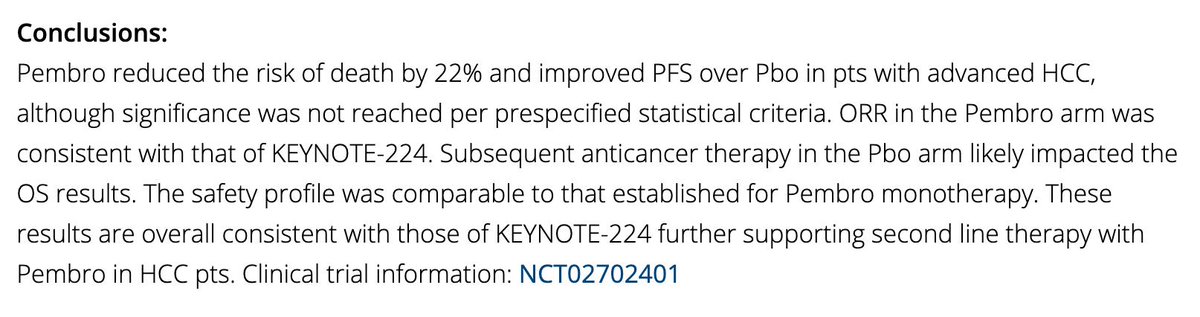
How did hematopoietic stem cell transplantation (BMT) develop? A procedure that is so widely used now and have led to the cure of many hematologic disorders has evolved over the last 70 years. This 🧵 is a short historical overview of #BMT 

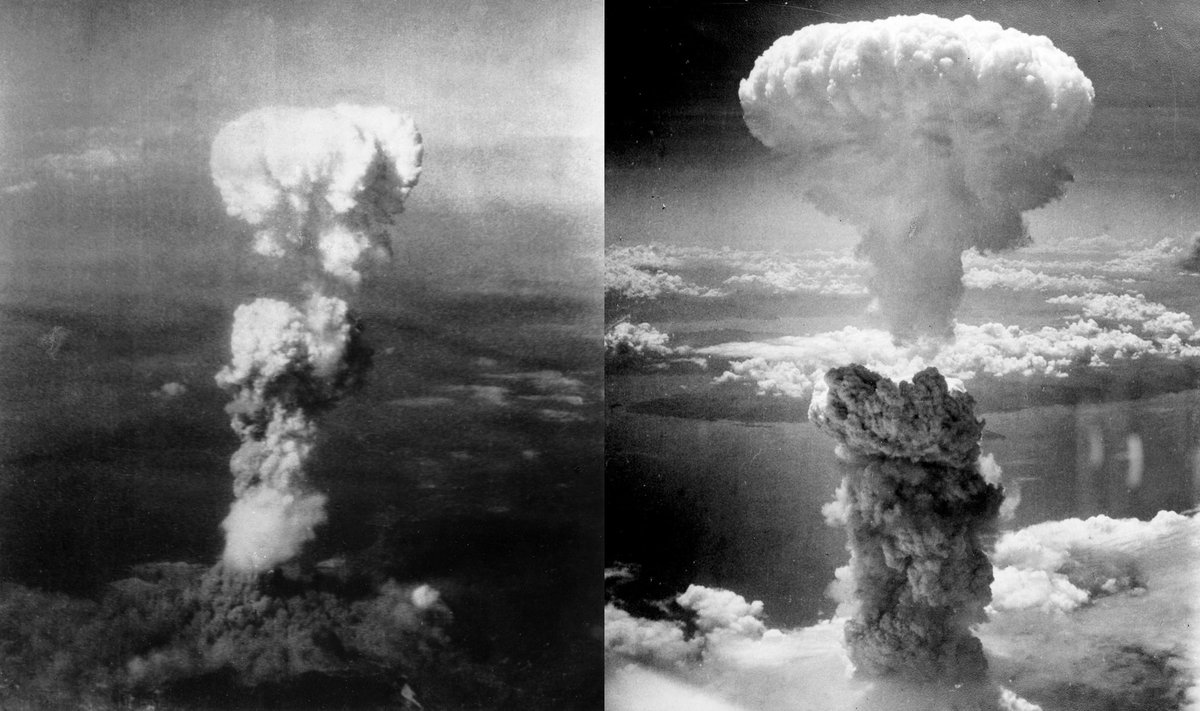
After Word War II, and specifically after the atomic bomb was dropped on Hiroshima and Nagasaki in 1945, there was an interest in funding treatments for radiation sickness that caused bone marrow failure and led to the death of many. 
In 1949, L.O. Jacobsen demonstrated that mice can be protected from otherwise lethal effects of body irradiation by shielding the spleen (the spleen in mice contains hematopoietic tissue) 
In 1951, Lorenz et al showed that this protection can also be achieved by infusing fresh bone marrow intravenously after lethal doses of radiation.
This recovery was thought to be due to “humoral” factors in the syngeneic (genetically identical) bone marrow.
This recovery was thought to be due to “humoral” factors in the syngeneic (genetically identical) bone marrow.
In a 1956 a @nature paper demonstrated that the injection of bone marrow from one animal replaced the cellular characteristics of the host.
The recipient was termed a “radiation chimera” - a Greek mythological creature with a lion’s head, a goat’s body, and a serpent’s tail.

The recipient was termed a “radiation chimera” - a Greek mythological creature with a lion’s head, a goat’s body, and a serpent’s tail.


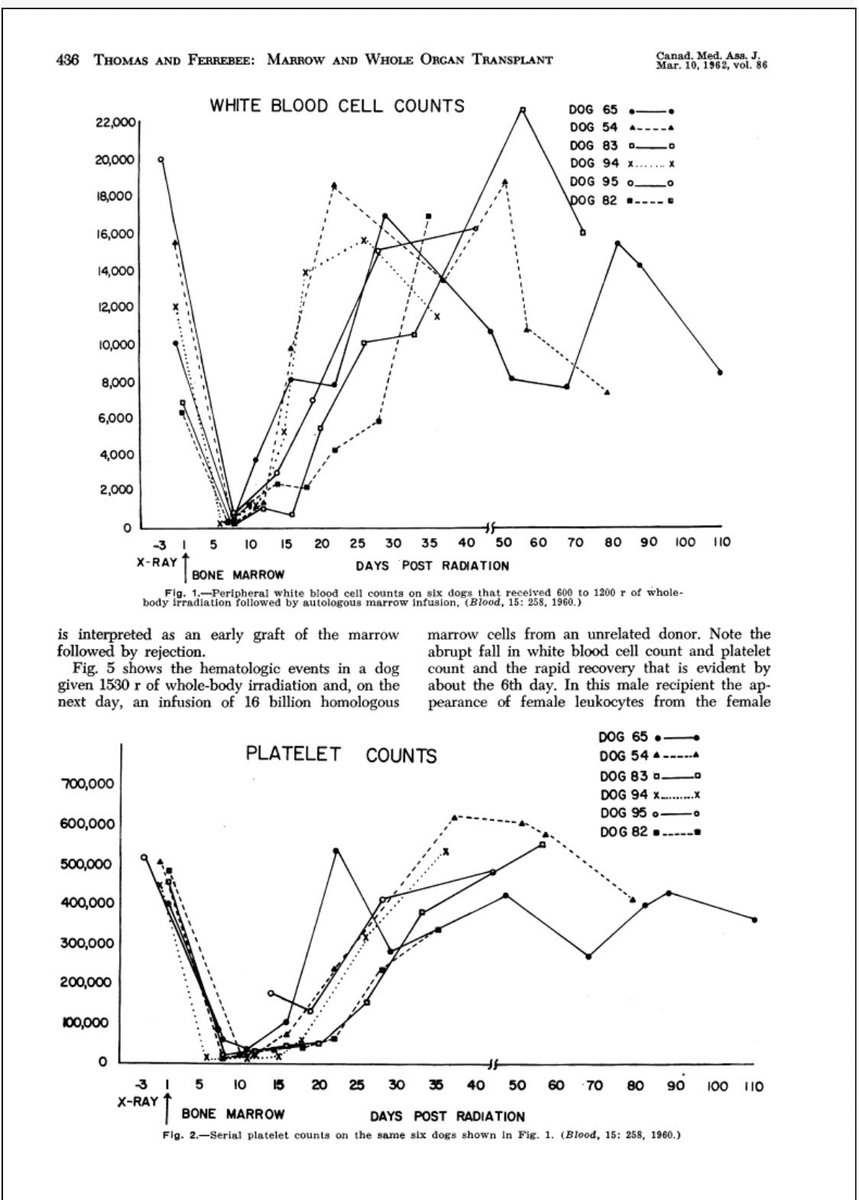
In the late 1950s, E. Donnall Thomas and colleagues in New York worked on canine models to determine the dose of total body irradiation (TBI) needed to prevent graft rejection.
On the right is the WBC and platelet counts of a group of dogs given between 600-1200 r (6-12 Gy)

On the right is the WBC and platelet counts of a group of dogs given between 600-1200 r (6-12 Gy)
Before gaining a full understanding of all the key factors, #BMT was tested in humans.
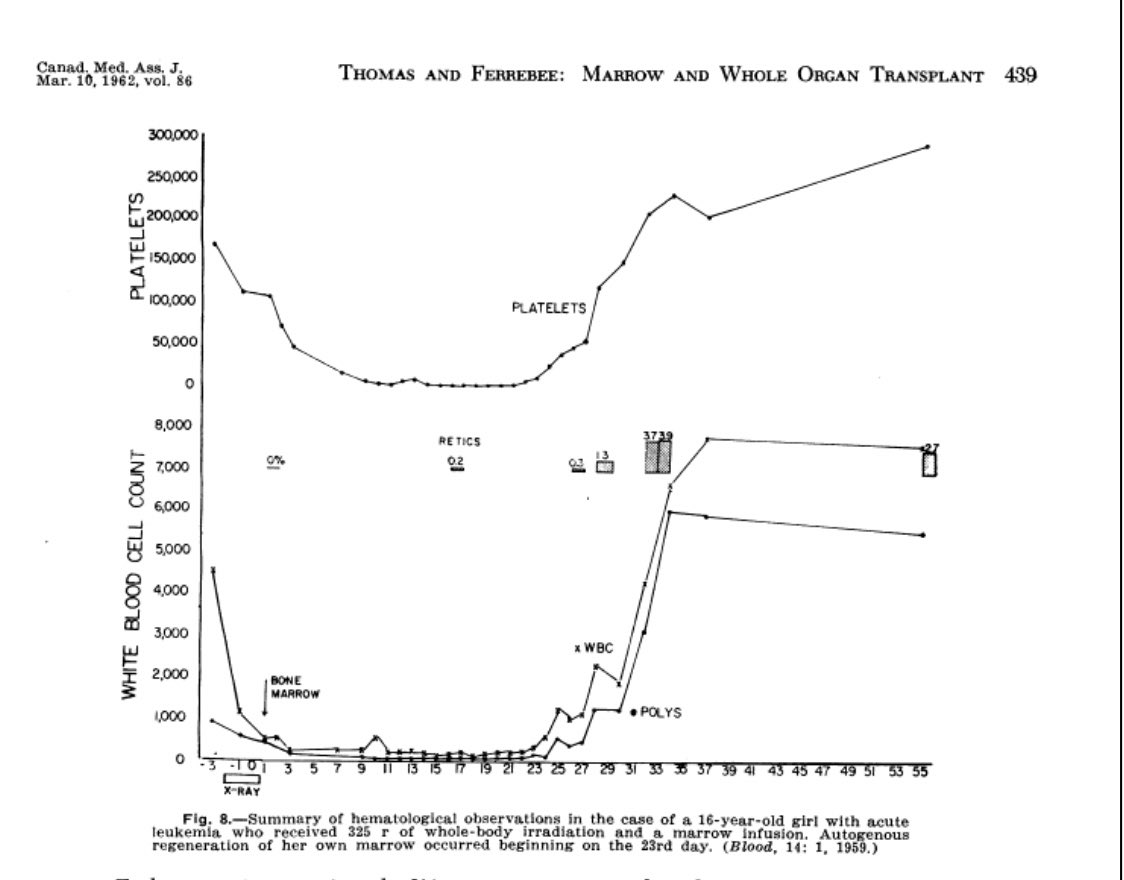
Thomas describes in his 1962 paper a 16-year old patient with terminal AML who received 325 r of TBI, marrow infusion from her sister, had a remission but with autologous recovery.
Thomas describes in his 1962 paper a 16-year old patient with terminal AML who received 325 r of TBI, marrow infusion from her sister, had a remission but with autologous recovery.
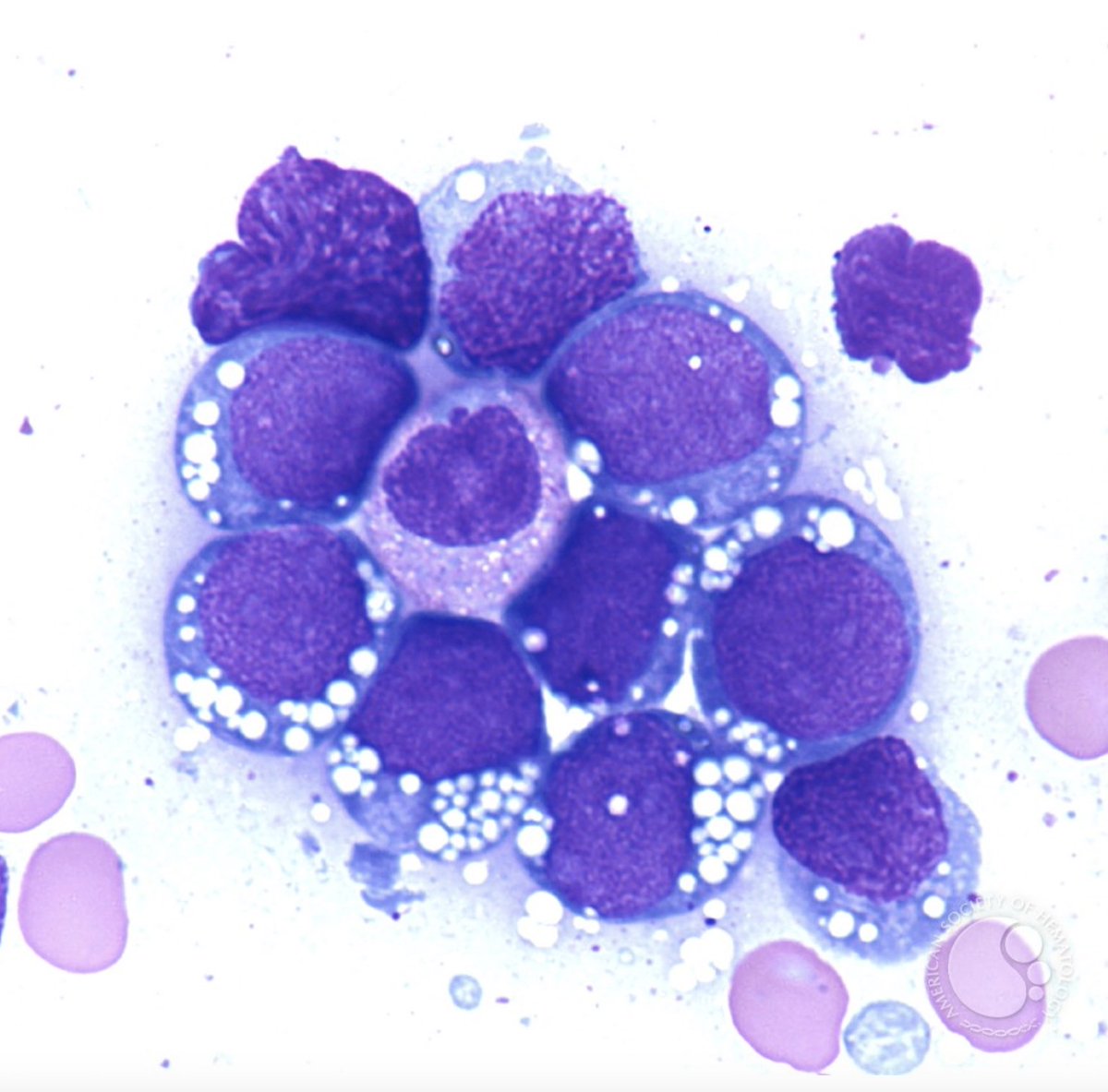
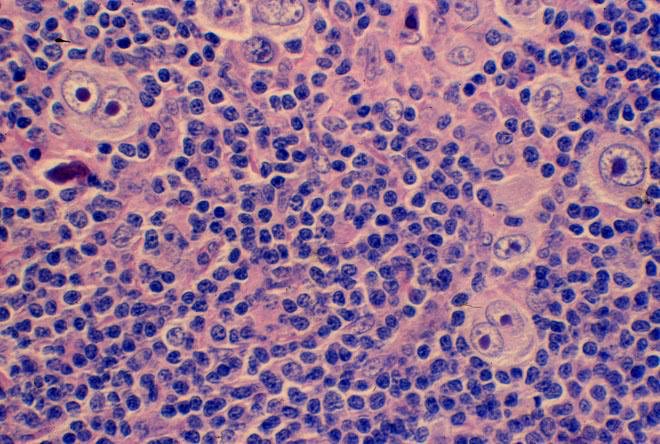
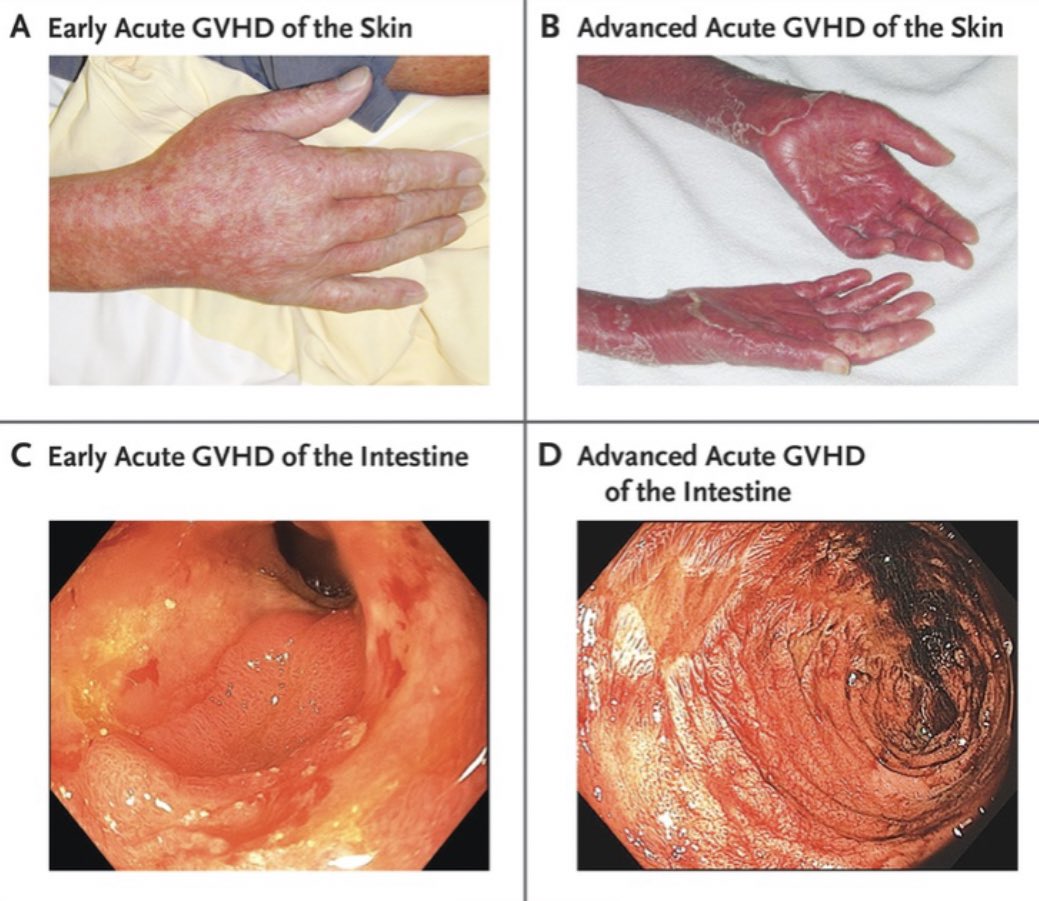
During animal studies, many mice and dogs developed a wasting, rash and diarrhea syndrome that was termed “secondary disease”
This was the first indicator of what would later be called graft versus host disease (GVHD)
This was the first indicator of what would later be called graft versus host disease (GVHD)
More human studies were carried out around the same time as scientists were trying to gain a better understanding of #BMT in the lab.
The same obstacles existed in successfully transplanting humans:
1) Graft failure
2) GVHD
The same obstacles existed in successfully transplanting humans:
1) Graft failure
2) GVHD
In 1958, French oncologist, Georges Mathé performed #BMT on 6 Yugoslav engineers that were exposed to radiation during a nuclear reactor incident. None survived.
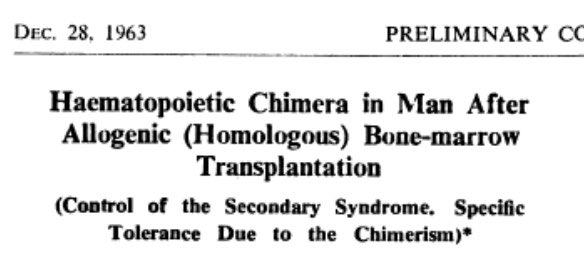
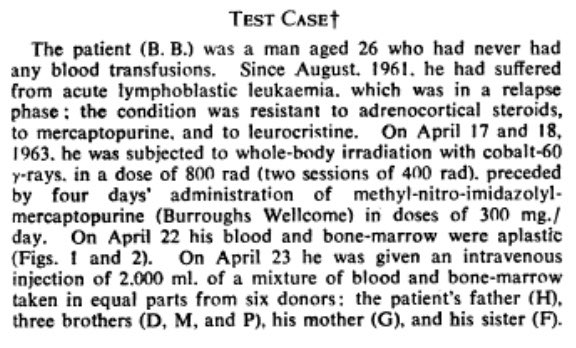
In 1963, he was able to carry out the first allogeneic #BMT, using 6 donors for 1 recipient showing donor chimerism.


In 1963, he was able to carry out the first allogeneic #BMT, using 6 donors for 1 recipient showing donor chimerism.
In 1959, Thomas performed the first syngeneic (from an identical twin) #BMT for refractory leukemia. The disease recurred.
Robert Kyle, who had trained under Thomas, successfully performed a syngeneic #BMT in 1963 for aplastic anemia - Nancy and her twin sister 👇 with Kyle
Robert Kyle, who had trained under Thomas, successfully performed a syngeneic #BMT in 1963 for aplastic anemia - Nancy and her twin sister 👇 with Kyle

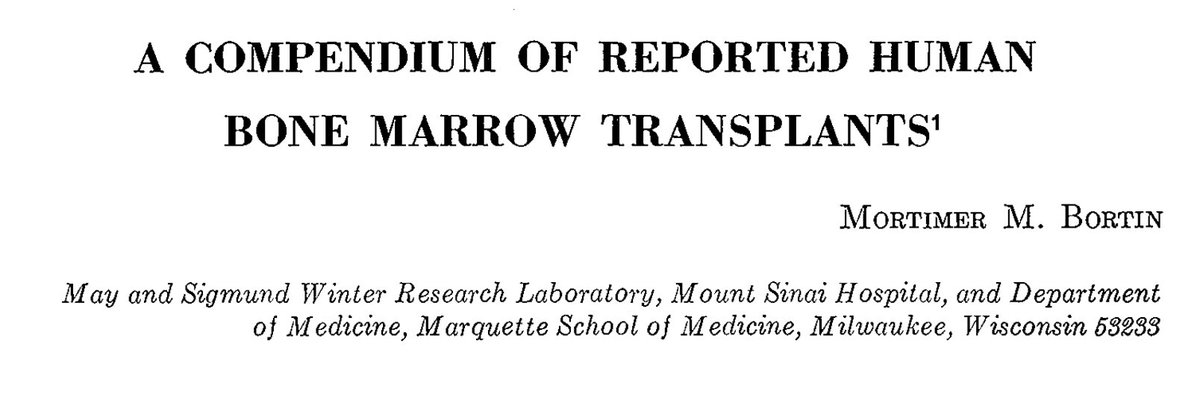
Despite these anecdotes, between 1956-1967, >200 allogeneic BMT were performed. M. Bortin published their outcomes in 1970 - not one of them had been successful!
The was less enthusiasm about #BMT as shown by the decrease in procedures
But, advances were on the horizon..


The was less enthusiasm about #BMT as shown by the decrease in procedures
But, advances were on the horizon..
In 1958, French immunologist, Jean Dausset identified human leukocyte antigens (HLA) which led to the formation of anti-leukocyte antibodies in recipients of blood transfusions.
Further understanding of histocompatibility was essential for the success of the marrow graft.
Further understanding of histocompatibility was essential for the success of the marrow graft.
Delta Uphoff et al showed that immunosuppression with methotrexate (MTX) ameliorated the effects of GVHD in mice.
Various MTX regimens were then tried in canines and then humans.
Various MTX regimens were then tried in canines and then humans.
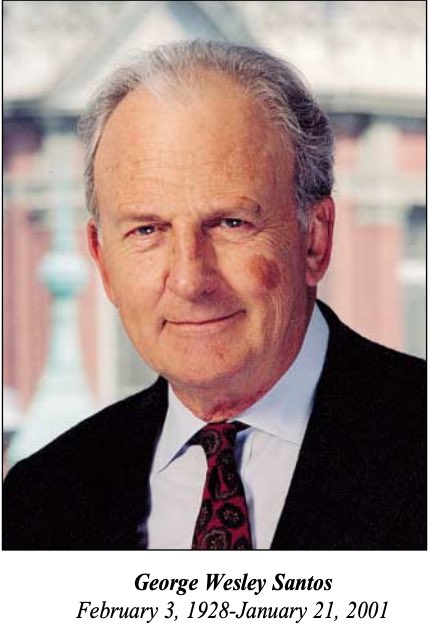
In 1965, cyclophosphamide was shown to be a potent immunosuppressant in a mouse model by George Santos, et al.
Rainer Storb used cyclophosphamide in place of TBI in dogs - he would later go on to develop the MTX/cyclosporine regimen for prevention of GVHD

Rainer Storb used cyclophosphamide in place of TBI in dogs - he would later go on to develop the MTX/cyclosporine regimen for prevention of GVHD

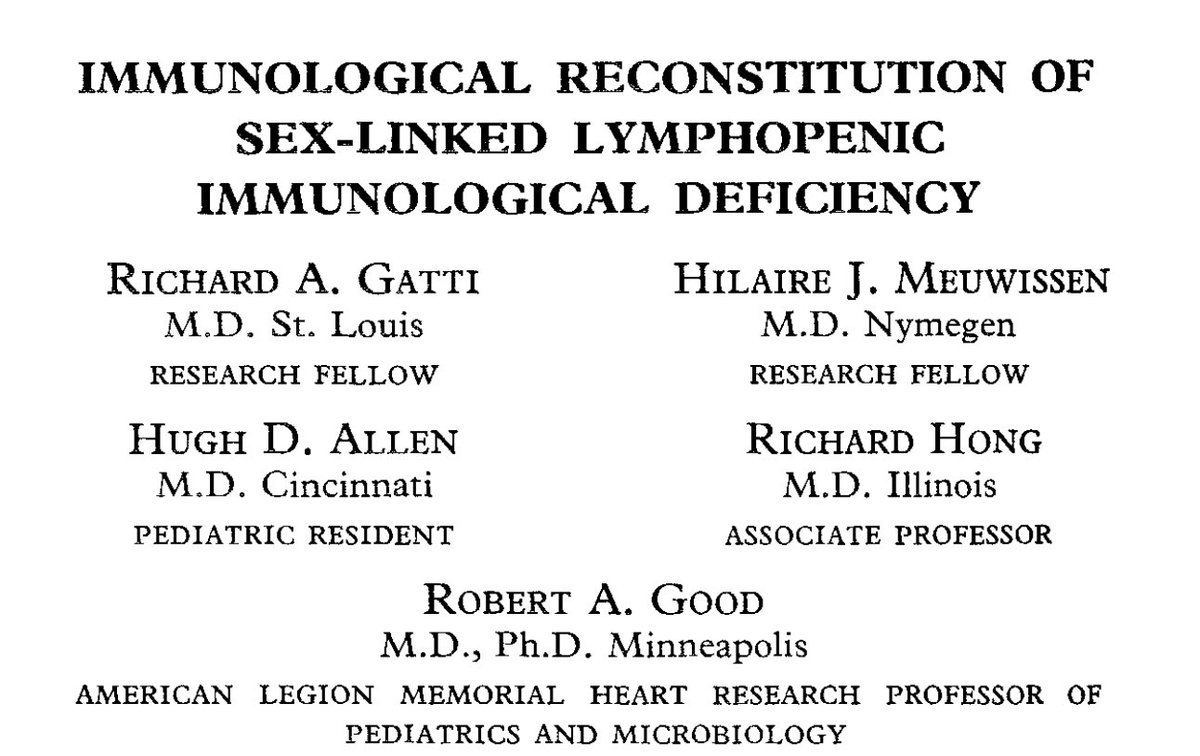
In 1968, the first 2 successful allogeneic-HCTs in non-malignant diseases were described in @TheLancet.
R. Good et al transplanted an HLA-matched marrow from a sibling to cure an 5-month old boy with severe combined immunodeficiency

R. Good et al transplanted an HLA-matched marrow from a sibling to cure an 5-month old boy with severe combined immunodeficiency

F. Bach and M. Bortin et al transplanted an HLA-matched sibling marrow to cure a 2 year old boy with Wiskott-Aldrich syndrome after preparation with cyclophosphamide 


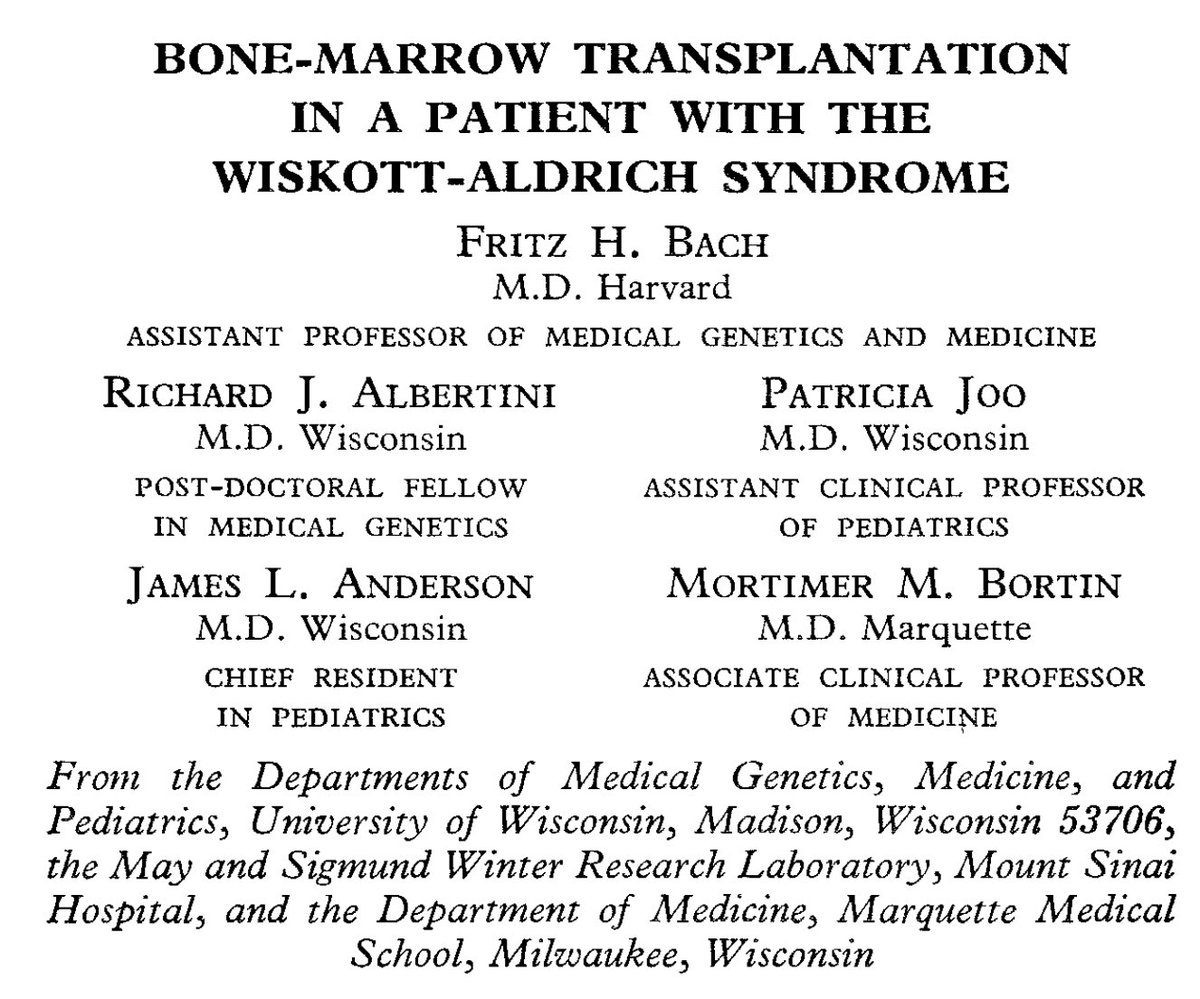
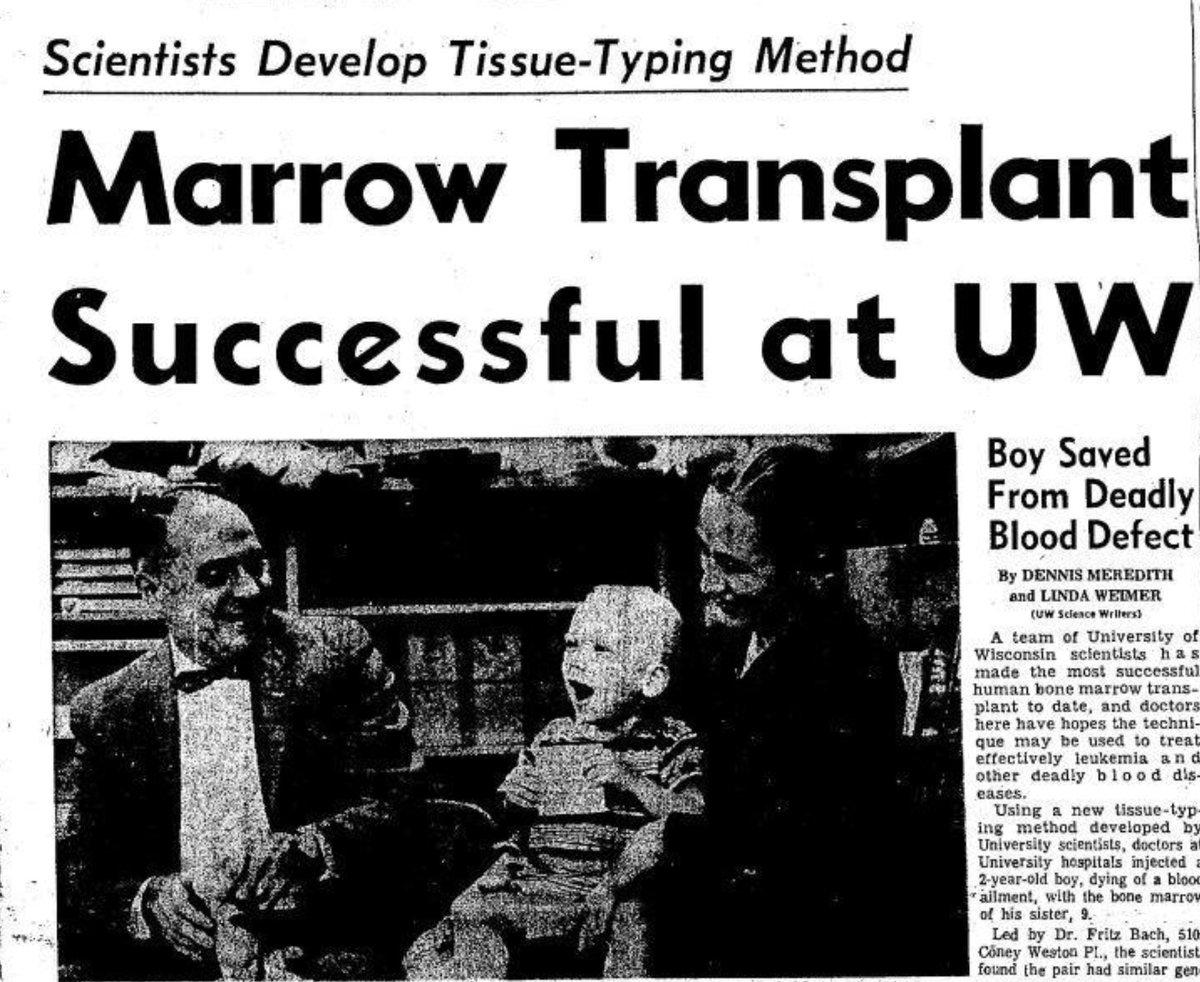

Bortin would go on to co-find the International Bone Marrow Transplant Registry (IBMTR) in 1970 at the Medical College of Wisconsin
@CIBMTR was created when the @NationalMarrow program united with IBMTR.
@CIBMTR was created when the @NationalMarrow program united with IBMTR.
By 1977, @fredhutch published a report of their first 100 allogeneic-#BMT recipients with the advanced acute leukemia treated with Cy/TBI and received marrow from HLA-matched sibling.
17% were alive at 1 year, and 8% lived >20 years. This was the first signal of cure with #BMT
17% were alive at 1 year, and 8% lived >20 years. This was the first signal of cure with #BMT
In 1979 the Seattle group reported outcomes of 19 patients who underwent allo-HCT with Cy/TBI prep followed by MTX for immunosuppression
50% would go on to survive >20 years
50% would go on to survive >20 years

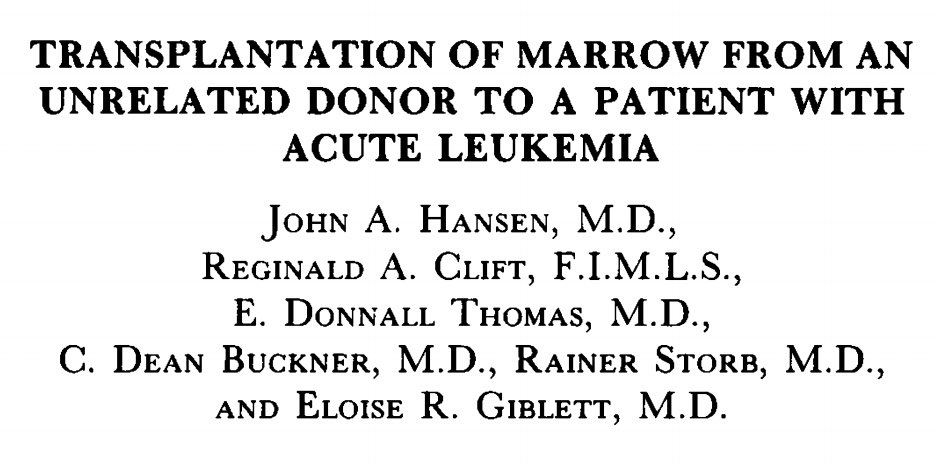
Eloise “Elo” Giblett was instrumental in pioneering unrelated marrow transplantation, publishing the first case report in @NEJM in 1980.
Her work in immunology and blood banking led to the discovery of the first immunodeficiency, and identification of many blood group antigens.

Her work in immunology and blood banking led to the discovery of the first immunodeficiency, and identification of many blood group antigens.

In 1980, Dausset was awarded the Nobel Prize in Physiology (along with Benacerraf and Davies) for their work in characterizing the major histocompatibility complex.
In 1990, E. Donnall Thomas was awarded the Nobel Prize for the development of cell and organ transplantation.

In 1990, E. Donnall Thomas was awarded the Nobel Prize for the development of cell and organ transplantation.
For the past 40 years, researchers have been able to gain a better understanding of many of the key factors that result in a successful and safe allo-HCT
1) Characterizing HLA alleles
2) Optimizing conditioning regimens
3) Improving supportive care
4) Treating GVHD
1) Characterizing HLA alleles
2) Optimizing conditioning regimens
3) Improving supportive care
4) Treating GVHD
Marrow grafting has evolved from a highly experimental procedure to being accepted as standard treatment modality. Progress has been slow but positive. There is more work to be done to advance the field further.
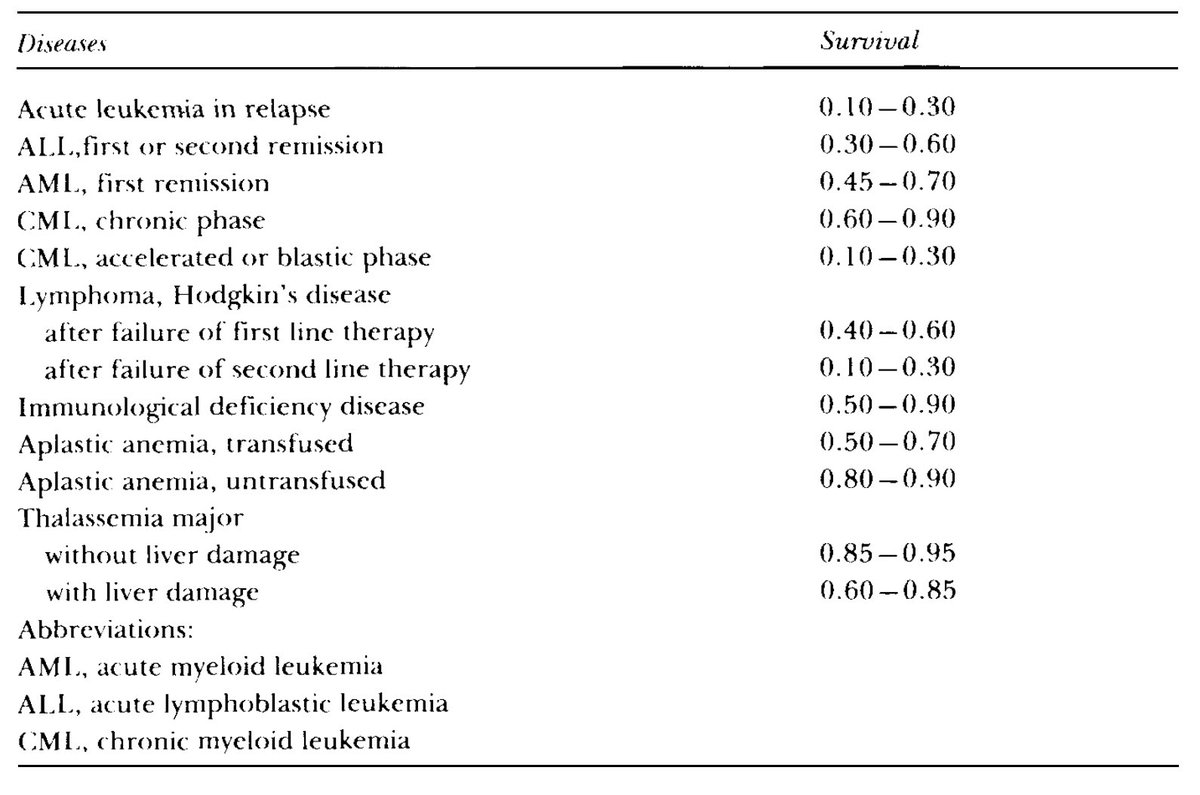
In 1990, Thomas presented the 5-year DFS during his Nobel lecture
In 1990, Thomas presented the 5-year DFS during his Nobel lecture
Mathé, Thomas, Dausett, Bortin, and Giblett were a few instrumental investigators; many were not mentioned.
With better treatments, one can only hope that #BMT will someday become obsolete, and these stories will remain in the archives of history to be reflected upon and studied
With better treatments, one can only hope that #BMT will someday become obsolete, and these stories will remain in the archives of history to be reflected upon and studied
• • •
Missing some Tweet in this thread? You can try to
force a refresh