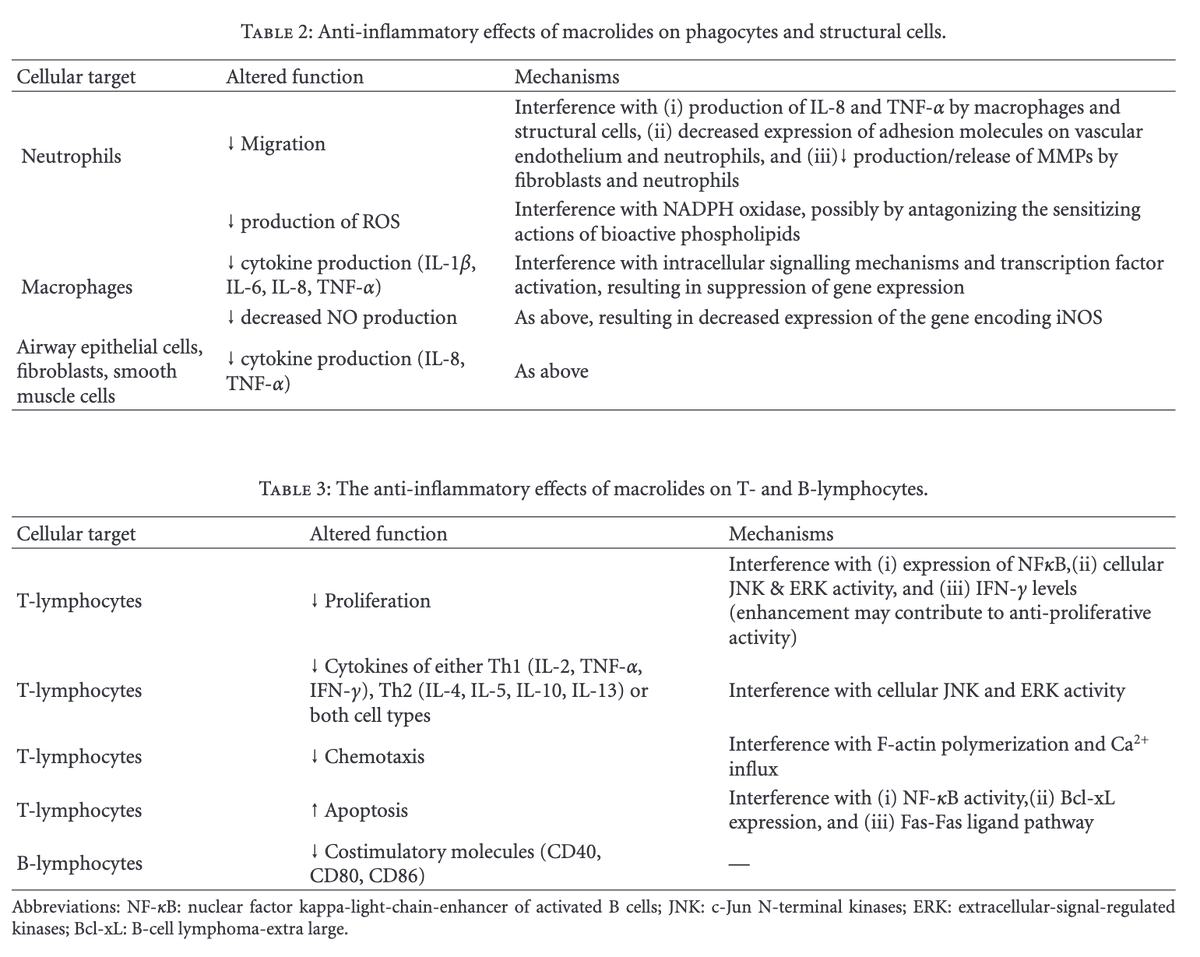
Why do patients with liver injury or dysfunction have conjugated hyperbilirubinemia?
If hepatocytes conjugate, why doesn't this "liver function" decrease in settings of severe inflammatory or fibrosis?
Before I offer a fuller explanation, I'll ask you: which plays a role?
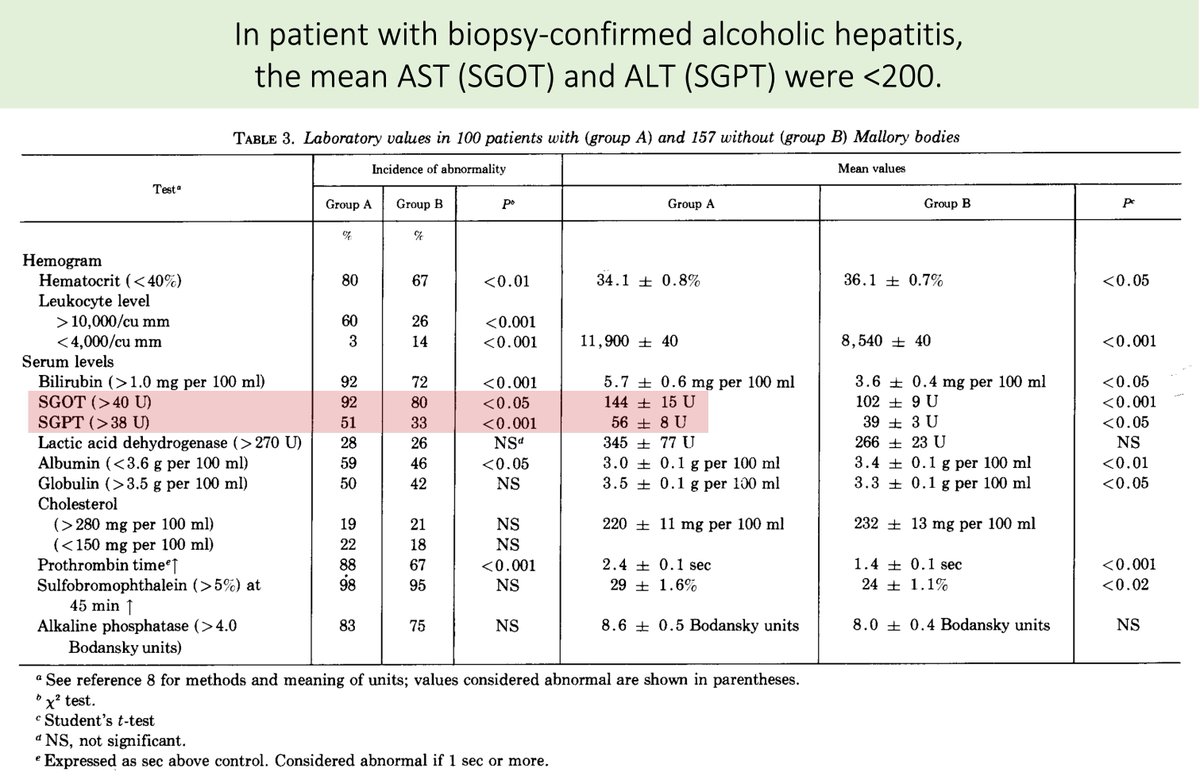
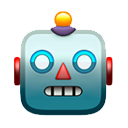
Let's start by confirming that liver diseases present with conjugated hyperbilirubinemia.
Here is the fraction of total bilirubin that is conjugated in 3 situations:
🔹Normal: 3.2%
🔹Chronic alcoholic cirrhosis: 20%
🔹Chronic viral hepatitis: 64%
ncbi.nlm.nih.gov/pubmed/25214800
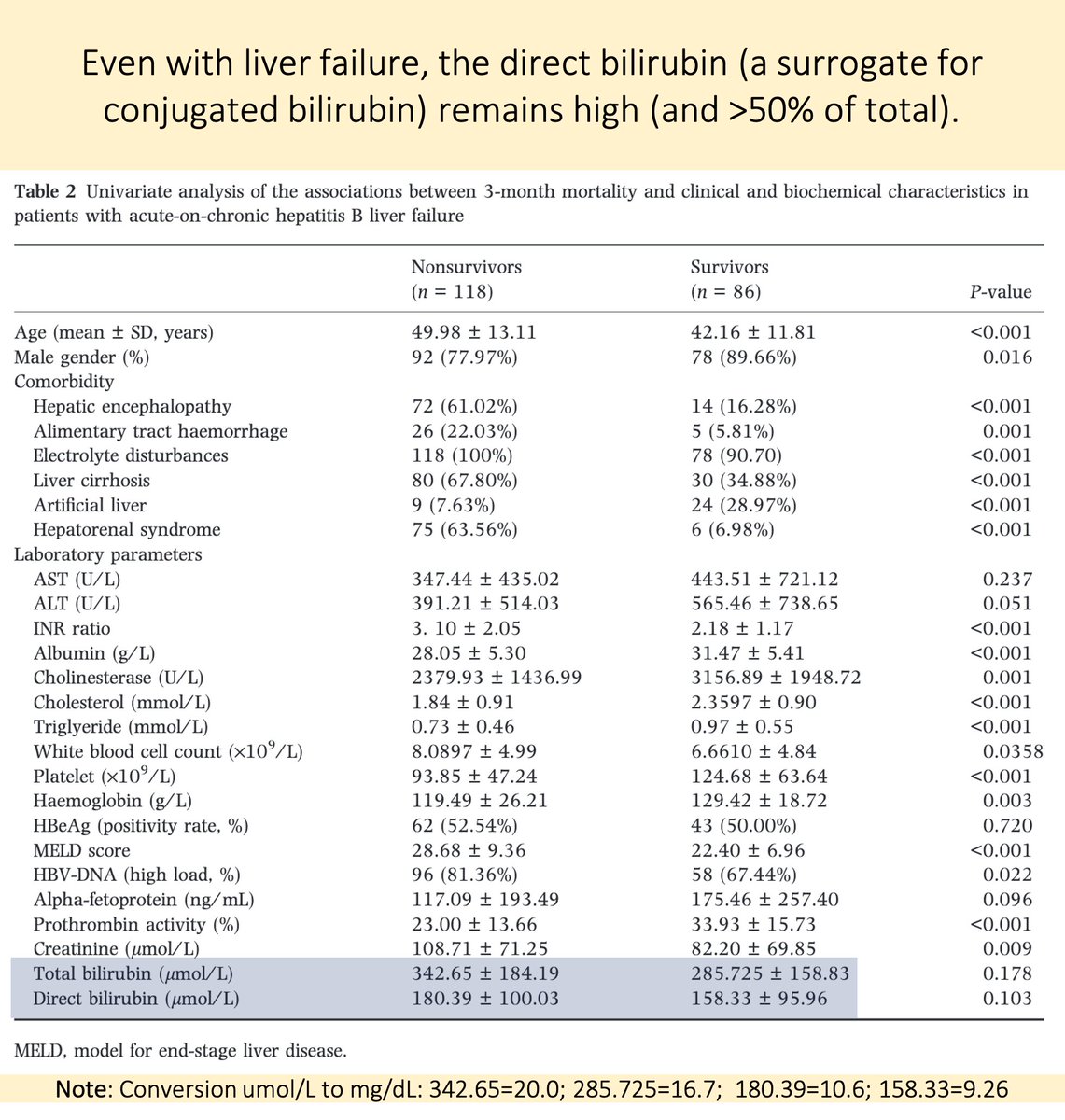
Even as the liver fails, its ability to conjugate bilirubin remains.
In one study of liver failure from hepatitis B, patients still had elevated conjugated bilirubin levels:
10.6 mg/dL for nonsurvivors
9.3 mg/dL for survivors
ncbi.nlm.nih.gov/pubmed/28440304
Ok, so we have identified the paradox that requires explanation:
💥How can a process (conjugation) that requires hepatocellular function continue when it appears that the liver is otherwise inflamed, fibrotic, or failing?💥
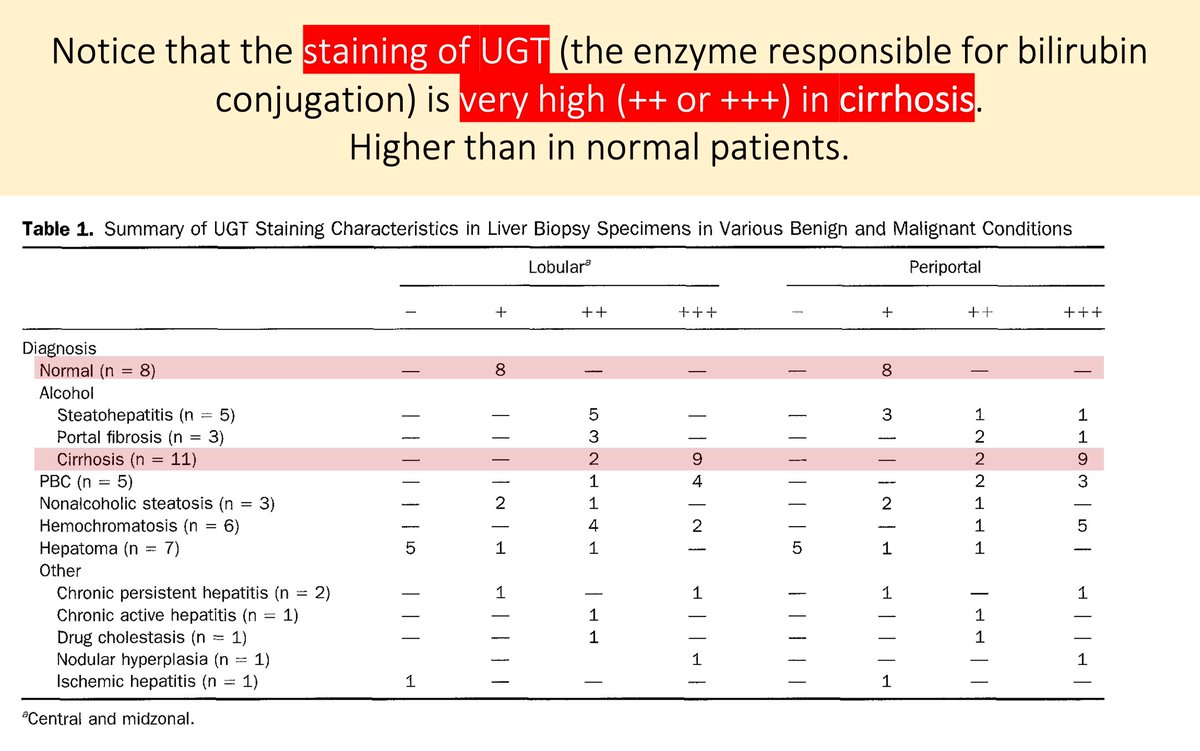
Here's the first part of the answer to our question:
In some liver diseases, there is upregulation of UGT enzyme content in the remaining viable hepatocytes.
i.e., Phase II function remains. It's worth noting that Phase I is often quite affected.
ncbi.nlm.nih.gov/pubmed/7729639
Furthermore, the levels of the specific isoform of UGT that conjugates bilirubin (UGT1A1) are stable as the degree of liver fibrosis progresses.
Even in severe fibrosis and cirrhosis.
ncbi.nlm.nih.gov/pubmed/11792680
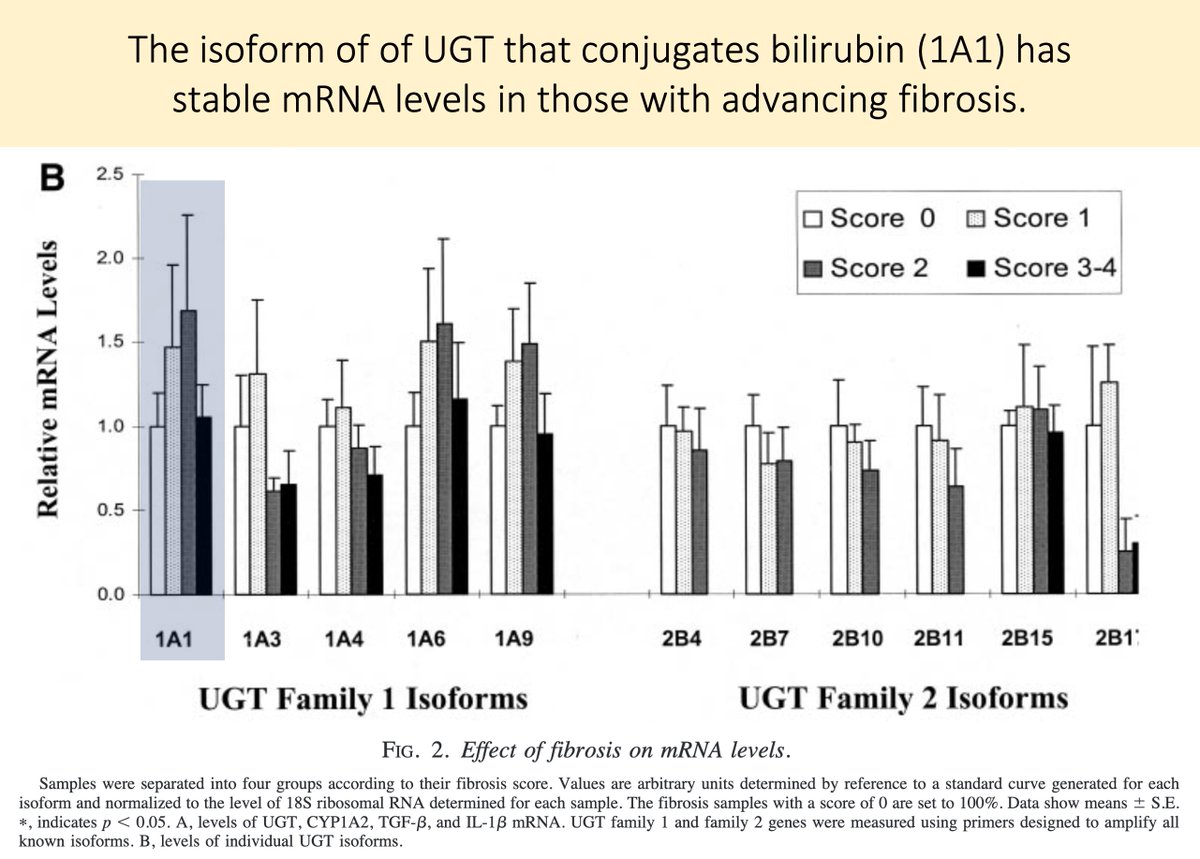
That UGT1A1 function remains despite liver disease explains the preserved ability to conjugate.
But why do these patients have conjugated hyperbilirubinemia? Why isn't it just cleared in the normal manner?
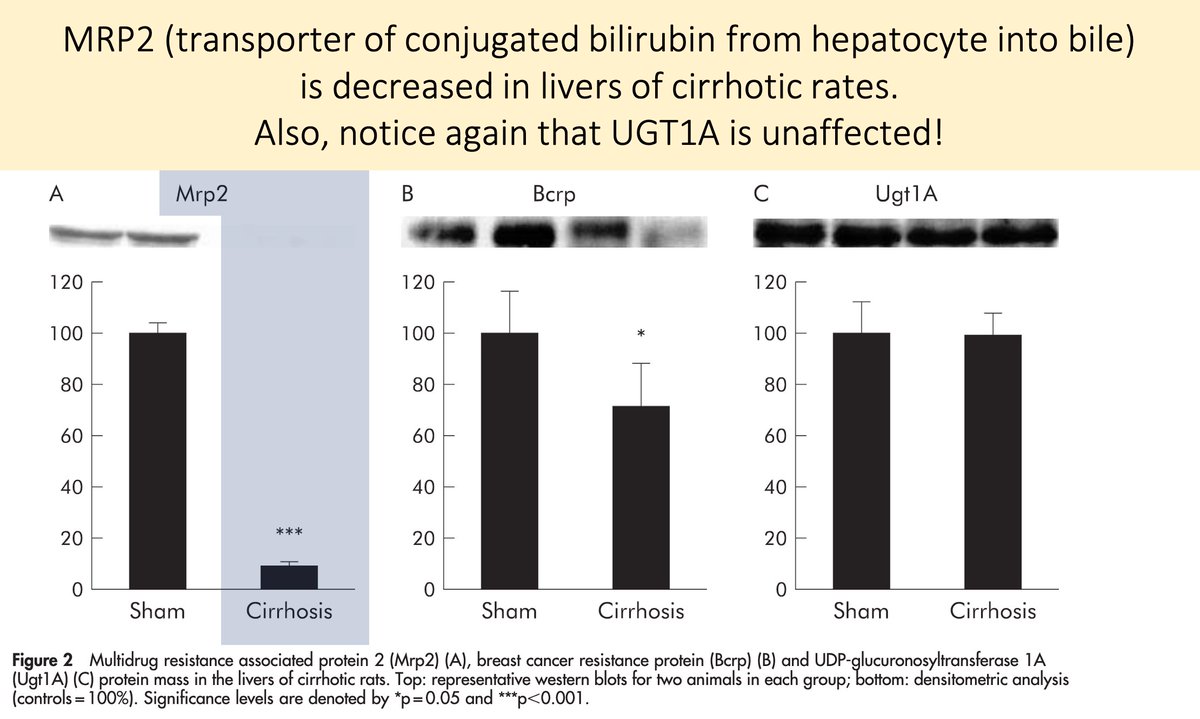
One problem is with the decreased transfer of bilirubin into bile.
Recall that MRP2 transports conjugated bilirubin from the hepatocyte into the bile.
Part of the explanation for conjugated hyperbilirubinemia in liver disease is DOWNregulation of MRP2.
This is best described in primary biliary cholangitis.
ncbi.nlm.nih.gov/pubmed/15542527
We have now explained why:
🔹Conjugation persists (stable UGT1A1)
🔹Conjugated bilirubin remains within hepatocytes (↓MRP2)
In order for a patient to have conjugated hyperbilirubinemia this conjugated bilirubin must somehow make it back into the blood.
We need more.
Interestingly, conjugated bilirubin is ROUTINELY secreted back into the sinusoidal blood by MRP3.
It is almost all reclaimed by hepatocytes via organic anion-transporting polypeptides (OATP).
The exact role of this "bilirubin hopping" is not clear.
ncbi.nlm.nih.gov/pubmed/24151358
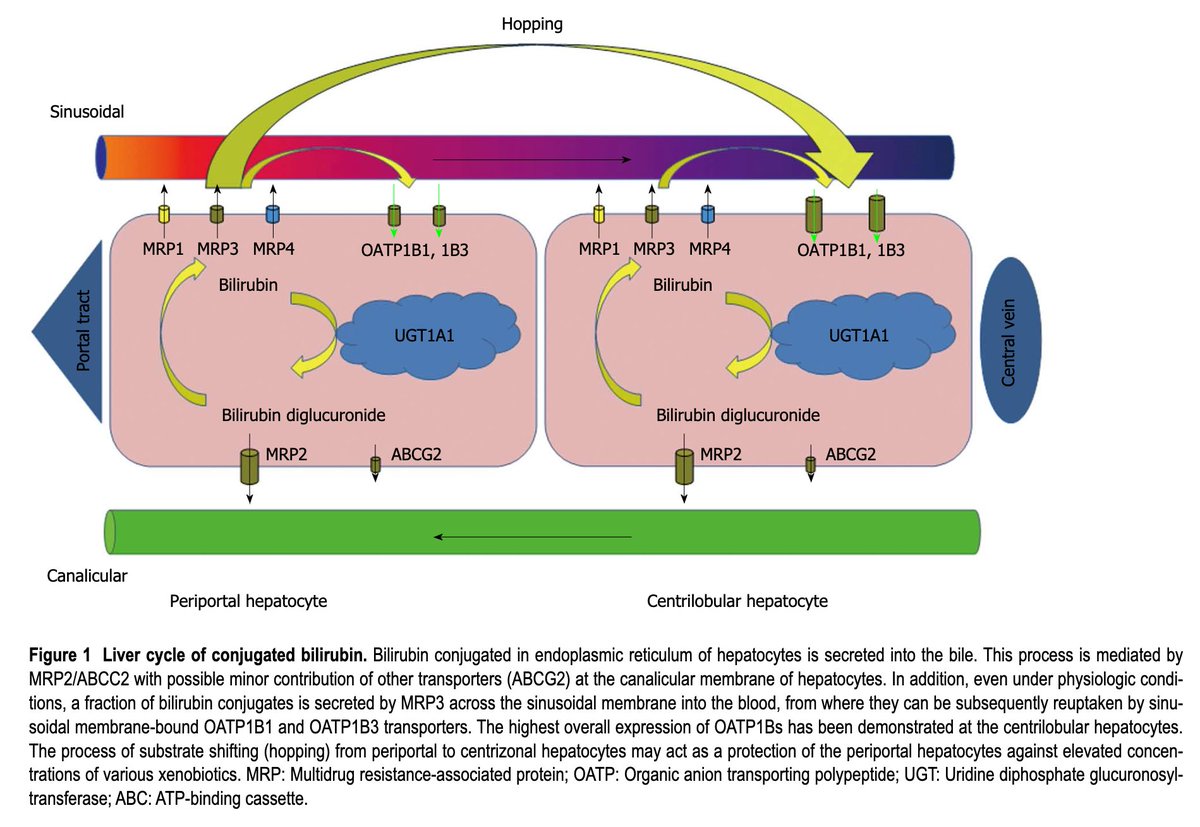
So, alongside the decrease in the usual portal of exit from the hepatocyte (MRP2) is there is concomitant:
↑MRP3
↓OATP
Thus: secretion and trapping of conjugated bilirubin in the blood
Result: conjugated hyperbilirubinemia!
ncbi.nlm.nih.gov/pubmed/11774951
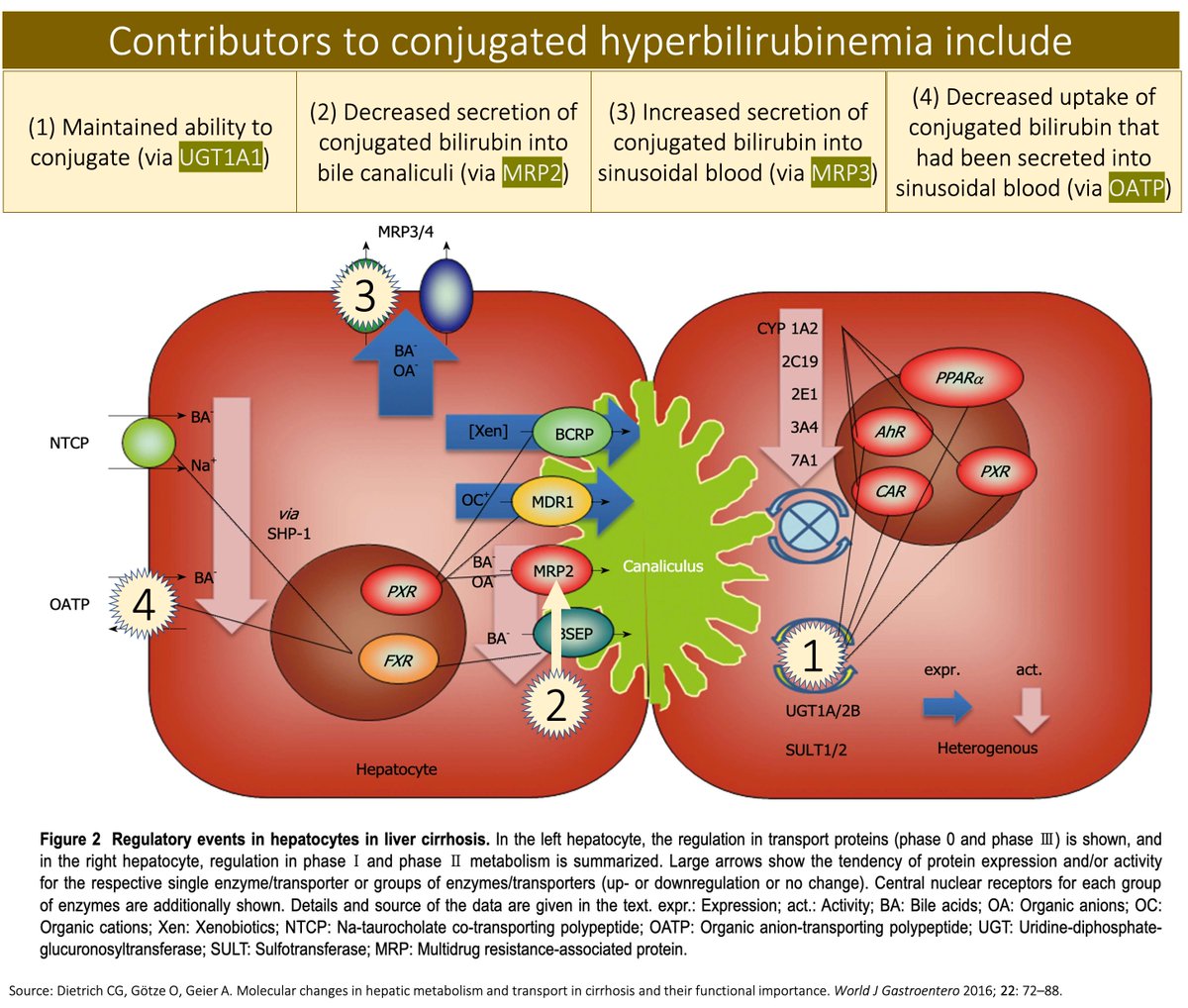
📣UGT1A1 conjugates bilirubin; this remains stable in liver disease
📣MRP2 transports conjugated bilirubin from hepatocytes into bile; this is ↓ in liver disease
📣As an alternative exit, conjugated bilirubin enters sinusoidal blood → conjugated hyperbilirubinemia!
🎗️Nneka Ufere (@NnekaUfereMD), GI Fellow, @MGH_GI
🎗️Elliot Tapper (@ebtapper), Hepatologist, @MichiganLiver
...for their peer review of this tweetorial!