1/
Have you ever a junior member of your team ask you a question, and you had NO IDEA what the answer was?
Like, literally no clue.
Racking your brain.
Nothing.
Nope, just me?
This week’s #MedEdTwagTeam #ClinicalTeaching topic: Humility.
#MedTwitter #MedEd
Have you ever a junior member of your team ask you a question, and you had NO IDEA what the answer was?
Like, literally no clue.
Racking your brain.
Nothing.
Nope, just me?
This week’s #MedEdTwagTeam #ClinicalTeaching topic: Humility.
#MedTwitter #MedEd
2/
On my first day as a senior resident, I was terrified that my interns would ask me a question that I didn’t know.
…And they did.
So I said, “I don’t know, let’s look it up.”
And, (not surprisingly) they appreciated that.
Me, admitting my limitations & offering to help.
On my first day as a senior resident, I was terrified that my interns would ask me a question that I didn’t know.
…And they did.
So I said, “I don’t know, let’s look it up.”
And, (not surprisingly) they appreciated that.
Me, admitting my limitations & offering to help.
3/ Honestly, this fear of not knowing things still plagues me.
I have a weird combination of confidence + imposter syndrome.
Some days I feel confident.
Other days I wonder why everyone else is so much smarter than me.
Why can't I remember the names of those famous trials?!
I have a weird combination of confidence + imposter syndrome.
Some days I feel confident.
Other days I wonder why everyone else is so much smarter than me.
Why can't I remember the names of those famous trials?!
4/
During residency I watched brilliant attendings solve mystery cases with ease.
I felt that I would never get there.
But then I realized that the “all knowing” physician was a myth.
We are all constantly learning & growing.
During residency I watched brilliant attendings solve mystery cases with ease.
I felt that I would never get there.
But then I realized that the “all knowing” physician was a myth.
We are all constantly learning & growing.
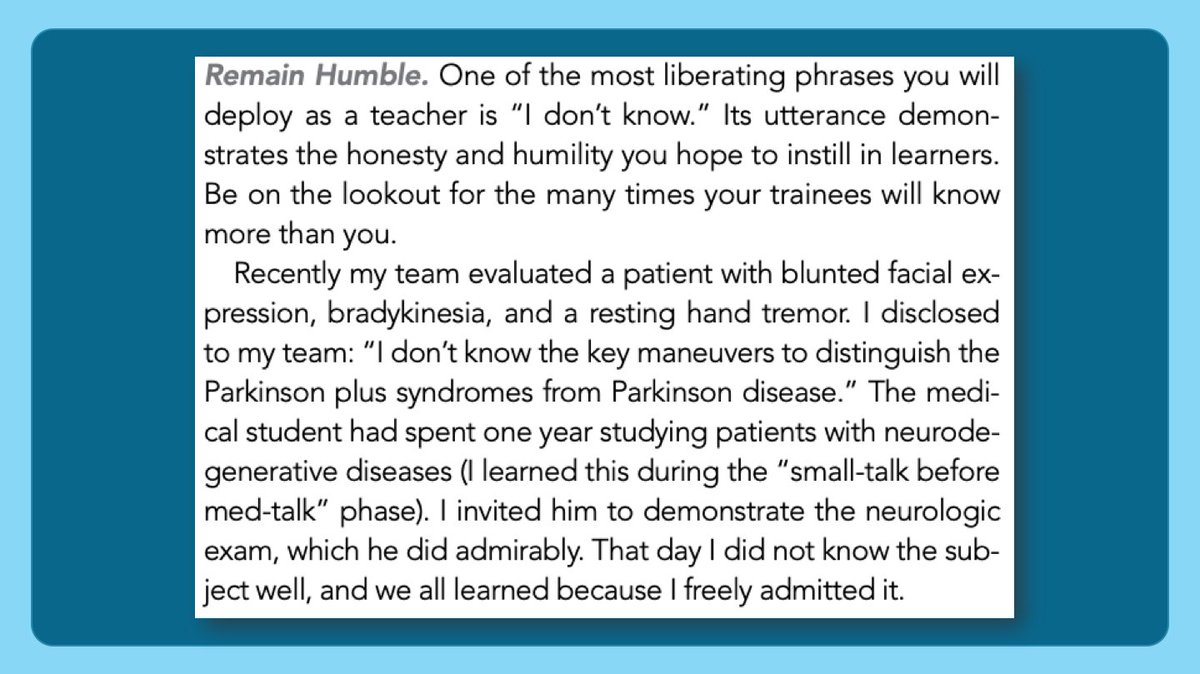
5/ And reading this passage from @DxRxEdu @Gurpreet2015 in @JHospMedicine tells me that I’m not alone.
“I don’t know.”
What a powerful phrase.
(Here’s the link to the full article: journalofhospitalmedicine.com/jhospmed/artic…)
“I don’t know.”
What a powerful phrase.
(Here’s the link to the full article: journalofhospitalmedicine.com/jhospmed/artic…)
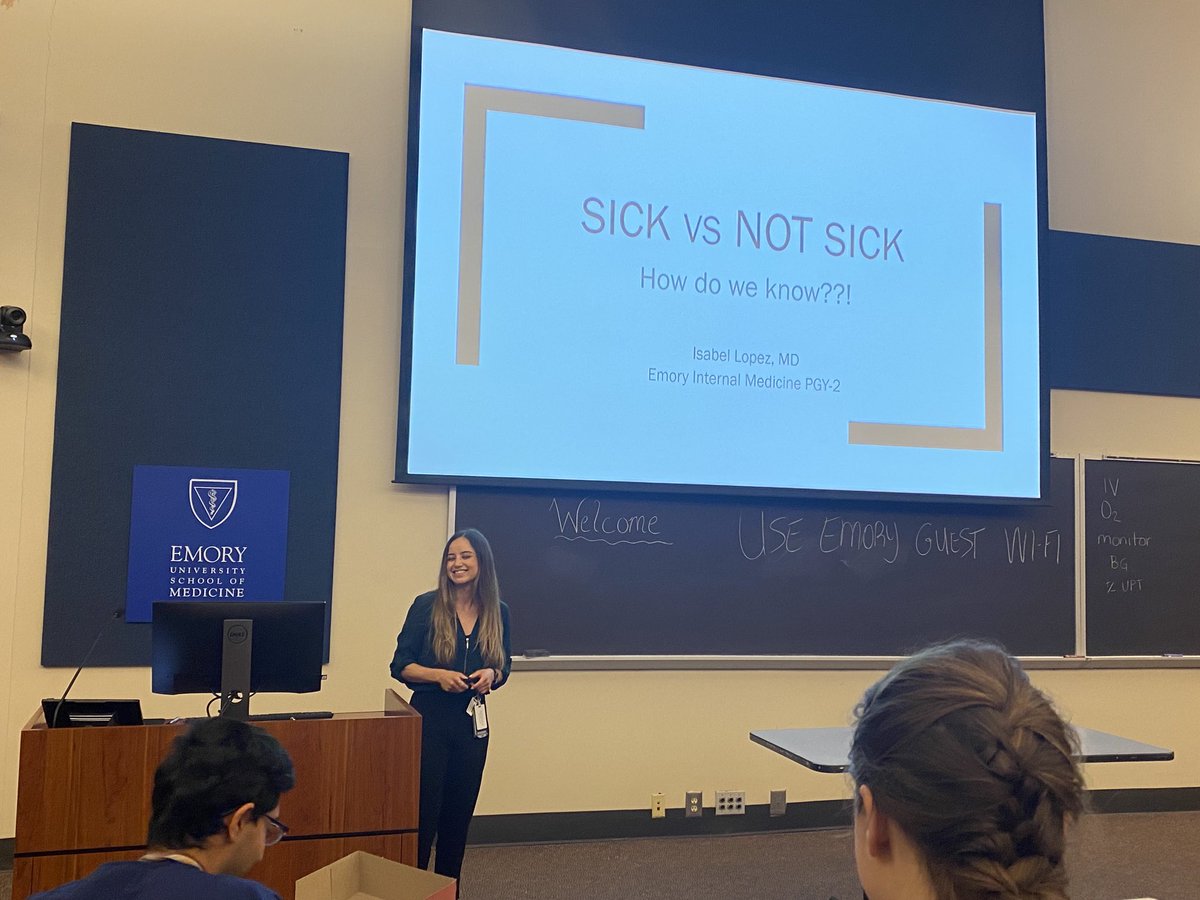
6/ And, over the last few months, @ricapitt & I have had Resident as Teacher sessions with our new(ish) @emoryimchiefs PGY2 residents.
When we ask them what their biggest fear is about being a senior resident, it’s a familiar concern:
That they won’t know enough.
When we ask them what their biggest fear is about being a senior resident, it’s a familiar concern:
That they won’t know enough.
7/ But, funny enough, when I hear them say this, I know they are going to be just fine.
Because they are humble.
They recognize their limits.
And they are sharing their fears.
Because they are humble.
They recognize their limits.
And they are sharing their fears.
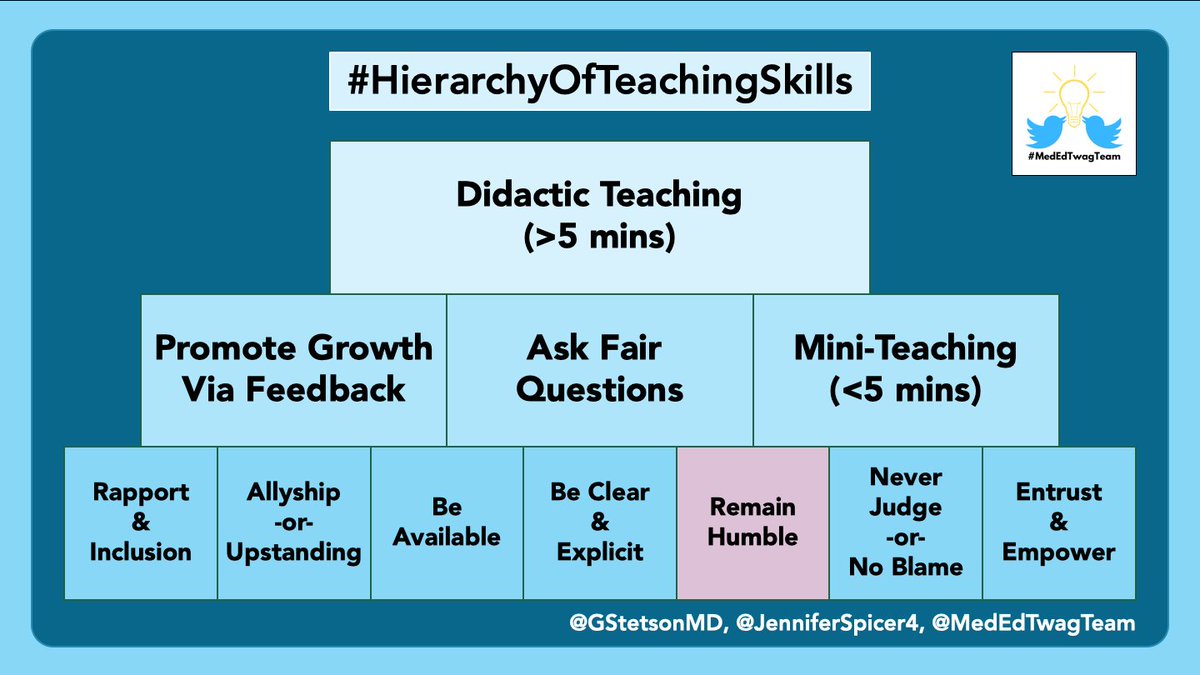
8/ Which all comes back to today’s concept of remaining humble.
Humility has helped me in 3 important ways on my clinical teams:
1⃣Flattening the hierarchy.
2⃣Establishing a growth mindset.
3⃣Creating trust.
Humility has helped me in 3 important ways on my clinical teams:
1⃣Flattening the hierarchy.
2⃣Establishing a growth mindset.
3⃣Creating trust.
9/ First, flattening the hierarchy.
On the first day of wards, I make it clear that everyone on the team has unique knowledge & value.
There is a LOT that I don’t know.
I’m very up-front about that.
I tell the team to correct me (and they do).
On the first day of wards, I make it clear that everyone on the team has unique knowledge & value.
There is a LOT that I don’t know.
I’m very up-front about that.
I tell the team to correct me (and they do).
10/ I emphasize teamwork.
And I encourage everyone to speak up if they have an idea, even if it’s not “their” patient.
I make it clear that a “correction” from someone else doesn’t reflect poorly on the person who was corrected.
We are all a team, and everyone gets the credit.
And I encourage everyone to speak up if they have an idea, even if it’s not “their” patient.
I make it clear that a “correction” from someone else doesn’t reflect poorly on the person who was corrected.
We are all a team, and everyone gets the credit.
11/ If you haven’t read Atul Gawande’s book “The Checklist Manifesto,” I highly recommend it.
atulgawande.com/book/the-check…
And this article from @MedEd_Journal is also a great read: onlinelibrary.wiley.com/doi/abs/10.111…
atulgawande.com/book/the-check…
And this article from @MedEd_Journal is also a great read: onlinelibrary.wiley.com/doi/abs/10.111…
12/ Second, establishing a growth mindset.
If you aren’t familiar with the term growth mindset, here’s a link to a 2 page summary from @MedEd_Journal:
onlinelibrary.wiley.com/doi/abs/10.111…
Growth mindset = success is due to effort
Fixed mindset = success driven by innate ability
If you aren’t familiar with the term growth mindset, here’s a link to a 2 page summary from @MedEd_Journal:
onlinelibrary.wiley.com/doi/abs/10.111…
Growth mindset = success is due to effort
Fixed mindset = success driven by innate ability
13/
Part of a growth mindset is recognizing that we all can improve.
So, in the spirit of a growth mindset, I remind my team that we are all (myself included) there to learn.
I HOPE they have gaps in their knowledge; otherwise, what am I doing there?!
Part of a growth mindset is recognizing that we all can improve.
So, in the spirit of a growth mindset, I remind my team that we are all (myself included) there to learn.
I HOPE they have gaps in their knowledge; otherwise, what am I doing there?!
14/ Third, humility engenders trust.
When trainees come to me and admit that they don’t know something (i.e. humility), it helps me trust that they know the boundaries of their knowledge.
I know that I can trust what they say and do.
And vice versa.
When trainees come to me and admit that they don’t know something (i.e. humility), it helps me trust that they know the boundaries of their knowledge.
I know that I can trust what they say and do.
And vice versa.
15/ So, in summary, consider how you can role model your humility by:
Admitting “I don’t know”
This will help your team by:
1⃣Flattening the hierarchy
2⃣Encouraging a growth mindset
3⃣Creating trust
Admitting “I don’t know”
This will help your team by:
1⃣Flattening the hierarchy
2⃣Encouraging a growth mindset
3⃣Creating trust
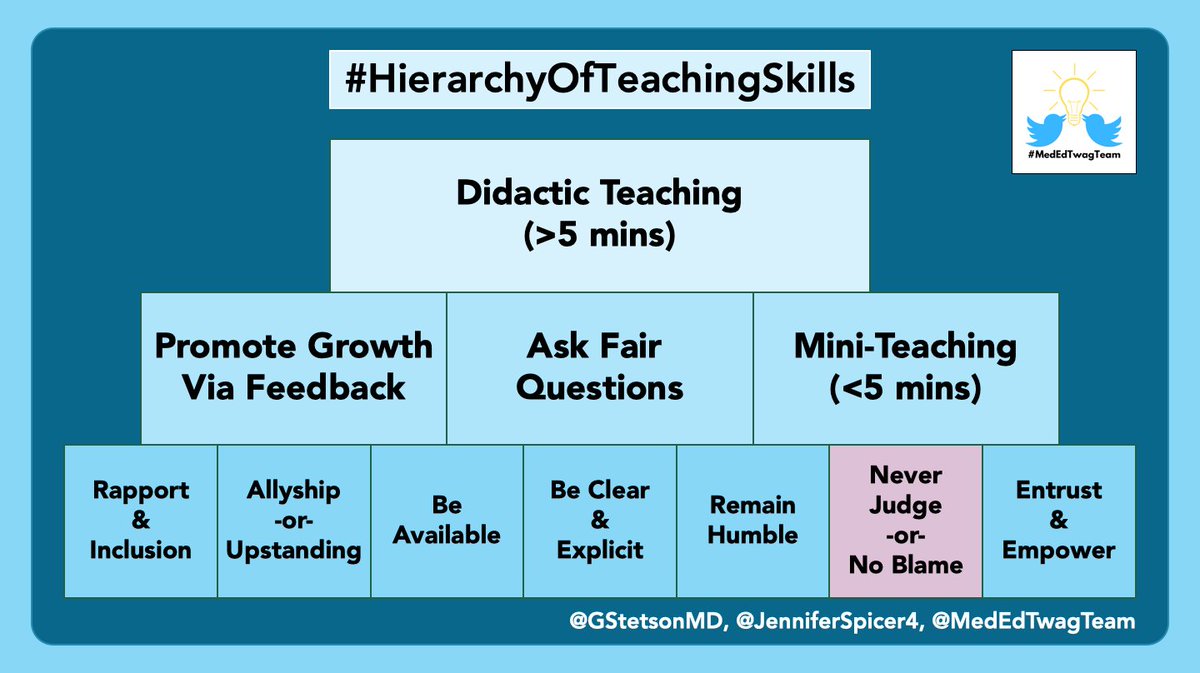
16/ And keep an eye out for @GStetsonMD’s thread next Tuesday on ”Never Judge”
And check out the @MedEdTwagTeam if you want to see all of our threads in one place!
Thanks for joining, and we will see you next week!
And check out the @MedEdTwagTeam if you want to see all of our threads in one place!
Thanks for joining, and we will see you next week!
• • •
Missing some Tweet in this thread? You can try to
force a refresh