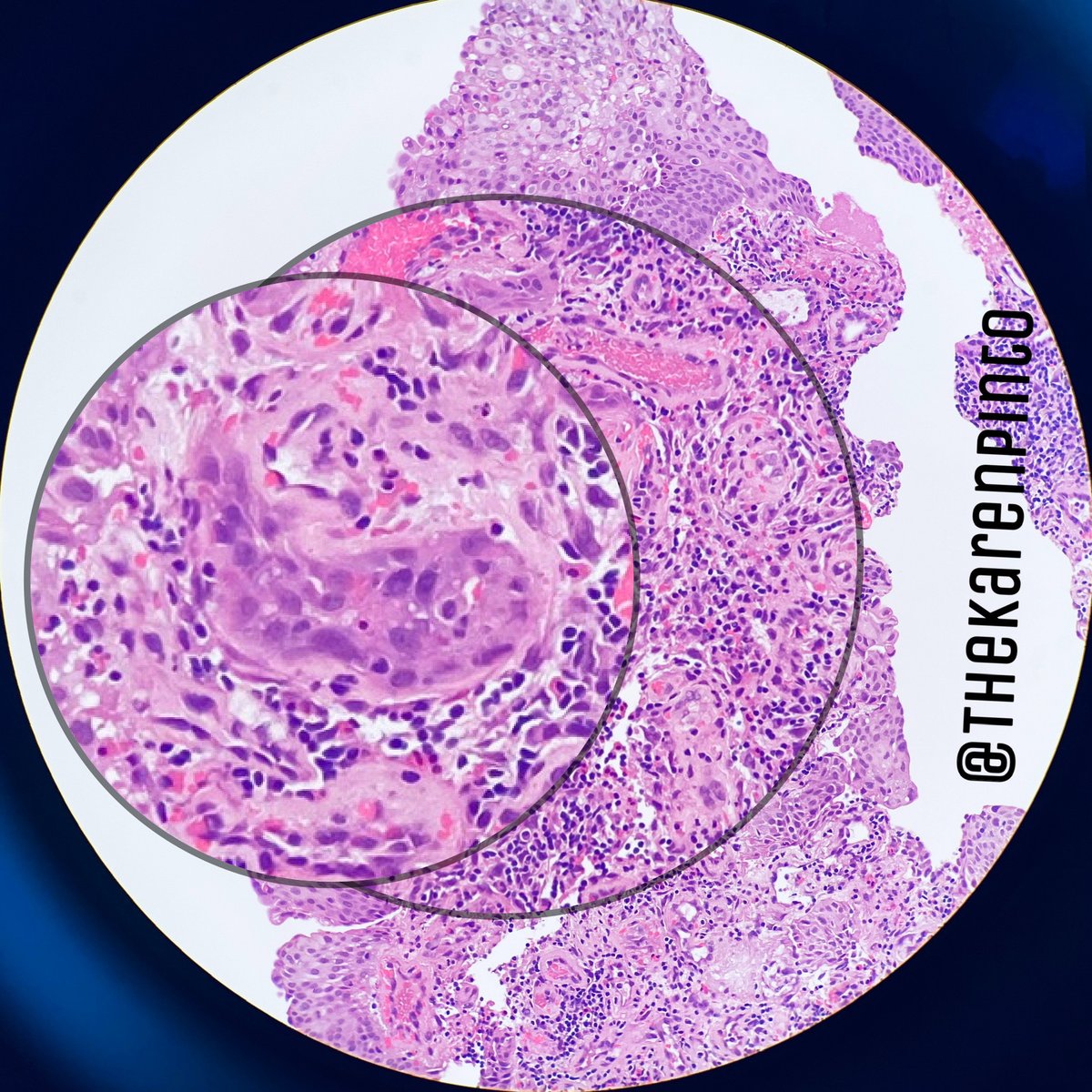
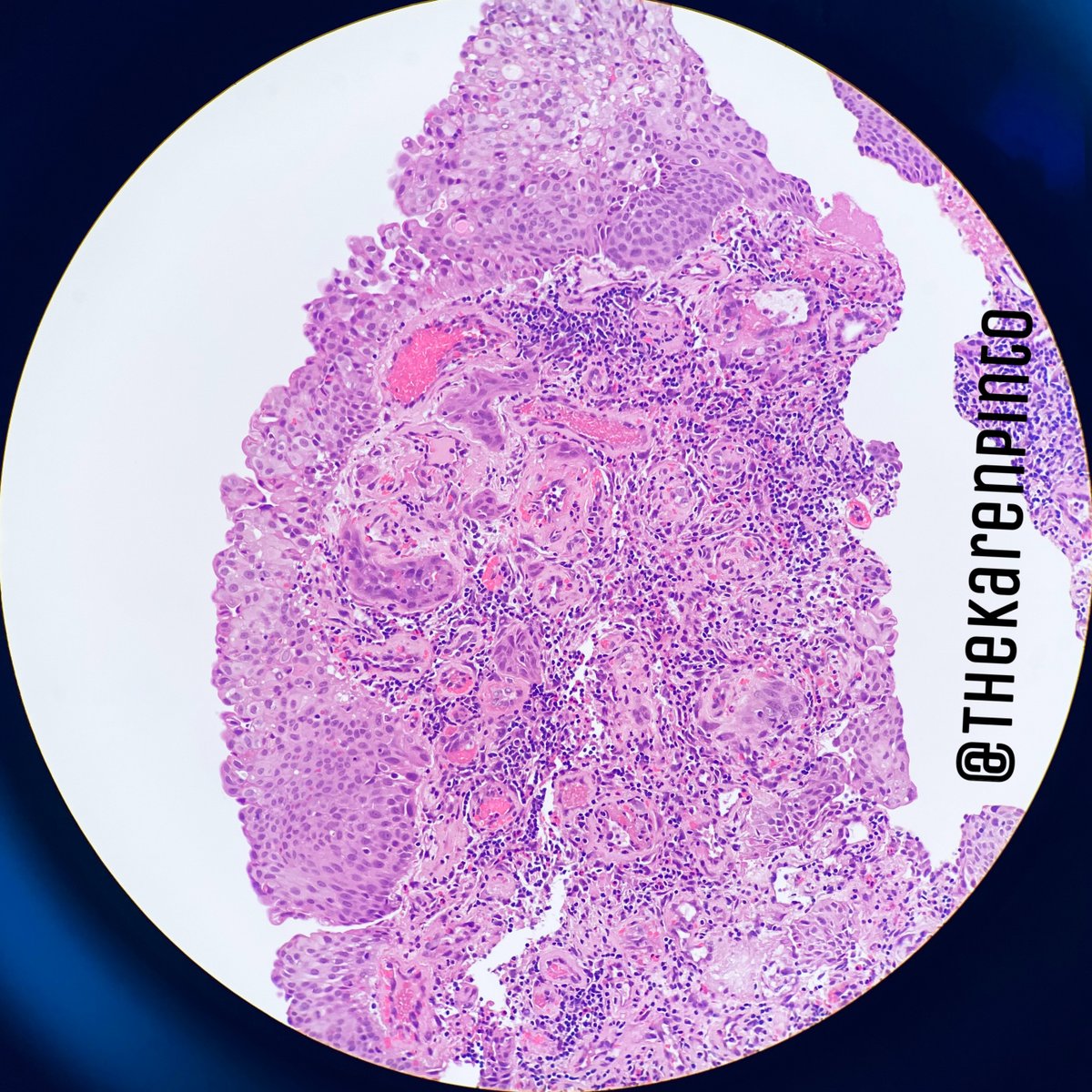
Biopsy from urinary bladder lesion
#pathology #GUPath
1. This could be a new urinary bladder primary
2. This could be metastasis from cervix
3. This is benign
YES
So this is benign
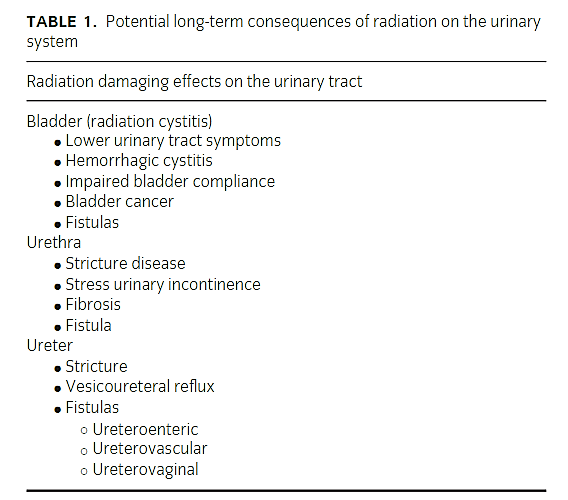
Radiation can be given for cancers of urinary bladder, uterus, ovaries, cervix, prostate, colon, rectum etc.
Radiation for any pelvic tumor, will show changes in the colon & urinary bladder.
1. Increased frequency
2. Urgency
3. Voiding pain
4. Hematuria
Acute: 3-6 weeks
Chronic: 6 months to 20 YEARS
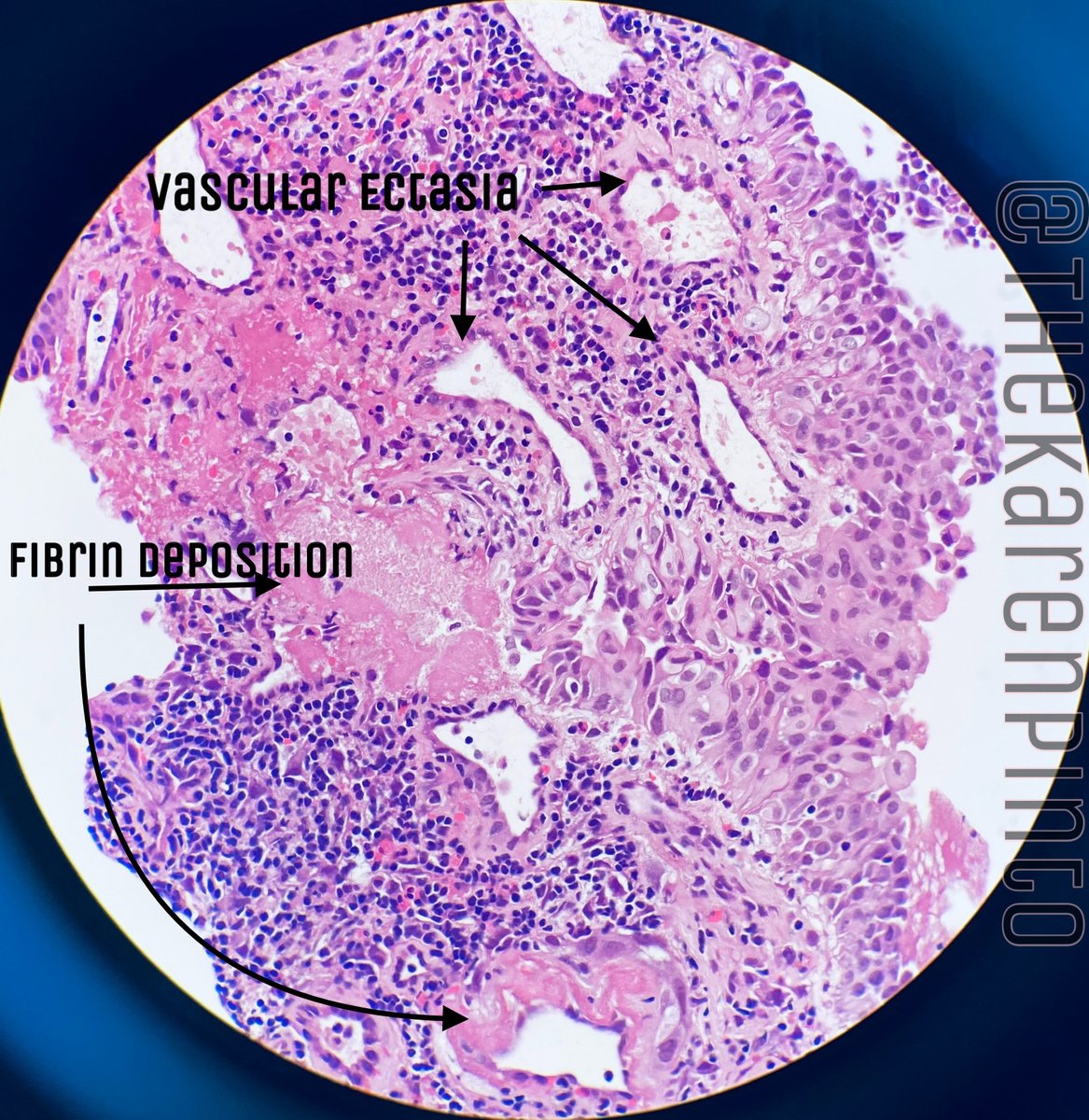
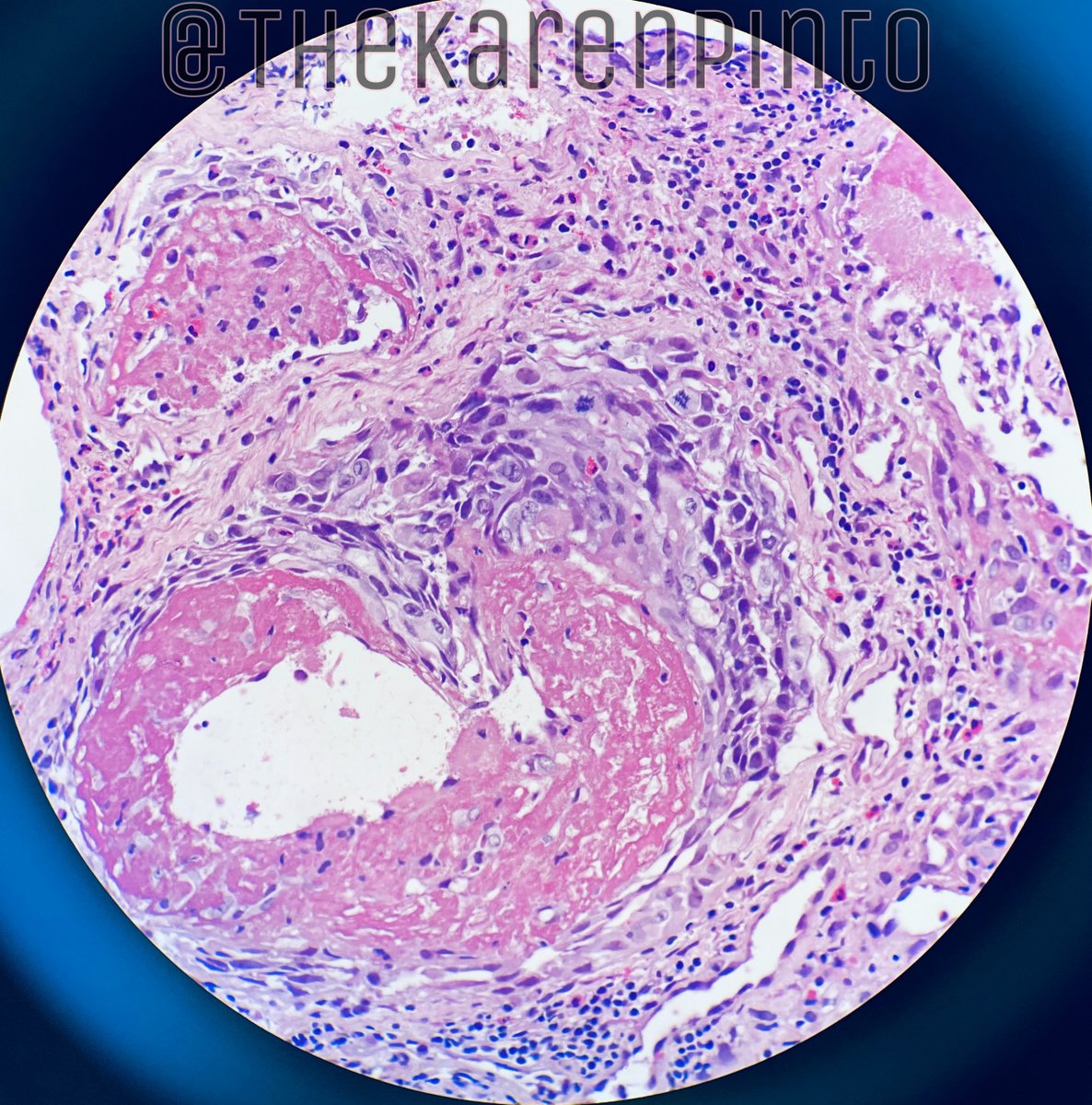
Bladder mucosa necrosis - shed off - hematuria
Permanent dilation of blood vessels - telangiectasia - bleeding
IC: doi.org/10.1111/luts.1…
H&E sometimes can look very frightening and it’s tough to distinguish it from carcinoma.
-Make sure you have the correct history + radiology
-Don’t be over-enthusiastic in calling anything “cancer” for a patient who has received radiation
End of #PathTweetorial