1/9 Big recent updates to #VitaminD #COVID19 evidence & thus now also to my review agingbiotech.info/vitamindcovid19: 3 highly cited preprints are out but even better studies replace them, including finally a large study of records from a big org. Main take-homes remain the same. Details:
2/9 2 preprints including very cited n=780 Indonesian study now withdrawn from SSRN. Another (Alipio's) suspected of being fraud. Details in section 9 of the review. All 3 removed from my 1pager summary agingbiotech.info/vitamindcovid1…. I now apply a new standard for preprints with data:
3/9 For preprints with D & C19 case data, I only include if author affiliations can be web-verified & authors have relevant pre-2020 publication records. With the 3 preprints removed, the evidence was still compelling. Now I've added 3 additional studies to the 1pager & review:
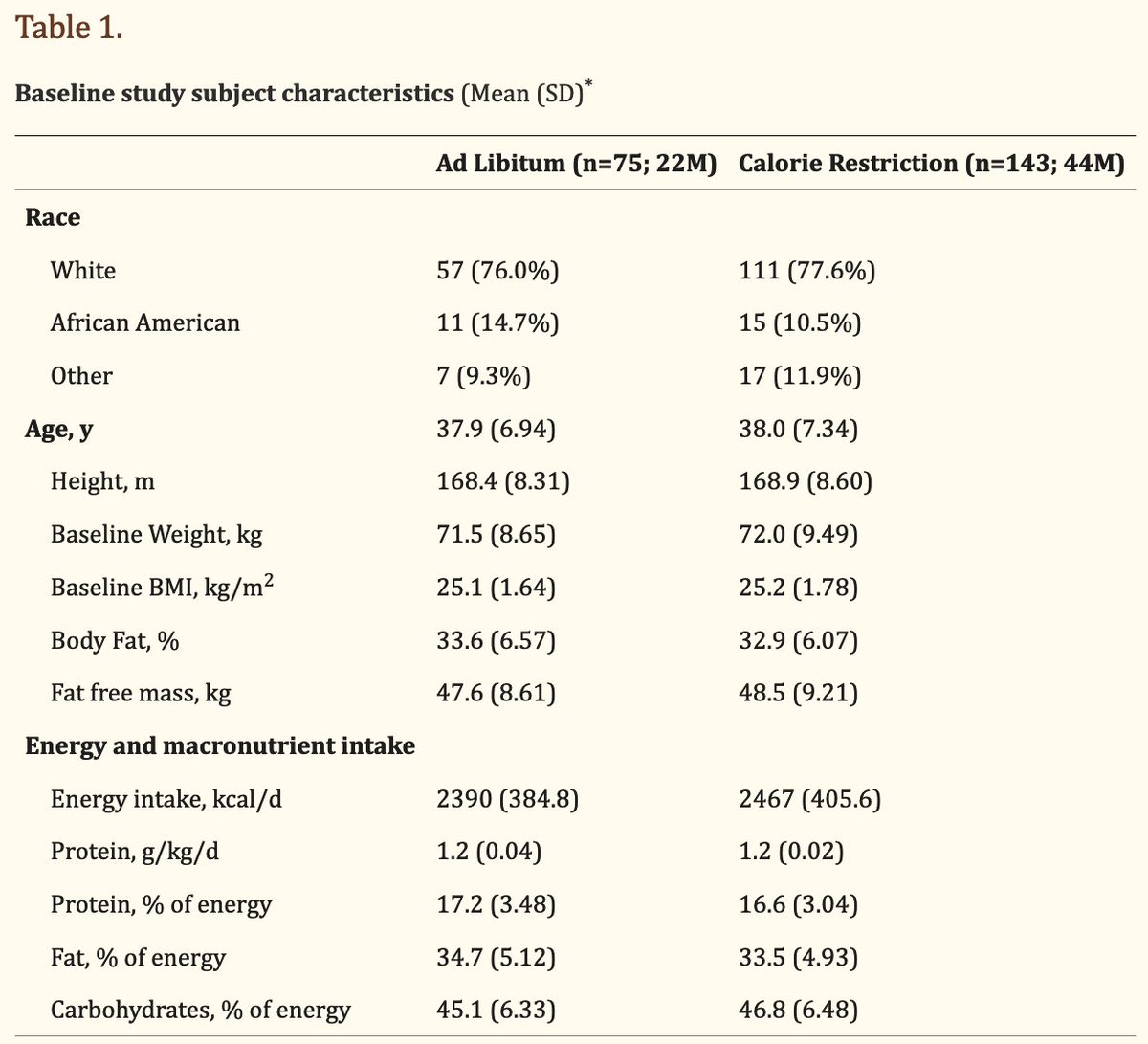
4/ On low-D correlation to C19 severity: Merzon etal's Israel study of 782 C19+ cases & De Smet etal's Belgium study of 186 cases now added to Panagioteu etal's UK study of 134 cases (& the handful of n<50 studies). Now 1100+ cases w/ low-D correlated to 3 measures of severity:
5/9 hospitalization vs. not, intensive-treatment-unit admission vs. only hospitalization, & chest CT categorization of severity. Together the data suggests low D worsens progression at multiple disease stages. See section 8. Already strong causality evidence also a bit better:
6/ Added Kohlmeier's Mendelian randomization study, which is 1-step better than typical group correlation studies by considering race & latitude. Confounders that could explain this data seem far less likely (eg racial economic disadvantages worsening w/ latitude moving north).
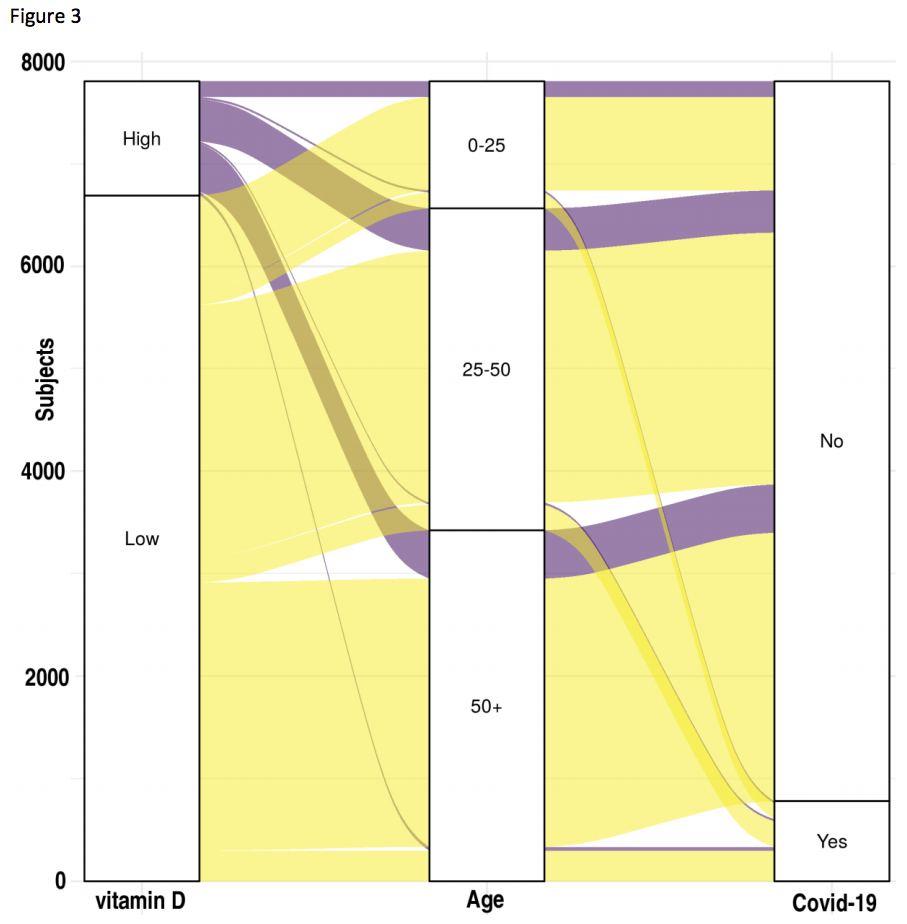
7/9 Merzon's study worth special attention as the 1st study from an org w/ many records. 14k/730k patients C19 tested, 7807/14k had 25OHD. Controlling for more confounders than any other studies so far, adjusted OR of infection 1.5 & OR of hospitalization if infected 1.95. So
8/9 overall low D patients had ~3x odds of hospitalization for C19. On low-D correlation to infection risk (vs case severity): With D'Avolio's & Meltzer's studies overall evidence now tilted against Hastie's & Darling's UK Biobank papers w/ the too-old D tests. See section 11.
9/9 Merzon's Fig-3 shows how few D>30ng/ml cases get hospitalized, esp. at younger ages. How many fewer deaths if everyone had adequate D? More orgs w/ many patient records need to publish data like this & add later measures of severity/outcome. NHS, Kaiser, VA, etc. Who's next? 
• • •
Missing some Tweet in this thread? You can try to
force a refresh