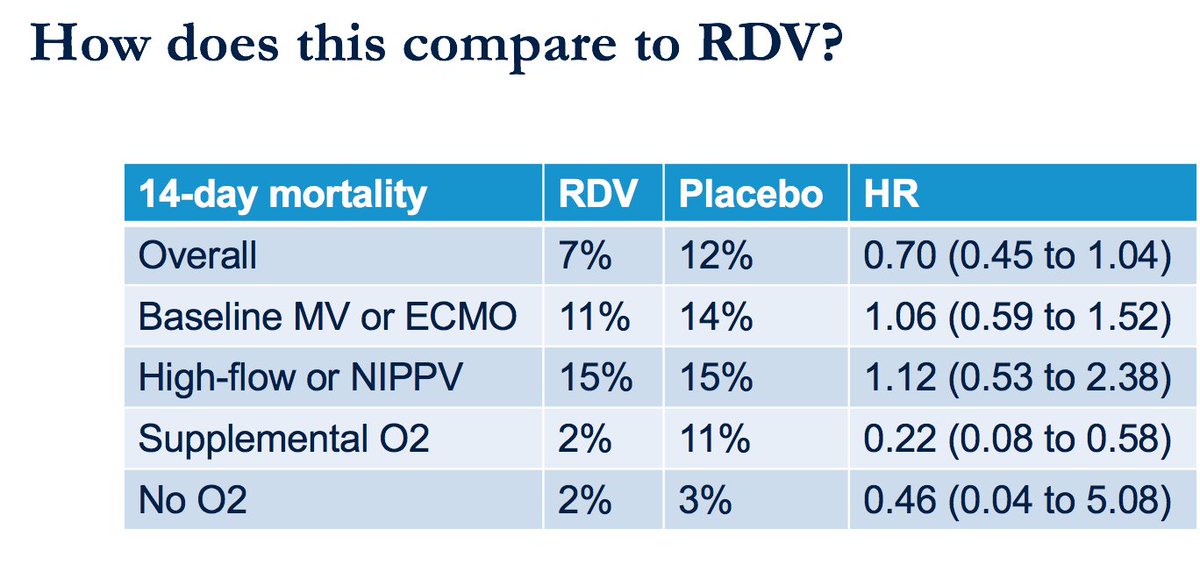
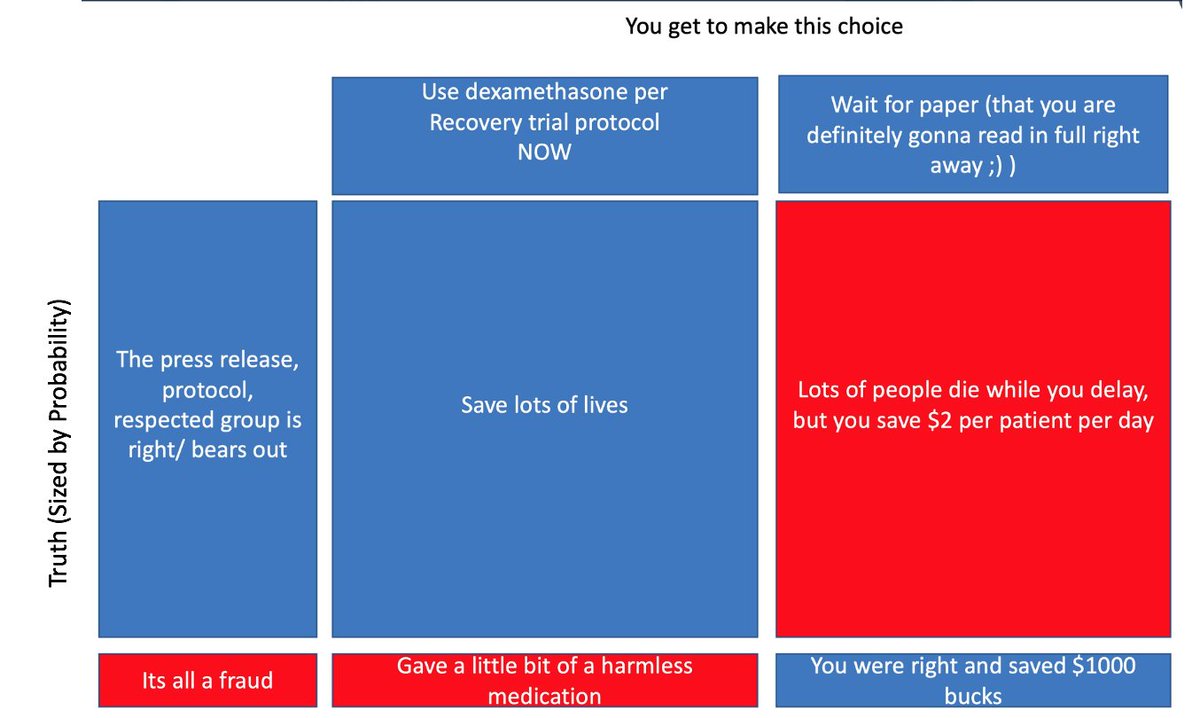
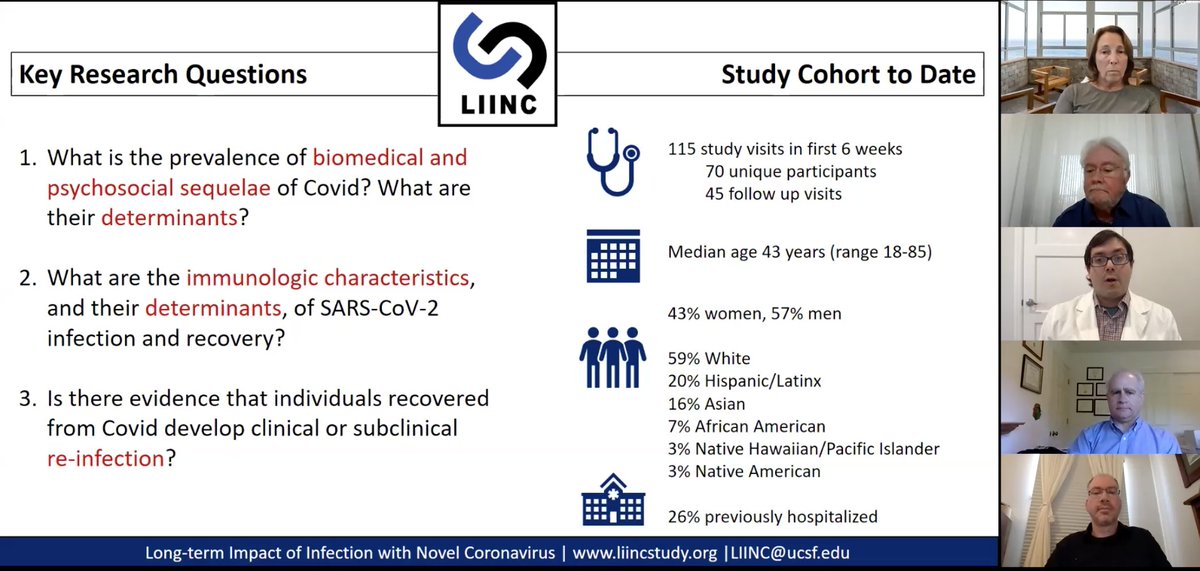
Grand Rounds today, available here: Today we cover two hot topics: 1) New data on therapies (including news on dexamethasone) & 2) Covid patients w/ persistent symptoms.
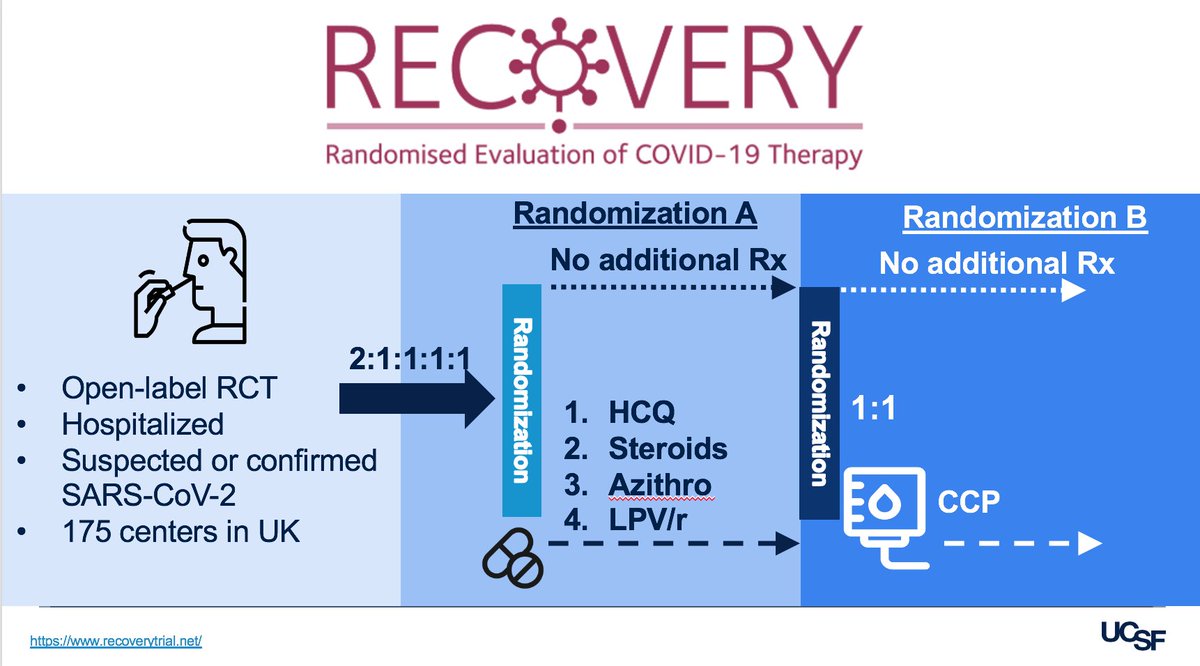
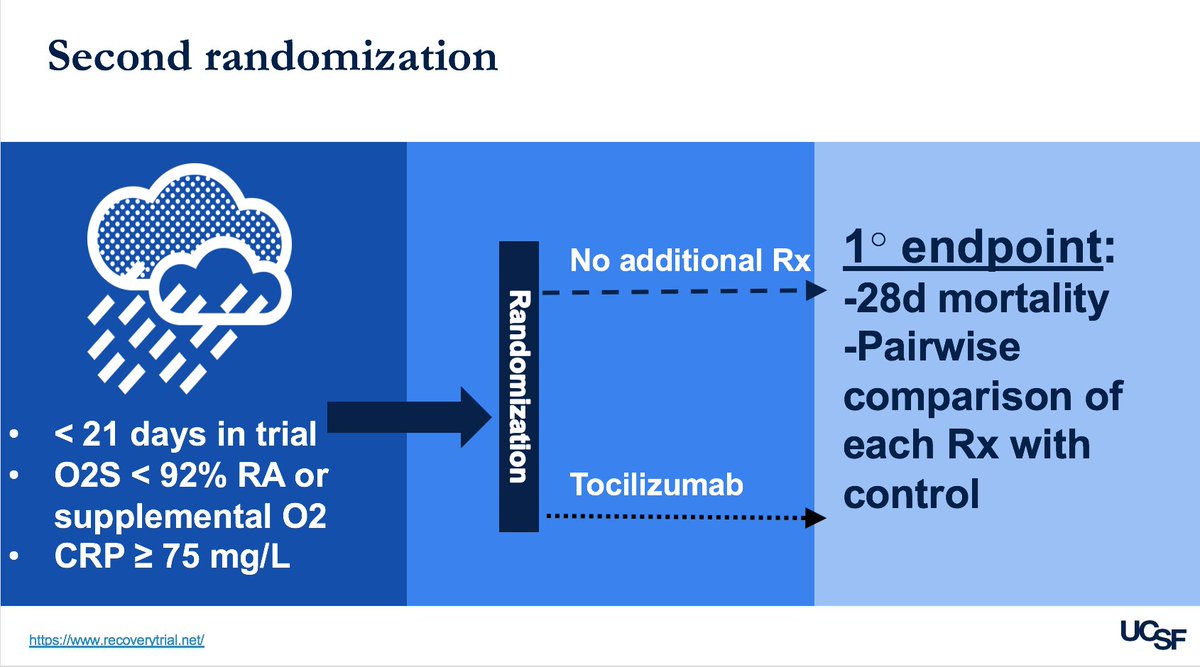
– hugely complex design. Patients randomized to 1 of 4 arms: HCQ, steroids (dex), azithromycin, or Lopinavir/Ritonavir. Then 2nd randomization to convalescent plasma or not, then 3rd (!) to Tocilizumab or not. Wow.

Again, hope you have a chance to watch this terrific Grand Rounds:
Back tomorrow with weekly update. Stay safe.