How do diuretics lead to metabolic alkalosis?
I often invoke "contraction alkalosis", typically as a hand-wave explanation as patients' bicarbonate increases with diuresis.
Should I continue to wave my hands?
In order to understand the mechanism of alkalosis with diuresis, it is important to recall that there are at least two phases to any metabolic alkalosis (MA):
(1) Generation
(2) Maintenance
First, let's discuss the generation of MA with diuresis.
The idea of a "contraction alkalosis" comes from a 1965 paper in which diuresis was induced with ethacrynic acid (200mg daily).
The participants made a lot of urine (3-7 liters/day for 1-3 days).
ncbi.nlm.nih.gov/pubmed/14283394
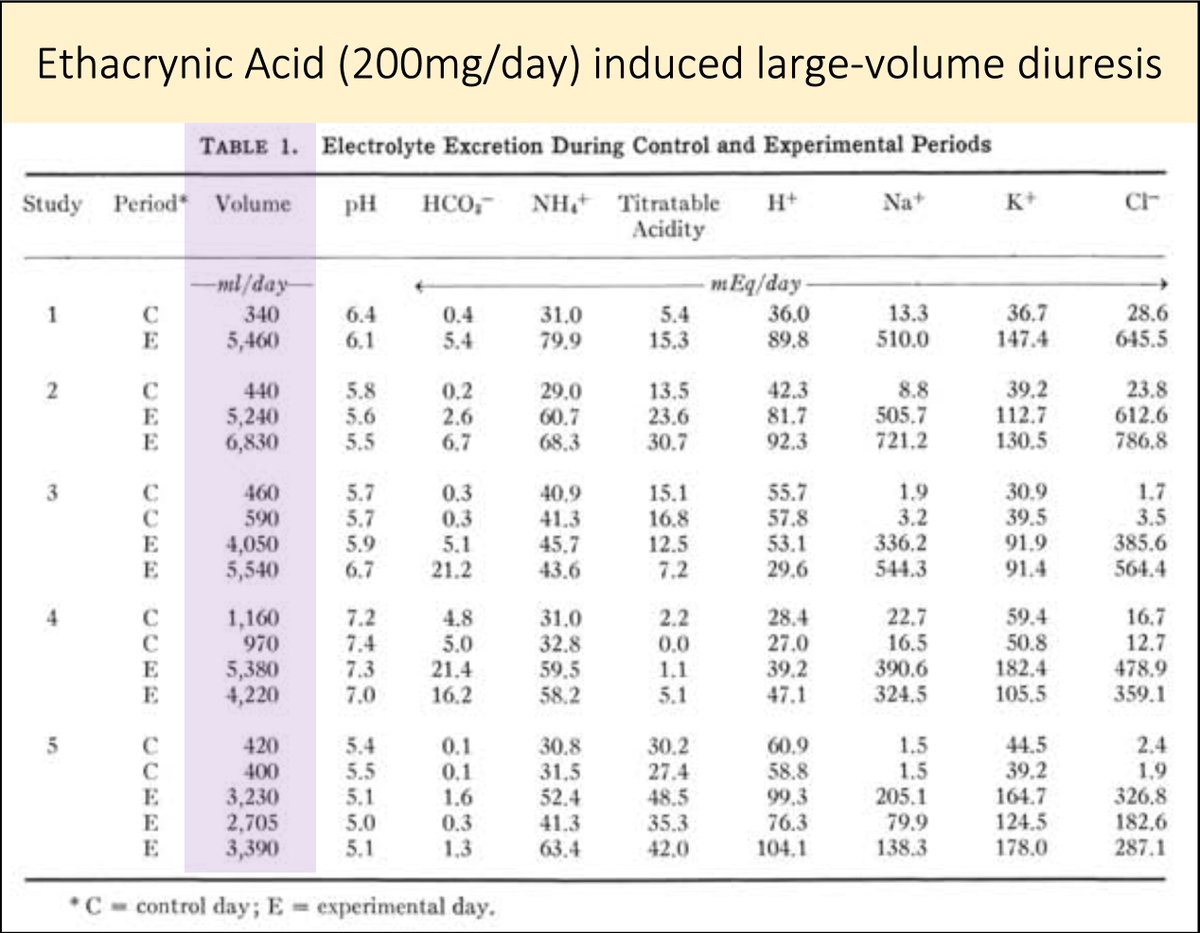
As water was lost, the fluid in the extracellular space "contracted" around an unchanged amount of bicarbonate.
The result: alkalosis
More specifically, what Cannon et al called "contraction alkalosis".
ncbi.nlm.nih.gov/pubmed/14283394
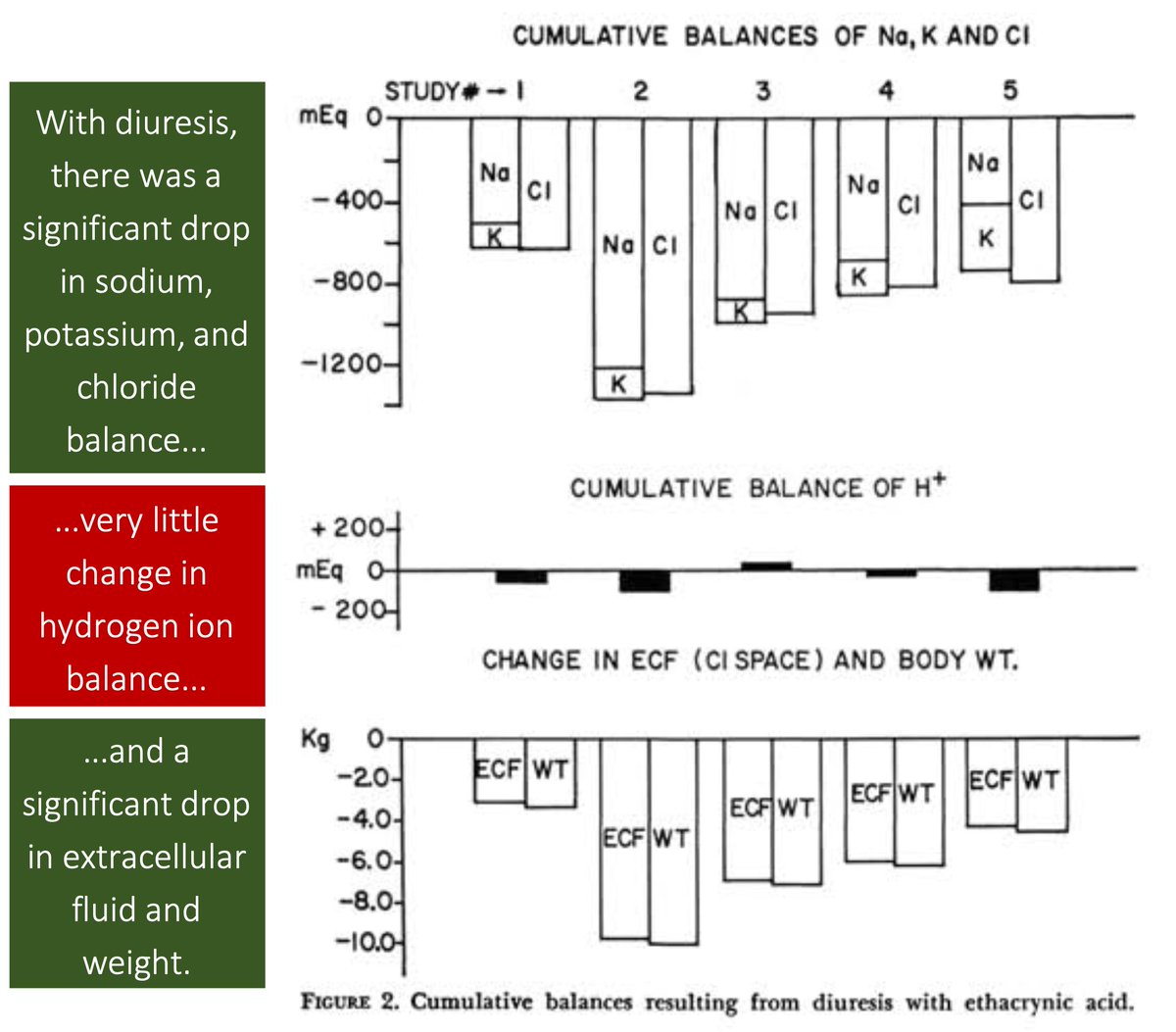
So, maybe aggressive diuresis is one way to GENERATE a metabolic alkalosis via contraction of the extracellular volume.
But, what MAINTAINS the metabolic alkalosis in these patients? [Poll]
[ECV = extracellular volume]
To understand the answer, recall that kidneys are VERY good at excreting excess bicarbonate.
In one study subjects were given 1000mEq of bicarb per day for 2 weeks.
They excreted nearly all the excess with only a small increase in serum HCO₃⁻.
ncbi.nlm.nih.gov/pubmed/13190687
This study suggests Key Point #1
🔑Maintenance of a metabolic alkalosis is always due to an inability of the kidney to excrete excess HCO₃⁻.
Let's examine the reasons why patients who have received diuretics may not be able to excrete excess HCO₃⁻.
There are a few things that may maintain MA. One is the extracellular volume depletion that diuretics may induce.
This leads to:
(1) ↓GFR, which leads to ↓filtered HCO₃⁻ and ↓excretion
(2) ↑tubular reabsorption of HCO₃⁻
But, volume depletion alone does not fully explain maintenance of MA.
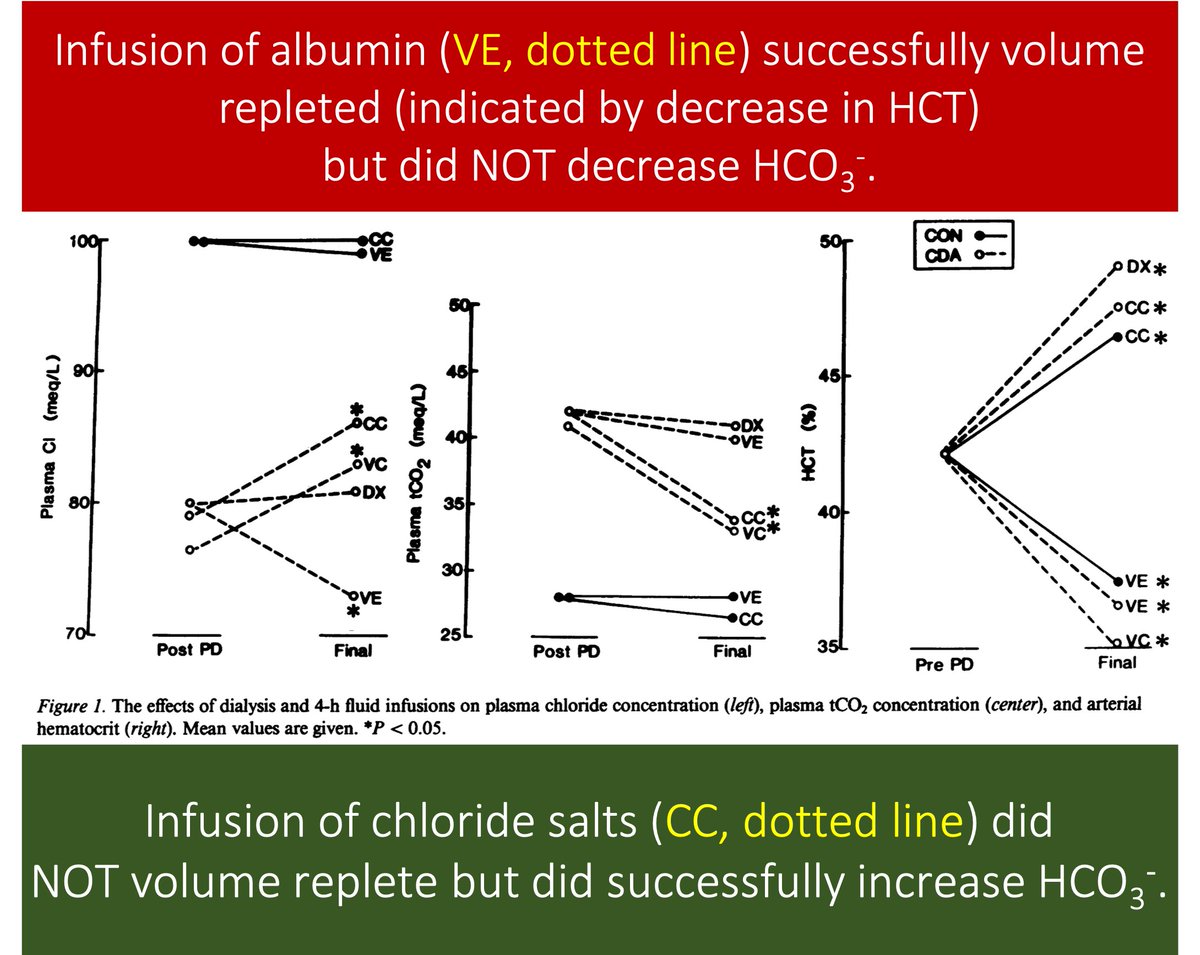
In one study, rats were volume expanded with albumin. This did NOT correct the MA. Chloride salts DID correct the MA, even though the rats remained volume depleted.
Cl⁻ matters.
ncbi.nlm.nih.gov/pubmed/3110214
Why does Cl⁻ matter?
One answer: pendrin.
And what is pendrin?
Pendrin is a Cl⁻/HCO₃⁻ exchanger in type-B intercalated cells within the cortical collecting duct.
ncbi.nlm.nih.gov/pubmed/25668022
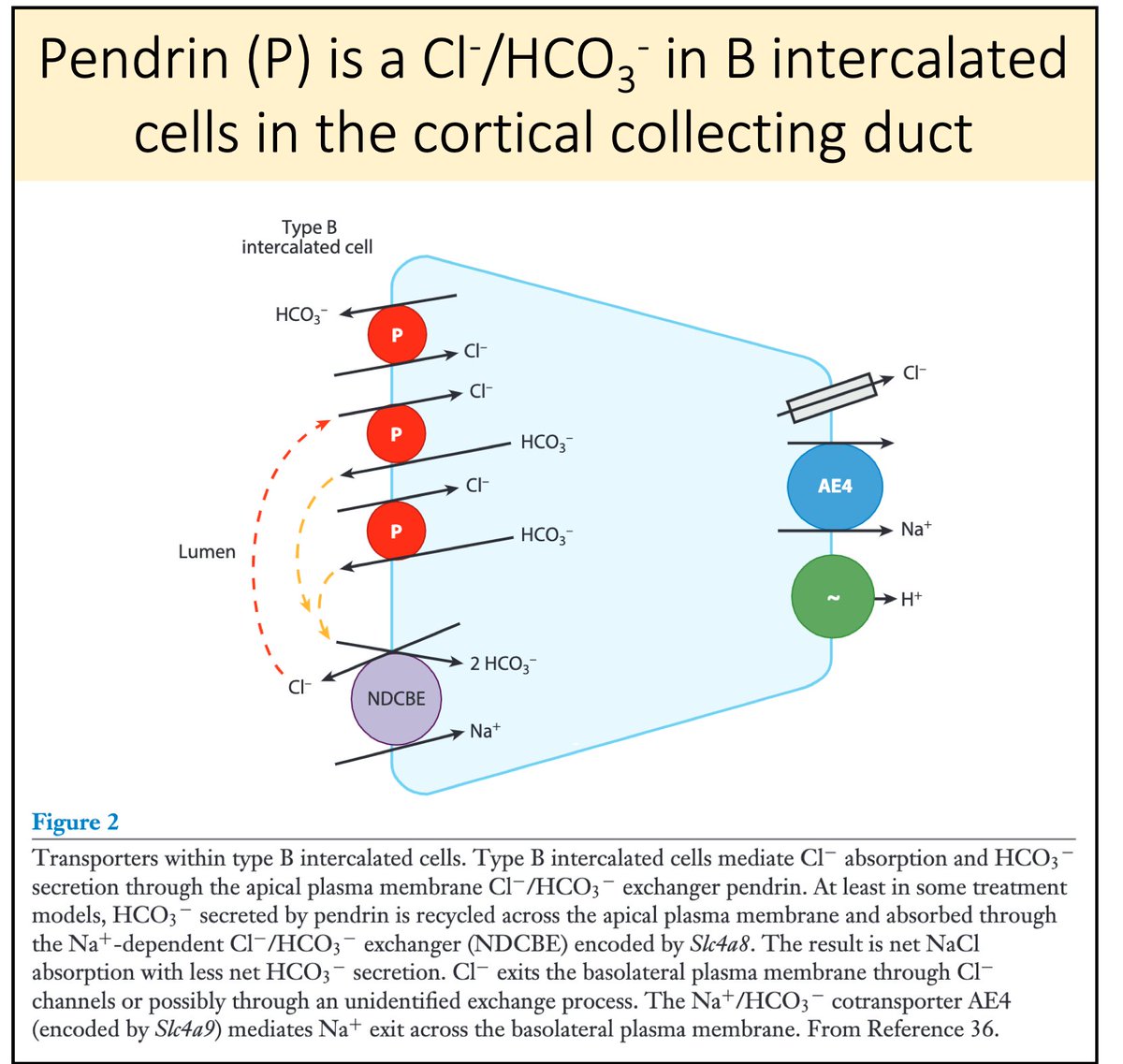
Key Point #2
🔑In order for pendrin to secrete HCO₃⁻, it must have luminal Cl⁻ to exchange it with.
In states of Cl⁻ depletion (e.g., post-diuresis), luminal Cl⁻ is NOT available and pendrin cannot secrete HCO₃⁻
Result: the MA is maintained.
ncbi.nlm.nih.gov/pubmed/22223876
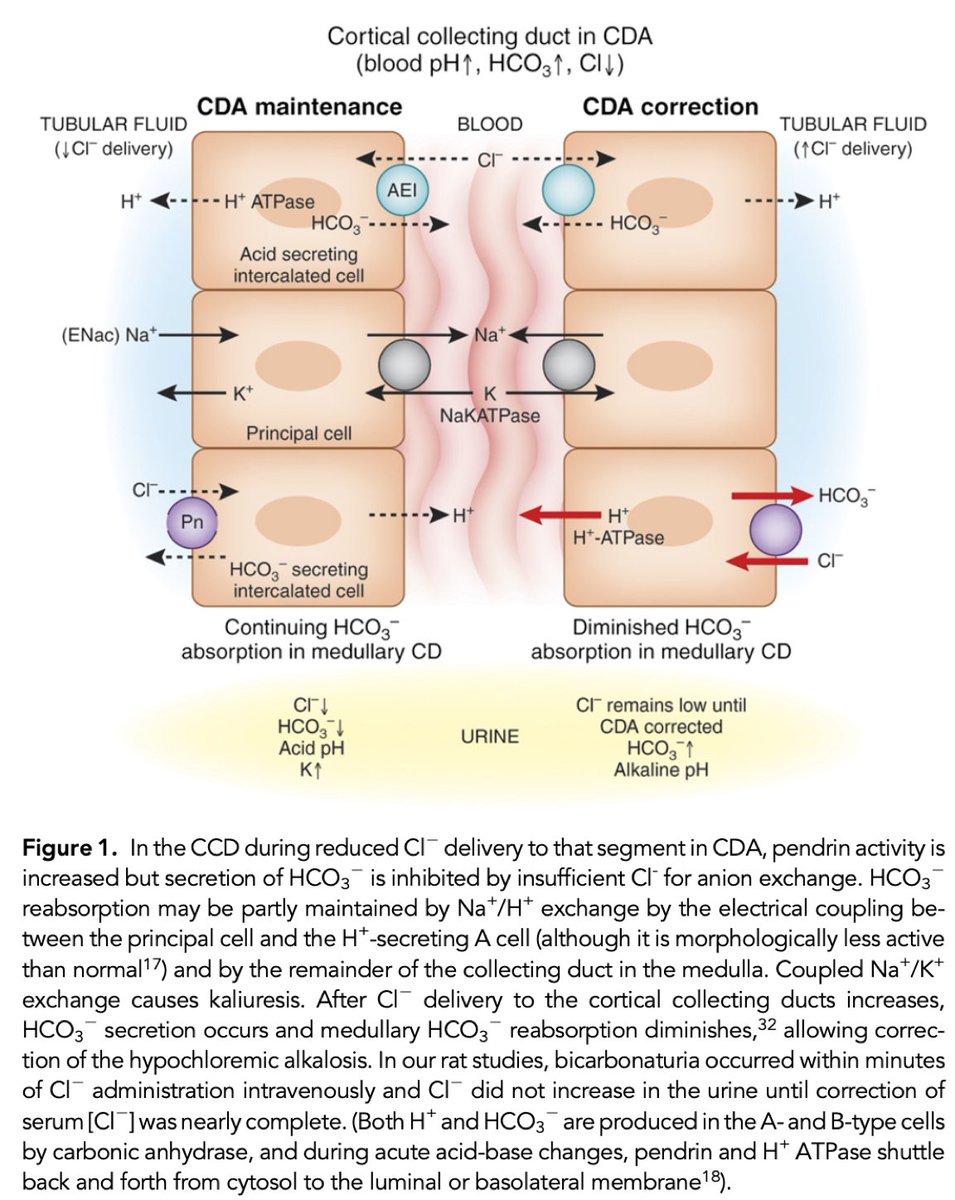
The role of pendrin helps explain why we stratify metabolic alkalosis using urinary chloride.
And why metabolic alkaloses are described as "chloride sensitive" or "chloride resistant".
One interesting clinical correlate:
Pendrin may be inactivated in cystic fibrosis, leading to metabolic alkalosis when volume depleted.
ncbi.nlm.nih.gov/pubmed/29482189
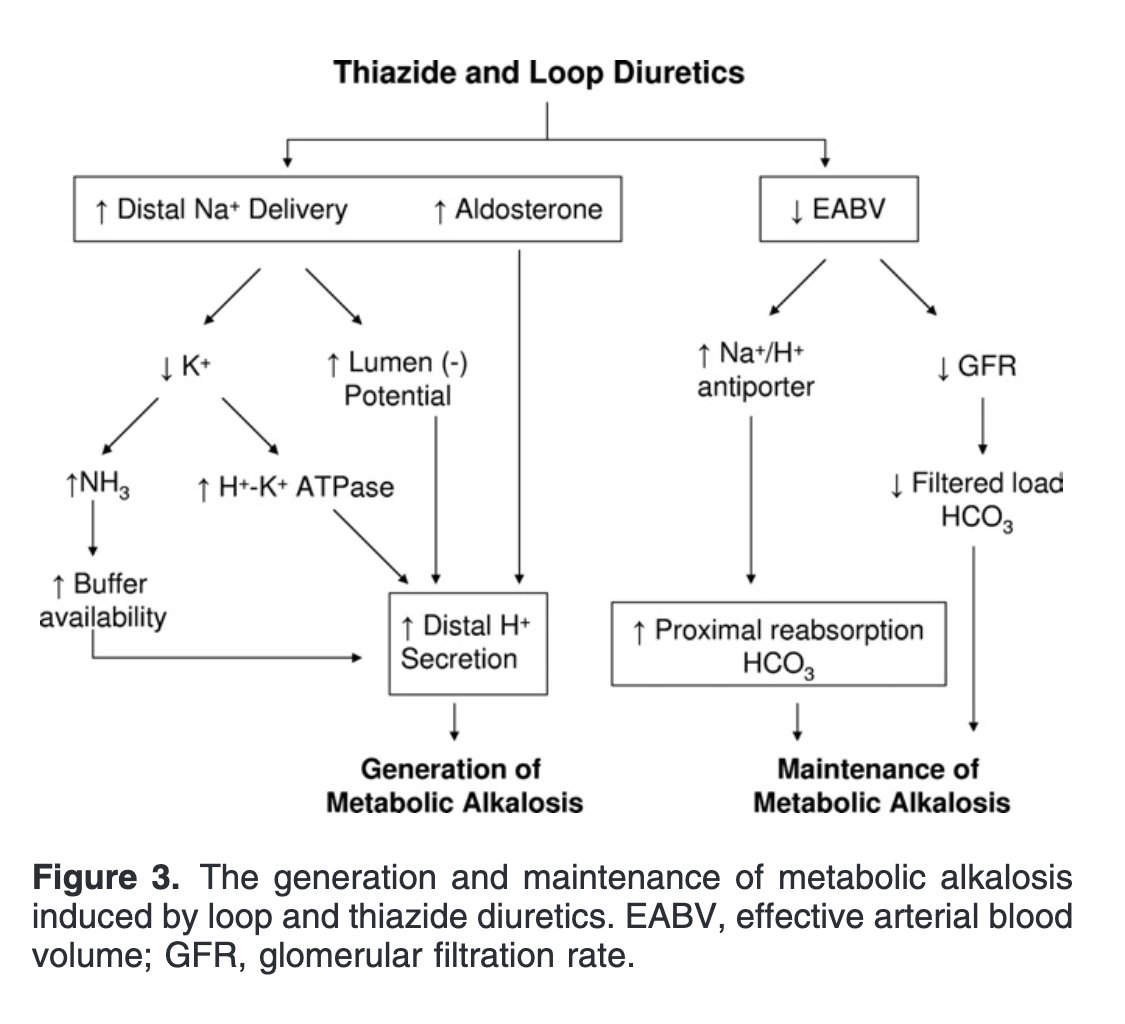
There are other effects of diuretics that help to generate and maintain metabolic alkalosis, including:
▪️hypokalemia
▪️distal sodium delivery
▪️increased aldosterone
ncbi.nlm.nih.gov/pubmed/22099511
🔹Contraction might generate metabolic alkalosis, but...
🔹...maintenance requires an inability of the kidney to excrete excess bicarbonate
🔹Chloride depletion maintains metabolic alkalosis as the exchange of Cl⁻ with HCO₃⁻ via pendrin is limited