Part 1/2
19/M fr Colorado +5 d fever, sudden-onset SOB. ER: 38.7, 60/40, 84%RA. Intubated. CXR +pulmonary edema. WBC 38K (60% N w/ marked immature cells, +atypical lymphs), Hgb 14/Hct 60%, Plt 78, ALT 90, n/l bili. Blood, BAL Cx’s (-), COVID, flu(-).
MCQ, exposures in Part 2/2
19/M fr Colorado +5 d fever, sudden-onset SOB. ER: 38.7, 60/40, 84%RA. Intubated. CXR +pulmonary edema. WBC 38K (60% N w/ marked immature cells, +atypical lymphs), Hgb 14/Hct 60%, Plt 78, ALT 90, n/l bili. Blood, BAL Cx’s (-), COVID, flu(-).
MCQ, exposures in Part 2/2

Part 2/2 case continued..
2 wks ago, was renovating a rodent-infested house in a farm that grazed cattles. 1 wk ago, +tick/mosquito bites during a hike. Also reported his roommate had fever/cough a few days prior. What is the most likely source of transmission of this infection?
2 wks ago, was renovating a rodent-infested house in a farm that grazed cattles. 1 wk ago, +tick/mosquito bites during a hike. Also reported his roommate had fever/cough a few days prior. What is the most likely source of transmission of this infection?
1/8
The majority got this right, rodents 🐀. As everyone pointed out, this is a case of hantavirus pulmonary syndrome (HPS or cardiopulmonary syndrome HCPS).
5️⃣ things to know about hantavirus (specifically HPS) in the next tweets.
The majority got this right, rodents 🐀. As everyone pointed out, this is a case of hantavirus pulmonary syndrome (HPS or cardiopulmonary syndrome HCPS).
5️⃣ things to know about hantavirus (specifically HPS) in the next tweets.
2/8
1️⃣ Transmitted from rodents 🐀 (like many other infections 👇)
▪️ shed in the urine, feces, saliva & spread via aerosol
▪️ indoor exposure to rodent-infested buidling most important
▪️ person-person transmission doesn’t occur (except Andes)
@TxID_Edu @rabihmgeha @DxRxEdu
1️⃣ Transmitted from rodents 🐀 (like many other infections 👇)
▪️ shed in the urine, feces, saliva & spread via aerosol
▪️ indoor exposure to rodent-infested buidling most important
▪️ person-person transmission doesn’t occur (except Andes)
@TxID_Edu @rabihmgeha @DxRxEdu
3/8
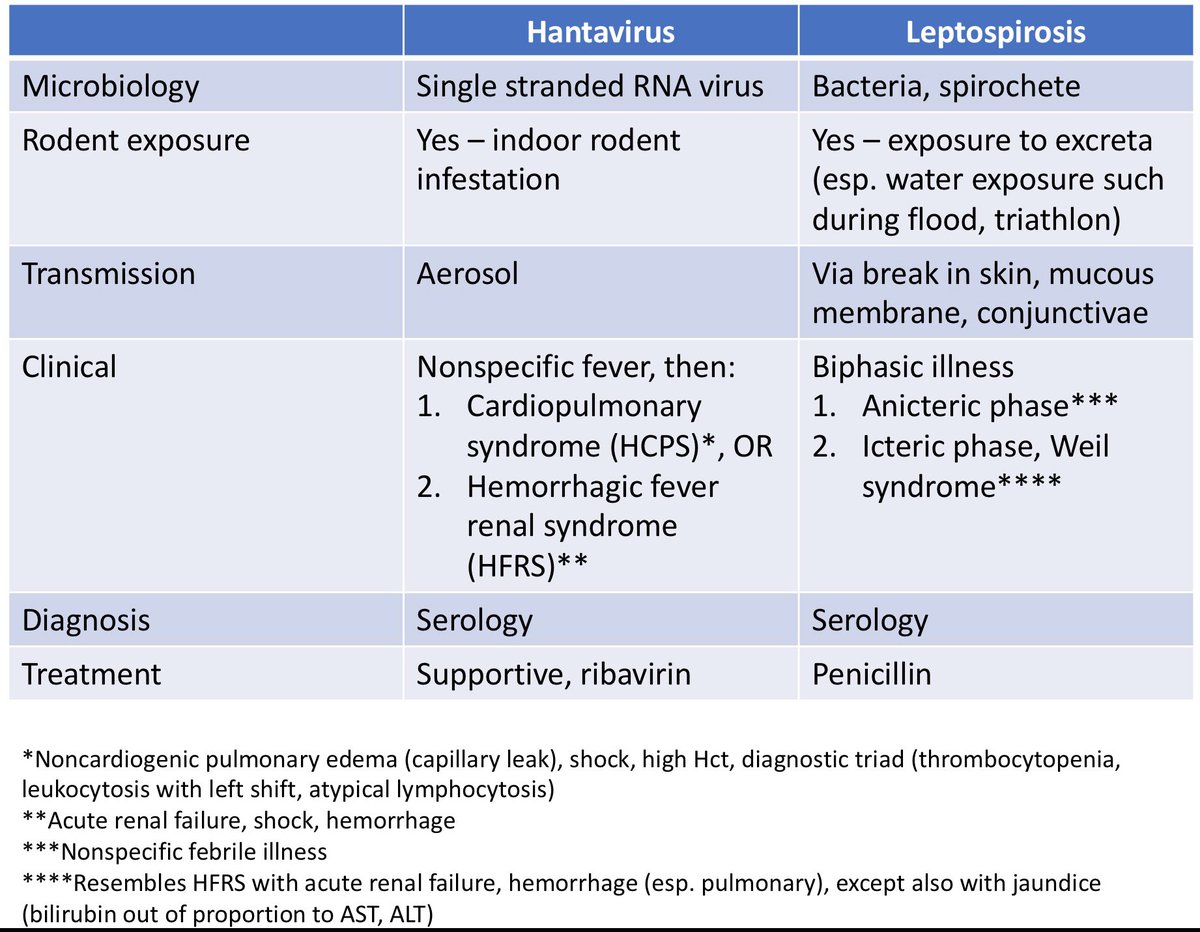
2️⃣ 2 major forms:
▪️HPS (case presented here): Sin Nombre, Andes virus
▪️Hemorrhagic fever with renal syndrome (HFRS): Hantaan, Dobrava, Puumala (nephropathia epidemica)
@arauseomd @FrannyBoly @NNolanMD @Jncherabie
2️⃣ 2 major forms:
▪️HPS (case presented here): Sin Nombre, Andes virus
▪️Hemorrhagic fever with renal syndrome (HFRS): Hantaan, Dobrava, Puumala (nephropathia epidemica)
@arauseomd @FrannyBoly @NNolanMD @Jncherabie
4/8
3️⃣ Clinical findings:
▪️Incubation: 2-3 wks
▪️Starts as nonspecific fever (myalgia, headache, abdominal pain can be severe), URI sx rare
▪️After 1 wk, differentiates into either HFRS (AKI, shock, hemorrhage) or HPS
3️⃣ Clinical findings:
▪️Incubation: 2-3 wks
▪️Starts as nonspecific fever (myalgia, headache, abdominal pain can be severe), URI sx rare
▪️After 1 wk, differentiates into either HFRS (AKI, shock, hemorrhage) or HPS
5/8
Hanta pulmonary sx (HPS)
⚡️ Heralded by dry cough, SOB 👉 respiratory failure (noncardiogenic pulm edema 2/2 pulm capillary leak), shock (renal failure mild)
⚡️ High Hct, diagnostic triad (low plt, leukocytosis w/ left shift, atypical lymphocytosis) 👉 unique in ID‼️
Hanta pulmonary sx (HPS)
⚡️ Heralded by dry cough, SOB 👉 respiratory failure (noncardiogenic pulm edema 2/2 pulm capillary leak), shock (renal failure mild)
⚡️ High Hct, diagnostic triad (low plt, leukocytosis w/ left shift, atypical lymphocytosis) 👉 unique in ID‼️
6/8
bit.ly/3c9mCHz
In this study, in the right epidemiological and clinical setting, 4 of 5 labs findings has Sn 96% and Sp 99% for HPS:
✔️low plt
✔️left shift
✔️hemoconcentration
✔️lack of toxic granulation
✔️10% lymphocytosis
bit.ly/3c9mCHz
In this study, in the right epidemiological and clinical setting, 4 of 5 labs findings has Sn 96% and Sp 99% for HPS:
✔️low plt
✔️left shift
✔️hemoconcentration
✔️lack of toxic granulation
✔️10% lymphocytosis
7/8
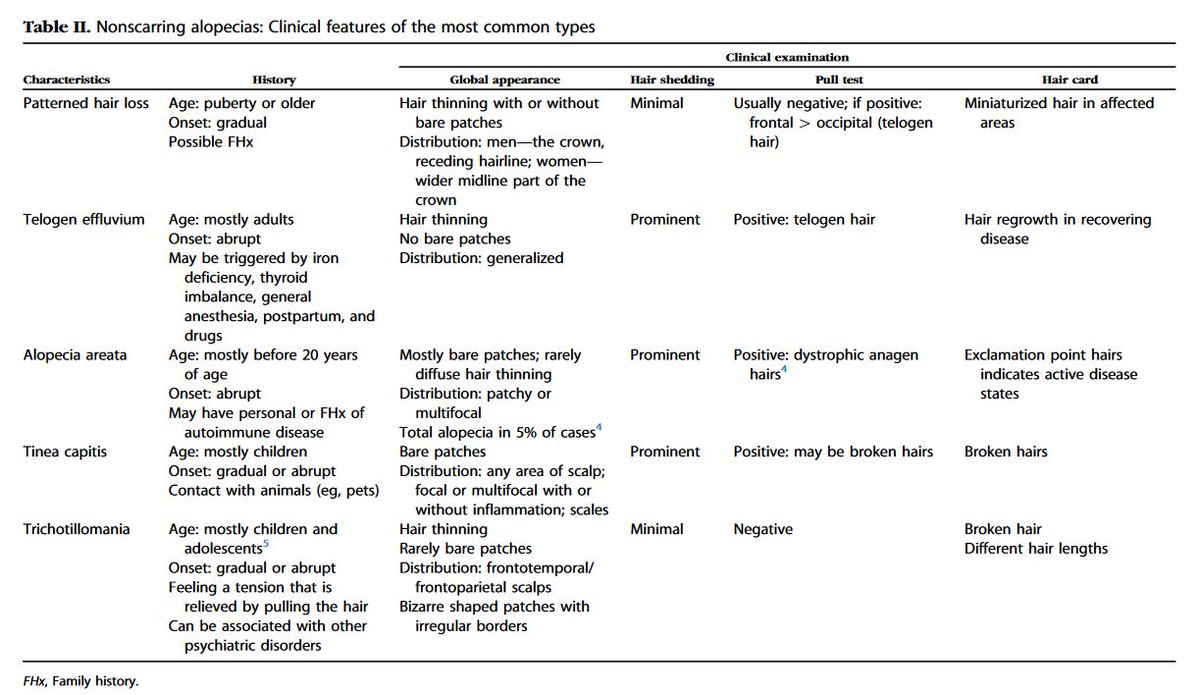
4️⃣ Resembles leptospirosis in many ways. See table 👇 for comparison.
Resembles dengue: high Hct, low plt, capillary leak
Resembles #COVID19: dry cough, resp failure after prodrome, rare URI sx, ARDS (pulmonary-renal sx vs ⚡️Hanta w/c is pulmonary OR renal sx)
4️⃣ Resembles leptospirosis in many ways. See table 👇 for comparison.
Resembles dengue: high Hct, low plt, capillary leak
Resembles #COVID19: dry cough, resp failure after prodrome, rare URI sx, ARDS (pulmonary-renal sx vs ⚡️Hanta w/c is pulmonary OR renal sx)
8/8
5️⃣ Serology (+IgM, or 4x rise in IgG) is the main diagnostic method; available at state labs. Treatment is supportive. Ribavirin works for HFRS but equivocal effect in HPS. No role of steroids. Cautious IV fluids (2/2 capillary leak, like dengue).
5️⃣ Serology (+IgM, or 4x rise in IgG) is the main diagnostic method; available at state labs. Treatment is supportive. Ribavirin works for HFRS but equivocal effect in HPS. No role of steroids. Cautious IV fluids (2/2 capillary leak, like dengue).
• • •
Missing some Tweet in this thread? You can try to
force a refresh