Tweetorial alert📢
Hello, #nephtwitter, we hope you enjoyed our latest blog post
renalfellow.org/2020/07/20/ske…
Let’s talk all about Low Salt Diet & Ca handling in kidney stones. Are you ready ⁉️
💥#kidneystones #lowsaltdiet #dietmatters #theskeletonKG #NSMCInternship #podkopiluwak💥
Hello, #nephtwitter, we hope you enjoyed our latest blog post
renalfellow.org/2020/07/20/ske…
Let’s talk all about Low Salt Diet & Ca handling in kidney stones. Are you ready ⁉️
💥#kidneystones #lowsaltdiet #dietmatters #theskeletonKG #NSMCInternship #podkopiluwak💥
2/ Kidney stones 🪨 💎🔶♦️💠are a worldwide issue with increasing prevalence. Calcium stones (oxalate > phosphate) - most common (75%).
📍Which of the following contribute to stone formation?
📍Which of the following contribute to stone formation?
3/ All the above.
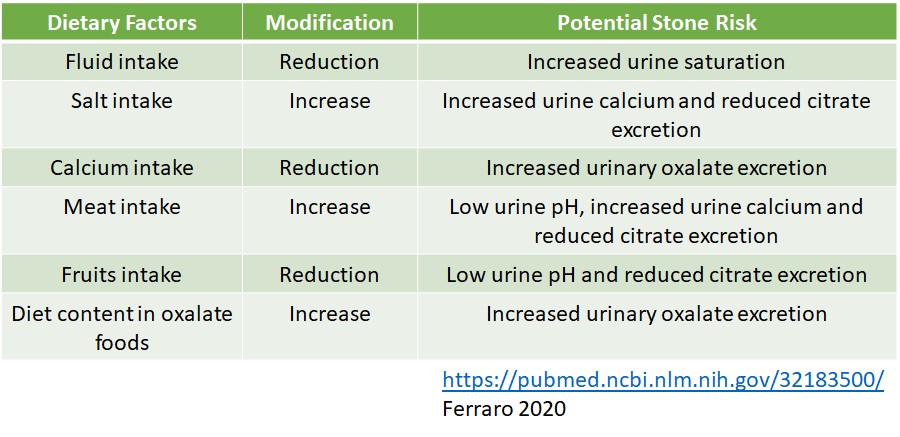
Nevertheless, dietary factors are modifiable.
Look, now we have some control, eh...🤓🦾
Nevertheless, dietary factors are modifiable.
Look, now we have some control, eh...🤓🦾
4/Let's focus on Salt🧂:
⬆️dietary intake of NaCl🧂 → ⬆️ urinary Ca
📌1 teaspoon of NaCl (2.3 g of Na) → urinary calcium excretion by 40 mg/day
pubmed.ncbi.nlm.nih.gov/7666985/
📌dietary salt intake >10 g/day → increased prevalence of hypercalciuria
pubmed.ncbi.nlm.nih.gov/9092314/
⬆️dietary intake of NaCl🧂 → ⬆️ urinary Ca
📌1 teaspoon of NaCl (2.3 g of Na) → urinary calcium excretion by 40 mg/day
pubmed.ncbi.nlm.nih.gov/7666985/
📌dietary salt intake >10 g/day → increased prevalence of hypercalciuria
pubmed.ncbi.nlm.nih.gov/9092314/

5/ Maximum RDA for NaCl intake - 2.3 g/day. (WHO: <5g/day)
📌Low salt diet ⬇️ calciuria (RCT)
pubmed.ncbi.nlm.nih.gov/14519796/
📌Prospective follow-up study - DASH diet ⬇️ kidney stones pubmed.ncbi.nlm.nih.gov/19679672/
This is difficult to achieve as the common food additive/ preservative is🧂
📌Low salt diet ⬇️ calciuria (RCT)
pubmed.ncbi.nlm.nih.gov/14519796/
📌Prospective follow-up study - DASH diet ⬇️ kidney stones pubmed.ncbi.nlm.nih.gov/19679672/
This is difficult to achieve as the common food additive/ preservative is🧂
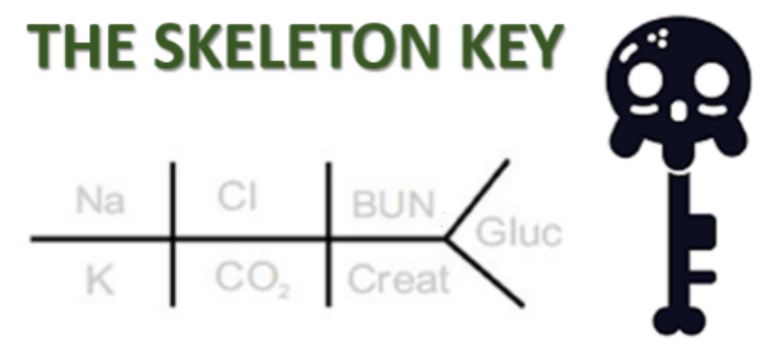
7/ Before understanding the mechanism of salt-induced calciuria, let’s understand the mechanism of Ca transport.
Quiz time: Where is Ca absorbed in the Nephron?
Quiz time: Where is Ca absorbed in the Nephron?
9/ What is the predominant mechanism of Ca+2 absorption in PT?
10/ Ans: Paracellular
📍PT and the thick ascending limb (TAL) of the loop of Henle - mostly paracellular (depends on transepithelial electrochemical gradient & tight junction’s permeability)
📍reminder in DT- transcellular
✴️Let’s look at Ca transport across various cells✴️
📍PT and the thick ascending limb (TAL) of the loop of Henle - mostly paracellular (depends on transepithelial electrochemical gradient & tight junction’s permeability)
📍reminder in DT- transcellular
✴️Let’s look at Ca transport across various cells✴️
11/ PT: ~ 55-65% of Ca reabsorbed
📌Mostly paracellular- mediated by claudin-2 (CLDN2)
📌Early PT: (dependent on Na)
Na reabsorption (Na-H exchanger (NHE3) & Na-K ATPase)→ osmotic gradient→ H2O absorption→ Ca solute drag
📌late PT: transcellular absorption across Ca gradient
📌Mostly paracellular- mediated by claudin-2 (CLDN2)
📌Early PT: (dependent on Na)
Na reabsorption (Na-H exchanger (NHE3) & Na-K ATPase)→ osmotic gradient→ H2O absorption→ Ca solute drag
📌late PT: transcellular absorption across Ca gradient

12/ Ca reabsorption in PT & Parathyroid hormone (PTH)
📌PTH→⬇️ Calcium reabsorption by attenuating its driving force (Sodium)
📌PTH + PTHR (apical & basolateral)→ activates protein kinases A & C→ inhibits NHE3
📌apical PTHR→ preferential PKC activation→ inhibits Na/ K ATPase
📌PTH→⬇️ Calcium reabsorption by attenuating its driving force (Sodium)
📌PTH + PTHR (apical & basolateral)→ activates protein kinases A & C→ inhibits NHE3
📌apical PTHR→ preferential PKC activation→ inhibits Na/ K ATPase

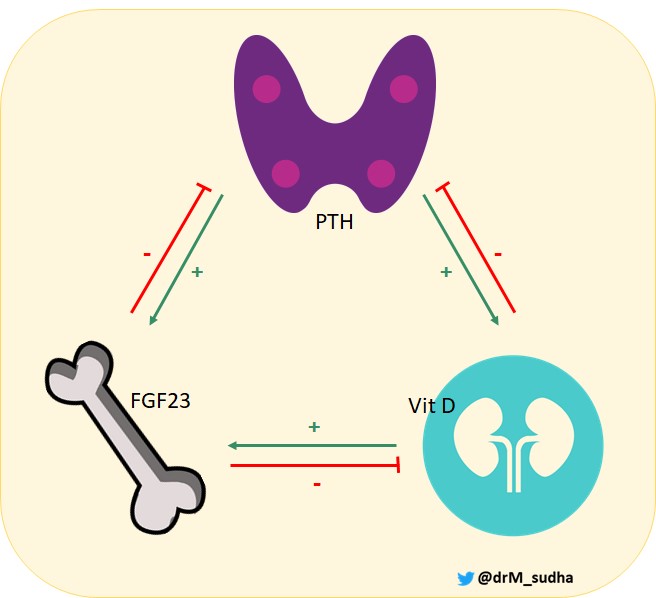
13/ Other actions of PTH →
⬇️ tight-junction permeability in the PT
⬆️active vitamin D3 synthesis
A word about FGF23 - What does FGF23 do to Vit D3 activation?
⬇️ tight-junction permeability in the PT
⬆️active vitamin D3 synthesis
A word about FGF23 - What does FGF23 do to Vit D3 activation?
15/ Let’s look at the mechanisms of Ca absorption at the remaining sites of the nephron
📌TAL & DT: mediated by PTH & vitamin D
📌TAL: ~20% - paracellular- via CLDN 16/19
Other factors that influence Ca handling: EC volume status & acid-base balance
📌TAL & DT: mediated by PTH & vitamin D
📌TAL: ~20% - paracellular- via CLDN 16/19
Other factors that influence Ca handling: EC volume status & acid-base balance

16/ DT: 5-10% of filtered calcium - Transcellular reabsorption
📌PTH (PTHR - basolateral membrane)→ activation of protein kinase A&C pathways → ⬆️ number and activity of TRPV5 (apical) → Ca influx
📌PTH (PTHR - basolateral membrane)→ activation of protein kinase A&C pathways → ⬆️ number and activity of TRPV5 (apical) → Ca influx

17/ In short,3 factors affect Ca reabsorption majorly-
📌PTH : ⬆️TAL & DT (⬇️ PT)
📌Extracellular Volume : Vol Contraction → Na & Ca reabsorption (eg., Thiazide diuretic)
📌Acid-base balance: Acidosis → leaching of Ca from bone🦴 & ⬇️ Ca binding to proteins → calciuria
📌PTH : ⬆️TAL & DT (⬇️ PT)
📌Extracellular Volume : Vol Contraction → Na & Ca reabsorption (eg., Thiazide diuretic)
📌Acid-base balance: Acidosis → leaching of Ca from bone🦴 & ⬇️ Ca binding to proteins → calciuria
18/ Let’s come back to our first question❓
🧂salt-induced calciuria
⬆️ Na intake→⬇️ Na and H2O reabsorption in PT→ osmotic diuresis 🚽→⬇️ Ca reabsorption in PT→Calciuria→Stone 🪨💎💠♦️🔶formation
Also, PO4 reabsorption in the PT is dependent to some degree on Na transport
🧂salt-induced calciuria
⬆️ Na intake→⬇️ Na and H2O reabsorption in PT→ osmotic diuresis 🚽→⬇️ Ca reabsorption in PT→Calciuria→Stone 🪨💎💠♦️🔶formation
Also, PO4 reabsorption in the PT is dependent to some degree on Na transport
19/ So, the Low-Salt Diet prevents stone formation by ⬇️calciuria
👉👉DIET👈👈 is considered THE MOST IMPORTANT factor for management and recurrence
👉👉DIET👈👈 is considered THE MOST IMPORTANT factor for management and recurrence

Until next tweetorial...
#NSMC #Kidneystones #theskeletonKG #nephtwitter #urotwitter @Rupam_Ruchi @amyaimei @kidney_boy @SaynaNorouzi @deniise_am @DTomacruzMD @ASPNeph @sugarkro @DietKidney @KidneyPatients @Thecookingdoc
#NSMC #Kidneystones #theskeletonKG #nephtwitter #urotwitter @Rupam_Ruchi @amyaimei @kidney_boy @SaynaNorouzi @deniise_am @DTomacruzMD @ASPNeph @sugarkro @DietKidney @KidneyPatients @Thecookingdoc
• • •
Missing some Tweet in this thread? You can try to
force a refresh