
My first thread-wish me luck! More on why Medicaid expansion is important for maternal #healthequty
Medicaid covers 25-50% of births in the US and is the largest single-payer of maternity care; Medicaid disproportionately covers low-income women & racial/ethnic minorities. Regarding Medicaid and maternal health, there are two separate/equally important issues.
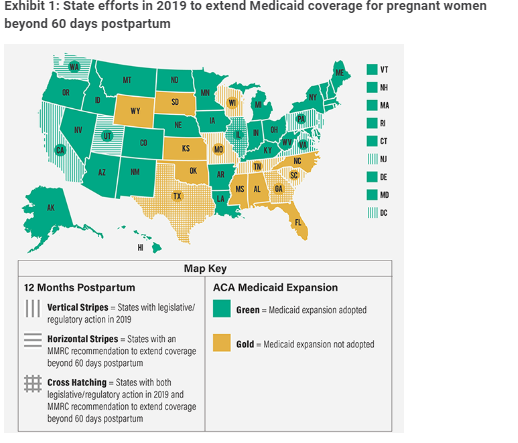
#1 Expansion of eligibility criteria,"Medicaid expansion". Medicaid coverage lasts up to 60 days postpartum, in non-expansion states, after this time is up, women must requalify for Medicaid as low-income parents; this is harder to do & results in coverage "churn"/ coverage gaps
Medicaid expansion decreases coverage churn, but beyond that does it matter? Some evidence from Gordon et. al to suggest that medicaid expansion may improve coverage stability and ⬆️use of Medicaid-financed outpatient care postpartum .…lthaffairs-org.proxy1.library.jhu.edu/doi/full/10.13…
But perhaps the most important benefit of Medicaid expansion is demonstrated in study by @eleliason @WHIjournal: Medicaid expansion associated w/⬇️ maternal mortality by 7.01 maternal deaths per 100,000 live births (p = .002); Effects concentrated among Black mothers. 

But is Medicaid expansion enough? Even in the post ACA era, where many states have expanded Medicaid, women still experience coverage churn ( albeit less than in non-expansion states)
healthaffairs.org/do/10.1377/hbl…
Which brings me to #2 extension of benefit coverage time
healthaffairs.org/do/10.1377/hbl…
Which brings me to #2 extension of benefit coverage time
Currently, Medicaid coverage stops 60 days postpartum. This is not insignificant, in a "Report of 9 Maternal Mortality review committees", 18% of deaths occurred after 42 days postpartum. This varies widely by state. In 2018 Texas reported 56% of deaths AFTER 60 days postpartum.
So there is some clear potential benefit of increasing access during the 1st year postpartum & several states have been working on this, in a recent report @emilyanneck @Health_Affairs gives an overview of the legislative landscape/including federal bills.healthaffairs.org/do/10.1377/hbl…. 
As a researcher focused on maternal health equity, I know that Medicaid expansion is just 1 lever & several more need pulling! Excited about the Black Maternal health #Momnibus act by @RepAdams @KamalaHarris @LaurenUnderwood. 9 bills to try & address this maternal health crisis.
Mortality=worst & thankfully rarest outcome. Many more have severe maternal morbidity which can impact long-term health/wellbeing & can also present after 60 days. Also patients w/ medical complications of pregnancy benefit from close follow up w/ primary care in the 1st year
• • •
Missing some Tweet in this thread? You can try to
force a refresh


