1/ Understanding CDC’s updated guidance that aerosols are the main mode of SARS-CoV-2 transmission
CDC recently updated its guidance. It is worded in a confusing way & this makes it a little self-contradictory. This is causing some confusion, so I’ll try to explain it here
CDC recently updated its guidance. It is worded in a confusing way & this makes it a little self-contradictory. This is causing some confusion, so I’ll try to explain it here
2/ Bottom line 1 : most important new text is:
“These particles can be inhaled into the nose, mouth, airways, and lungs and cause infection. This is thought to be the main way the virus spreads.”
Particles here (and this thread) = either aerosols or droplets (NOT virions)
“These particles can be inhaled into the nose, mouth, airways, and lungs and cause infection. This is thought to be the main way the virus spreads.”
Particles here (and this thread) = either aerosols or droplets (NOT virions)
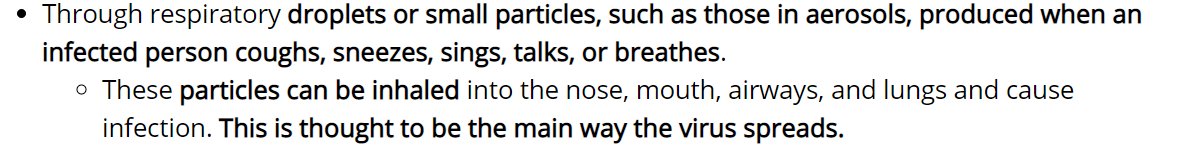
3/ **Inhalation = aerosols**, period, full stop.
We’ll review the history later.
They also use the word "droplet," but not consistently with current or historical WHO/CDC definitions, we'll get to that soon
We’ll review the history later.
They also use the word "droplet," but not consistently with current or historical WHO/CDC definitions, we'll get to that soon
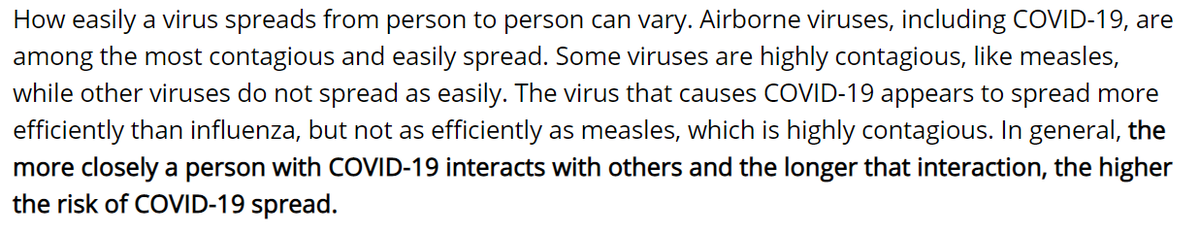
4/ Bottom line 2: Also very important text:
“Airborne viruses, including COVID-19, are among the most contagious and easily spread. Some viruses are highly contagious, like measles, while other viruses do not spread as easily.
“Airborne viruses, including COVID-19, are among the most contagious and easily spread. Some viruses are highly contagious, like measles, while other viruses do not spread as easily.

5/ The virus that causes COVID-19 appears to spread more efficiently than influenza, but not as efficiently as measles, which is highly contagious.”
(yours truly has been stating the idea in last sentence for months, e.g. medscape.com/viewarticle/93…)
(yours truly has been stating the idea in last sentence for months, e.g. medscape.com/viewarticle/93…)
6/ So **Inhalation is thought to be the main way the virus spreads.**
What particles can be inhaled?
Inhalation is the flow of air into our respiratory system due to breathing (en.wikipedia.org/wiki/Inhalation)
What particles can be inhaled?
Inhalation is the flow of air into our respiratory system due to breathing (en.wikipedia.org/wiki/Inhalation)
7/ EPA gives us the summary of a lot of research on deposition of inhaled particles in the respiratory tract at epa.gov/pmcourse/parti…
So basically particles up to ~100 um can be inhaled. Larger particles cannot.
So basically particles up to ~100 um can be inhaled. Larger particles cannot.

8/ Droplets are defined as particles that fall in 1-2 m & infect by impact on eyes, nostrils, or mouth
Let’s review the history of "droplet" for disease transmission (we are very close to submitting a paper on this history, so it is fresh in my mind):
Let’s review the history of "droplet" for disease transmission (we are very close to submitting a paper on this history, so it is fresh in my mind):
https://twitter.com/linseymarr/status/1278036517890347008
9/ “Droplets” in disease transmission arose from the work of Carl Fuggle in 1890s. Using collection on agar plates, he showed that bacteria expelled from the mouth were observed close but not far from the subjects.
zenodo.org/record/1686460…
zenodo.org/record/1686460…
10/ Charles Chapin, President of the American Public Health Association, wrote a seminar book in 1910.
Correctly concluded that close proximity led to respiratory infection, and that social distance worked to reduce it.
That’s where social distance comes from, and it works
Correctly concluded that close proximity led to respiratory infection, and that social distance worked to reduce it.
That’s where social distance comes from, and it works
11/ But why does social distance work?
Unfortunately, he incorrectly attributed this observation to “sprayborne” transmission, due to Flugge’s droplets. And the said that “airbone” transmission was nearly impossible. A fateful error.
Chapin's book: archive.org/details/source…
Unfortunately, he incorrectly attributed this observation to “sprayborne” transmission, due to Flugge’s droplets. And the said that “airbone” transmission was nearly impossible. A fateful error.
Chapin's book: archive.org/details/source…
12/ Chapin: “former ideas [that] diseases may be air-borne are entirely erroneous; that most diseases are [...] spray-borne only for two or three feet, a phenomenon which after all resembles contact infection more than it does aerial infection as ordinarily understood.” 

13/ Let’s take that in for a moment.
According to Chapin, SPRAY-borne infection, due to Flugge’s droplets, explains “contact infection," i.e. infection in close proximity (2-3 ft).
AIR-borne does not.
According to Chapin, SPRAY-borne infection, due to Flugge’s droplets, explains “contact infection," i.e. infection in close proximity (2-3 ft).
AIR-borne does not.
14/ Chapin says not enough evidence to rule out airborne infection. But still states that airborne infection is nearly impossible (“we are warranted to discard it as a working hypothesis”).
15/ Why does he discard airborne infection?
Because he new that social distance + hygiene worked and:
“It is impossible, as I know from experience, to teach people to avoid contact infection while they are firmly convinced that the air is the chief vehicle of infection.’’
Because he new that social distance + hygiene worked and:
“It is impossible, as I know from experience, to teach people to avoid contact infection while they are firmly convinced that the air is the chief vehicle of infection.’’

16/ Chapin’s position becomes the new paradigm, and it has reigned successfully until now.
Airborne transmission is resisted, as it has for COVID-19. Only very contagious diseases (+TB) are proven, as evidence becomes undeniable.
Airborne transmission is resisted, as it has for COVID-19. Only very contagious diseases (+TB) are proven, as evidence becomes undeniable.
17/ Leading to *confusion of this artifact of history (only v contagious accepted as aerosol), with a law of nature.*
Stated in arguments like "if COVID-19 was aerosol, spread would be much larger, R0 would be much larger, we would see long-range transmission" etc. All false
Stated in arguments like "if COVID-19 was aerosol, spread would be much larger, R0 would be much larger, we would see long-range transmission" etc. All false
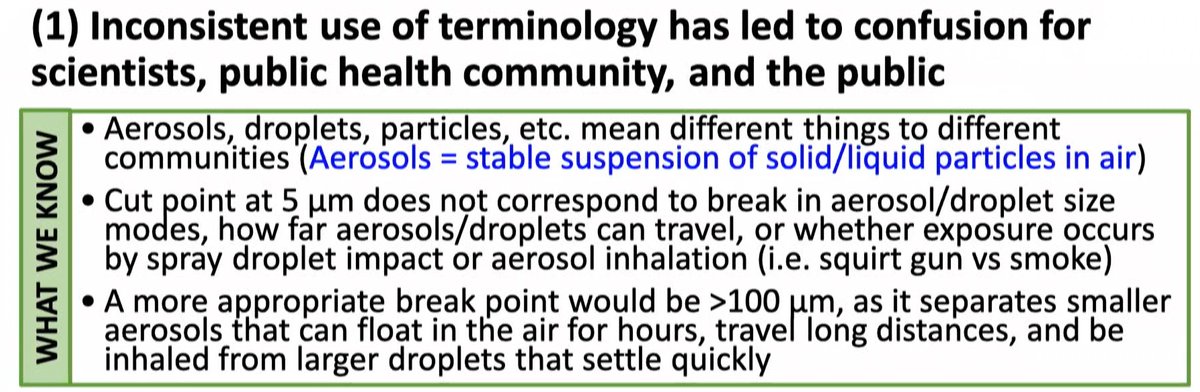
18/ Wells in 1934 at Harvard studies the droplet vs aerosol problem. He correctly determines that the aerosol-droplet separation is at ~100 um.
academic.oup.com/aje/article-ab…
academic.oup.com/aje/article-ab…

19/ Wells clearly defines droplet and airborne infection, consistent with Flugge and Chapin (who had defined “droplet infection proper”).
(Note that “proper droplets” are larger than 100 um, and thus we know now they are not inhalable).
(Note that “proper droplets” are larger than 100 um, and thus we know now they are not inhalable).

20/ Back to the present:
CDC defines droplet infection as caused by projectiles
E.g. see slide from the presentation by Dr. Butler (CDC's Deputy Director for Infectious Diseases) at recent workshop of the US National Academies of Sciences, Engineering, & Medicine (pres. #5):
CDC defines droplet infection as caused by projectiles
E.g. see slide from the presentation by Dr. Butler (CDC's Deputy Director for Infectious Diseases) at recent workshop of the US National Academies of Sciences, Engineering, & Medicine (pres. #5):

21/ As recently as this @NASEM workshop on 26-Aug-2020, CDC was stating (via Dr. Butler) that SARS-CoV-2 was spread mainly through “droplets that can land in the mouth, noses, or eyes of people”
nationalacademies.org/event/08-26-20…
nationalacademies.org/event/08-26-20…

22/ Consistent with historical practice at CDC.
E.g. as summarized in 2007 paper from Y. Li’s group (onlinelibrary.wiley.com/doi/10.1111/j.…), leader in disease transmission. “Droplets [..] are propelled a short distance through the air, and deposited on the host’s [eyes, nostrils], or mouth”
E.g. as summarized in 2007 paper from Y. Li’s group (onlinelibrary.wiley.com/doi/10.1111/j.…), leader in disease transmission. “Droplets [..] are propelled a short distance through the air, and deposited on the host’s [eyes, nostrils], or mouth”

23/ The same is true for the WHO, e.g. their famous video showing the ballistic “angry birds” flight of the droplets (
https://twitter.com/WHO/status/1244258441880797184):

24/ And this is clearly what the latest WHO brief says (9-Jul):
“droplets can reach the mouth, nose, or eyes” while “within 1 metre”. This is consistent with all the historical definition of droplets.
who.int/publications/i…
“droplets can reach the mouth, nose, or eyes” while “within 1 metre”. This is consistent with all the historical definition of droplets.
who.int/publications/i…

25/ It is also discussed in the WHO brief that aerosols could be inhaled and lead to infection.
Note that the word “inhale” is only present in this document for aerosols, and never for droplets.
Note that the word “inhale” is only present in this document for aerosols, and never for droplets.
26/ Also note the dismissive tone about aerosols in the 9-Jul @WHO brief: “hypotheses… theories…” which continues later in the document.
In my experience, nobody has read that document and concluded that aerosols were major. Possible maybe, but very uncertain.
In my experience, nobody has read that document and concluded that aerosols were major. Possible maybe, but very uncertain.
27/ So it is extremely clear what droplets & aerosols are for disease transmission, per history, CDC, WHO
Droplets are ballistic projectiles, fall to the ground 1-2 m, infect by impact on eyes / nostrils / mouth
Aerosols float in air for longer times, and infect by inhalation
Droplets are ballistic projectiles, fall to the ground 1-2 m, infect by impact on eyes / nostrils / mouth
Aerosols float in air for longer times, and infect by inhalation
28/ CRITICAL reminder :
- to be droplet & fall to ground, need > 100 um.
- Being a projectile also requires > 100 um (when talking, a projectile requires > 300 um). See this thread and refs therein:
- to be droplet & fall to ground, need > 100 um.
- Being a projectile also requires > 100 um (when talking, a projectile requires > 300 um). See this thread and refs therein:
https://twitter.com/jljcolorado/status/1292880342227984385
29/ And to be inhalable, need < 100 um. So there is a clear boundary between droplets and aerosols at 100 um
For much of the 20th Century, droplets and aerosols were separated at 100 um for infection purposes in guidance and papers, with references tracing back to Wells (1934)
For much of the 20th Century, droplets and aerosols were separated at 100 um for infection purposes in guidance and papers, with references tracing back to Wells (1934)
30/ But at some point in the later 20th Century, an error is introduced, for reasons we will explain when our history pre-print is available (
As a consequence of the error, health orgs start stating that the droplet-aerosol boundary is at 5 um
https://twitter.com/linseymarr/status/1278036517890347008)
As a consequence of the error, health orgs start stating that the droplet-aerosol boundary is at 5 um
31/ The 5 um error happened long enough ago, that for many people active today, 5 um is the only definition they may have ever known. And it is still an error.
32/ Fauci admitted recently that the 5 um aerosol/droplet boundary is an error:
https://twitter.com/adamhamdy/status/1304120806943928329
33/ The @NASEM workshop also concluded that 100 um is the correct aerosol-droplet boundary, and that 5 um is incorrect 
34/ Indeed 5 um makes no sense.
Particles of 5 um can float in the air for 30 min. This is from the “Aerosol’s 101” tutorial in the CDC webpage (cdc.gov/niosh/topics/a…):
Particles of 5 um can float in the air for 30 min. This is from the “Aerosol’s 101” tutorial in the CDC webpage (cdc.gov/niosh/topics/a…):

35/ However, 5 um error is widely adopted and repeated in many papers and guidance from CDC and WHO for decades.
For example in Klompas et al (2020) in JAMA: jamanetwork.com/journals/jama/… & in very recent paper from key members of the @WHO IPC committee: aricjournal.biomedcentral.com/articles/10.11…
For example in Klompas et al (2020) in JAMA: jamanetwork.com/journals/jama/… & in very recent paper from key members of the @WHO IPC committee: aricjournal.biomedcentral.com/articles/10.11…
36/ Sometimes, Wells (1934) is wrongly cited for the 5 um aerosol/droplet boundary, even though he clearly states > 100 um
We have found no other paper that would support why to define 5 um as anything special in the droplet-aerosol range. (Pls send to me, if you have any)
We have found no other paper that would support why to define 5 um as anything special in the droplet-aerosol range. (Pls send to me, if you have any)
37/ Confusingly, some people (as of today) seem to insist on the 5 um error, and seem to want to define:
(a) Aerosols < 5 um
(b) Inhalable droplets 5-100 um
(c) Ballistic droplets > 100 um
(a) Aerosols < 5 um
(b) Inhalable droplets 5-100 um
(c) Ballistic droplets > 100 um
38/ The “inhalable droplets” are really larger aerosols, according to accepted historical definitions.
Why define as something different particles that stay > 30 min or < 30 min in the air? They both can travel around a room well. It would make no sense to use that definition
Why define as something different particles that stay > 30 min or < 30 min in the air? They both can travel around a room well. It would make no sense to use that definition
39/ I have only seen this strange use of the 5 um boundary in Twitter.
I have been unable to locate a publication that states this distinction explicitly w a reason.
And in particular, I have not found any scientific reason explaining break. If you find one, please send to me
I have been unable to locate a publication that states this distinction explicitly w a reason.
And in particular, I have not found any scientific reason explaining break. If you find one, please send to me
40/ Another definition lurking in Twitter, w/ aerosols/droplet boundary at some unclear size > 5 um.
Despite asking, precise size, or any paper or document supporting and quantifying, have not been provided
I took to calling those the “magic droplets”
Despite asking, precise size, or any paper or document supporting and quantifying, have not been provided
I took to calling those the “magic droplets”
https://twitter.com/jljcolorado/status/1295527045712101376
41/ Magic droplets are droplets most of the time, consistent w/ CDC or WHO "droplets dominate"
But magic d. can behave like aerosols when needed. e.g. to explain the choir outbreak that we recently published, which is unexplainable except for aerosols:
But magic d. can behave like aerosols when needed. e.g. to explain the choir outbreak that we recently published, which is unexplainable except for aerosols:
https://twitter.com/jljcolorado/status/1306450428867964930
42/ Going back to CDC’s update on the modes of transmission, and after reviewing the history, the meaning is clear. INHALATION is the main way in which the virus spreads. This is aerosols and only aerosols. 

43/ Unfortunate that CDC’s text is confusing, also says that droplets can be inhaled. Not consistent w/ CDC’s own definition at @NASEM workshop or historically, nor w/ @WHO’s def., nor w/ historical scientific definitions for 125 years. Hopefully they will fix that error soon
44/ Ballistic droplets, that fall within 1-2 m, are NOT major mode of transmission.
Contrary to @WHO, CDC clearly states that SARS-CoV-2 is airborne. While being less contagious than measles. Thus shared-room-air transmission common --> superspreading. But long-range uncommon
Contrary to @WHO, CDC clearly states that SARS-CoV-2 is airborne. While being less contagious than measles. Thus shared-room-air transmission common --> superspreading. But long-range uncommon
45/ Important: opens the door for targeted controls for aerosols, in US and globally.
See an attempt at tinyurl.com/faqs-aerosol
(tinyurl.com/preguntas-espa… for other languages)
See an attempt at tinyurl.com/faqs-aerosol
(tinyurl.com/preguntas-espa… for other languages)
46/ Existing guidance (some aerosol, not naming it) was not used E.g. we helped @WHO write ventilation guidance.
But made no difference. People reported: not taken seriously or implemented by any government, because after all, the virus was not in the air
But made no difference. People reported: not taken seriously or implemented by any government, because after all, the virus was not in the air
https://twitter.com/MicroLevitator/status/1303837578857242624
47/ In particular I’ve been heart-broken trying to help teachers and parents, in Spanish-speaking countries in particular, where news that the virus could transmit through aerosols was “shocking”, and interviewers stopping me mid-sentence to confirm that they had heard that right
48/ And, as of today, ventilation measures were being FORBIDDEN by schools, companies etc, because the virus was not in the air
https://twitter.com/jessica_bassett/status/1307827288474619904
49/ I suspect SARS-CoV-2 is not isolated case. Likely on the verge of a significant paradigm shift, most respiratory diseases will be reclassified from droplet/fomite to *aerosol*/droplet/fomite
(Some sci. sociology at play? Paradigm shift pushed by “intruders” such as myself)
(Some sci. sociology at play? Paradigm shift pushed by “intruders” such as myself)
50/ Finally undoing the error of Chapin in 1910.
And keeping the useful part: (a) ease of infection at close proximity, social distance works very well to reduce trans.
And discarding the erroneous part: ballistic droplets lead to (a), while aerosols are unimportant
And keeping the useful part: (a) ease of infection at close proximity, social distance works very well to reduce trans.
And discarding the erroneous part: ballistic droplets lead to (a), while aerosols are unimportant
51/ Finally, we have to work together
Epi / PH / ID / virology / aerosol sci.+ need to work closely to figure out many open questions for SARS-CoV-2 trans. & mitigation, & similar questions for many other resp. diseases.
These collab. can lead to major benefits for humanity
Epi / PH / ID / virology / aerosol sci.+ need to work closely to figure out many open questions for SARS-CoV-2 trans. & mitigation, & similar questions for many other resp. diseases.
These collab. can lead to major benefits for humanity
Thread got broken, continues here:
https://twitter.com/jljcolorado/status/1307925764394774528
• • •
Missing some Tweet in this thread? You can try to
force a refresh










