Welcome to the second installation in our CASE report series! We are sharing challenging, interesting, and teachable cases from our resident teams here at CWRU! Chief Resident @Keithr3890 brings the second case from his time in our Medical ICU #MedEd #Tweetorial #CriticalCare
HPI: A 34 yo F is brought to an outside hospital ED by her husband with 3 days of worsening abdominal pain and new onset confusion. Triage VS: T 35.0, HR 128, BP 50/28, RR 20, SpO2 78% on RA.
The patient is quickly identified as having severe, undifferentiated circulatory shock. Which of the four ‘buckets’ of circulatory shock is most likely in this patient based on pre-test probability?
Teaching Point #1: In a European RCT comparing dopamine and norepinephrine in ~1700 patients presenting to the ICU with circulatory shock, De Backer et al found the following distribution: Distributive ~67%, Cardiogenic ~15%, Hypovolemic ~15% and Obstructive ~3%
At the OSH ED a central line is placed and the patient is given 3L of LR. Labs & blood cultures are drawn and 1g IV vanc & 4.5g IV pip-tazo is given. Norepinephrine infusion is started and patient is accepted for transfer to the MICU at our institution via air ambulance.
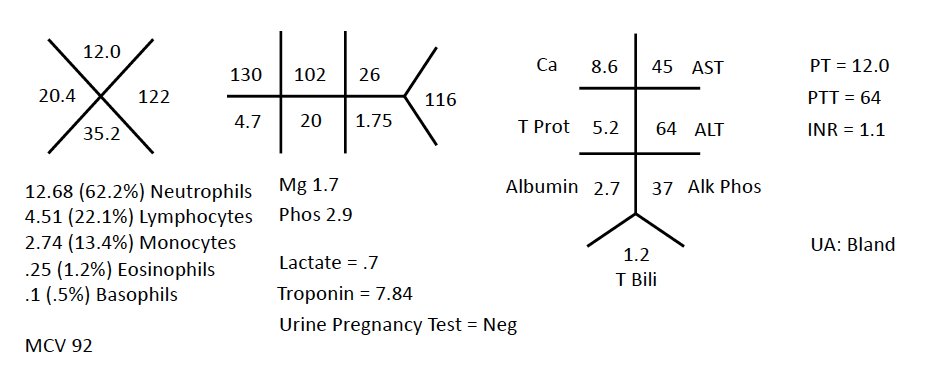
Based on the available data which of the following ‘buckets’ of circulatory shock appear most likely at this time?
Teaching Point #2 – In a study of ICU pts by Abidi et al, eosinopenia (defined as < 40 cells/mm3) had a sens & spec of 80% for the diagnosis of septic shock. Lack of eosinopenia in this pt argues AGAINST septic shock. Eosinopenia has been called a poor man’s procalcitonin!
Just prior to transfer, a non-con CT of the head/chest is performed. No acute intracranial or intrathoracic processes are identified, but patient is noted to have bilateral adrenal gland prominence. 100 mg of IV hydrocortisone is given as pt is loaded into the helicopter...
Teaching Point #3 – The CT raises concern for acute bilateral adrenal hemorrhage. This rare/deadly condition is assoc w/ the following 3 things (among others):
1) Gram Neg Sepsis (Waterhouse-Friedrichsen Synd)
2) Hypercoag. States (HIT and APLS especially)
3) Post-Op pts
The pt arrives to our MICU with VS: T 37.2, HR 104, BP 84/58, RR 20, Spo2 95% on RA. Patient is lethargic, but arousable. Neck is supple. Heart sounds regular & breath sounds vesicular. The abdomen is diffusely TTP w/out rebound or guarding. No rashes or lesions are visible.
What would your next step in management be?
A lumbar puncture and CT abd/pelvis are performed. Lumbar puncture is unremarkable. CT abd/pelvis is consistent with bilateral adrenal grand hemorrhage & infarction. Additional history is obtained from the patient’s husband…
Husband reveals the patient was recently diagnosed w/ ITP and started on a med called Eltrombopag – a thrombopoietin analog. This medication has been associated w/ bilateral adrenal hemorrhage & infarction in pts with underlying, undiagnosed anti-phospholipid syndrome (APS)!
Serologic studies later confirm the diagnosis of APS. The patient’s condition improved rapidly with continued glucocorticoids.
Teaching Point #4 - Remember that APS causes isolated prolongation of the PTT despite being a hypercoagulable state (see labs on tweet 6 of 18).
Teaching Point #5
The anatomy of the adrenals actually make them vulnerable to hemorrhage! 3 arteries supply, while only 1 vein drains. Kovacs et al describe this as a ‘vascular dam’. We also know that catecholamines are pro-thrombotic and cause vasoconstriction...
During times of stress, the adrenal veins have the highest concentration of catecholamines in the entire body. A thrombus forming in the adrenal vein is thus a predictable, but catastrophic event given its blood supply. It is a wonder it doesn’t happen more often…
Hope you enjoyed our case! Please let us know what you think. We will be looking to share more CASE reports throughout the year.
De backer et al - DOI: 10.1056/NEJMoa0907118
Abidi et al - DOI: 10.1186/cc6883
Kovacs et al - DOI: 10.1097/00005792-200101000-00005