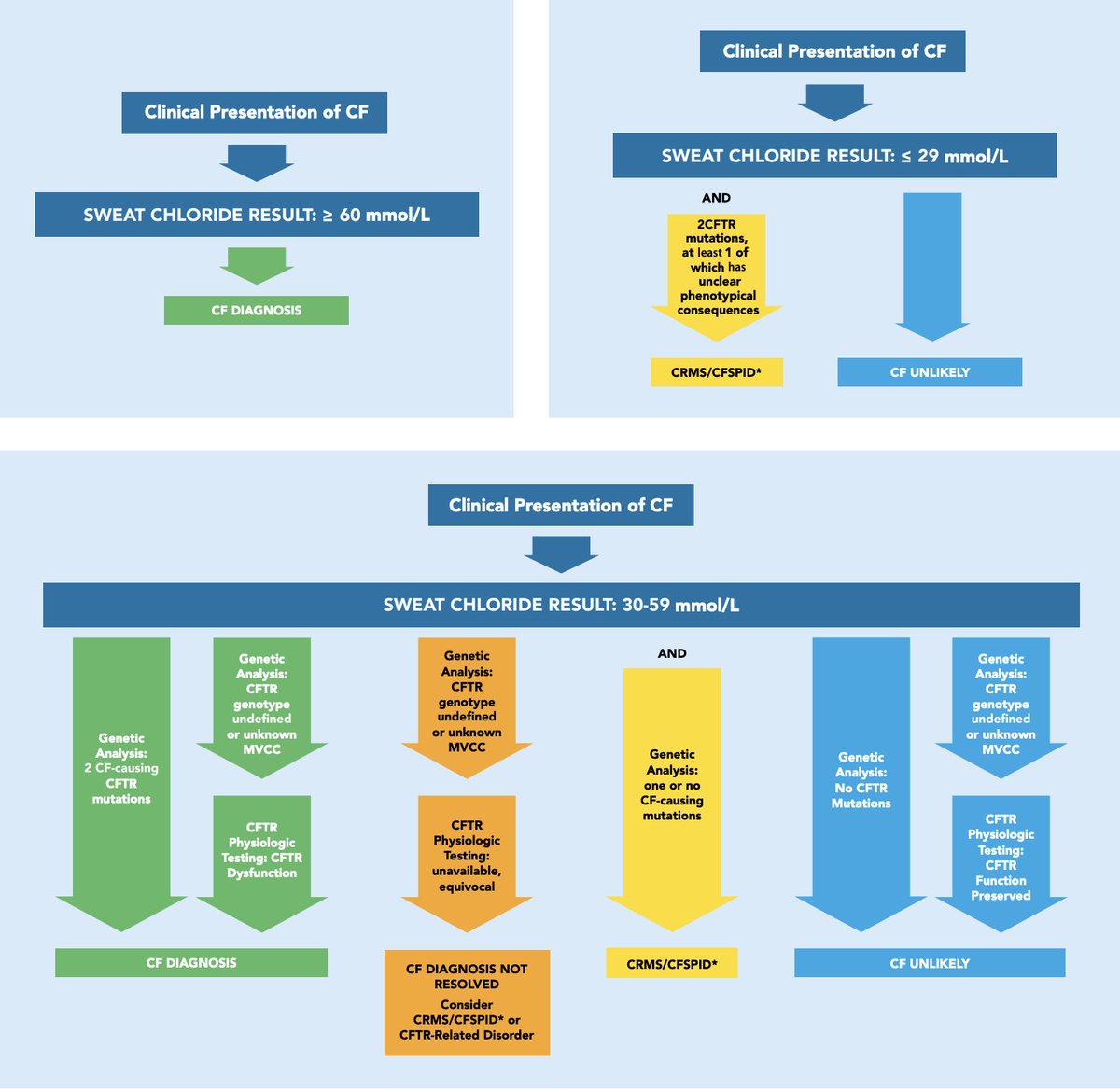
1/Pulmonary embolism is a commonly encountered condition; however, how comfortable are you with the acute diagnosis and treatment of the disease? Let's take a walk through the guidelines. #tweetorial #MedEd @VCU_PCCM @crit_caring_MD @lkbrath @PSinkam @AvrahamCooperMD @VCU_IMRes 
2/ Venous thromboembolism is currently the 3rd most frequent acute cardiovascular syndrome encountered globally with an annual incidence rate ranging from 39-155 per 100,0000 population. bit.ly/3j4iP2s @michellebr00ks @cjchiu @mdlizs @mkashiouris @B_M_Wiese @ptfaddenMD
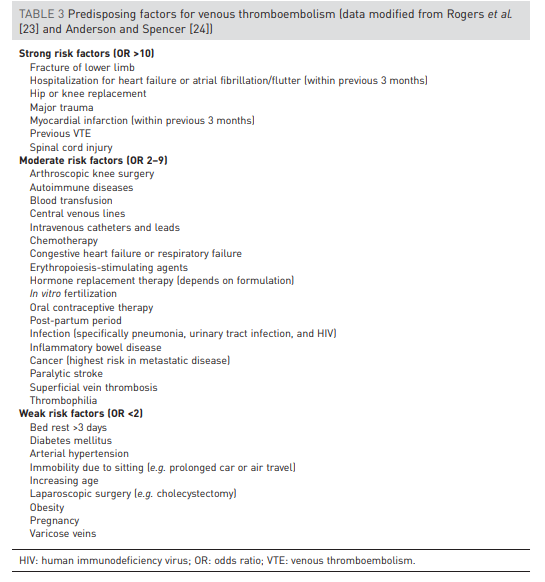
3/This chart by Rogers, Anderson, and Spencer found in the @EuroRespSoc guidelines displays predisposing risk factors for VTE based on odds ratios. Check out all the risk factors with an odds ratio >10! @DxRxEdu @rabihmgeha @CPSolvers @AdamRodmanMD @tony_breu @KevinSwiatek 
4/The pathophysiology of an acute pulmonary embolism can be quite complex; however, this can be simplified to an acute rise in pulmonary arterial pressures leading to right sided heart failure. @cderekleiner @rvawellmd @scall1200 @MedEdPGH @PaulNWilliamz @DoctorWatto @BrighamSK 

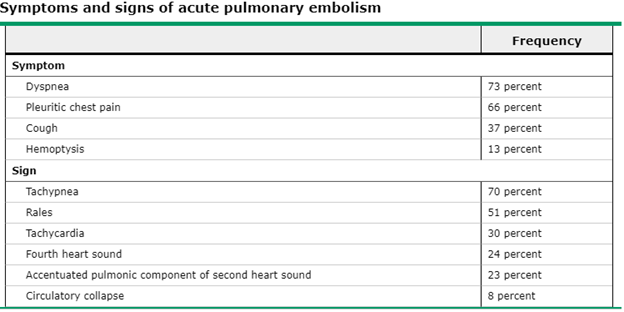
5/According to a meta-analysis of 19 studies with 25,343 patients, clinical suspicion of PE had a sensitivity 85% with specificity 51%. This table developed from the PIOPED study demonstrates common signs and symptoms of acute PE. @thecurbsiders @aoglasser @gradydoctor @UpToDate 
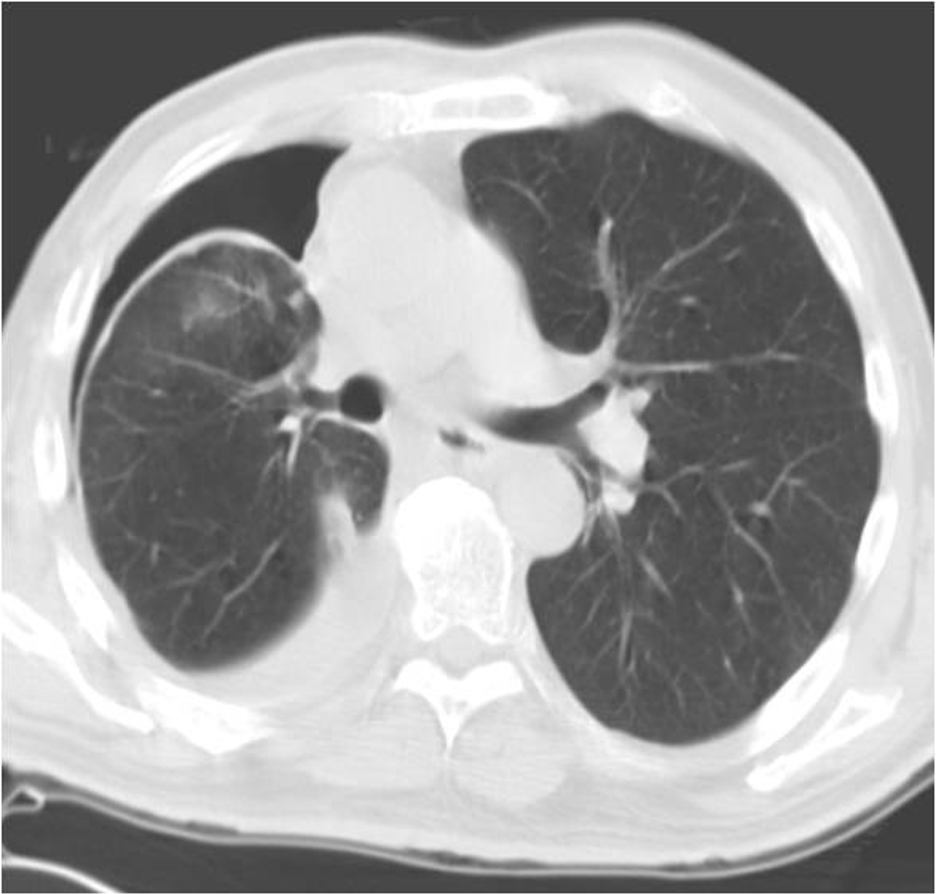
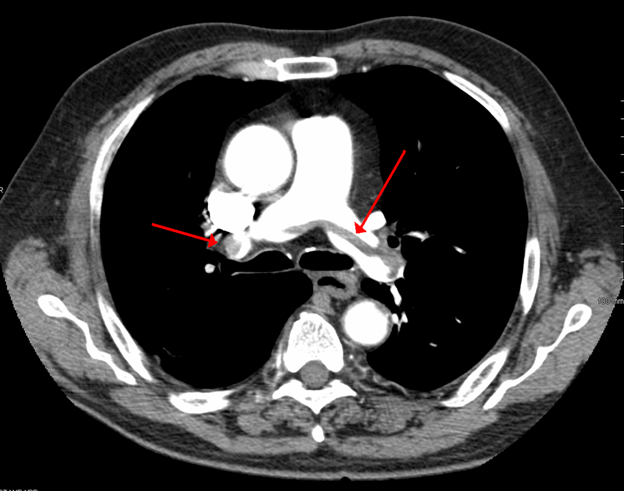
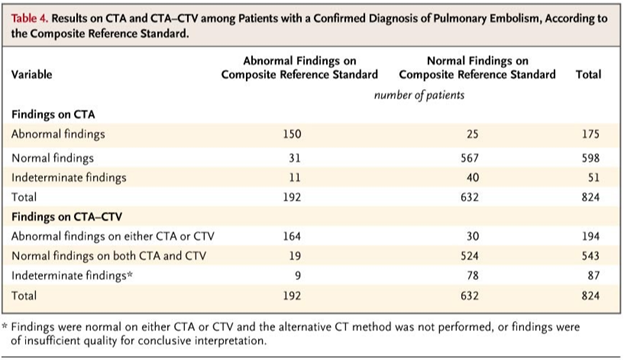
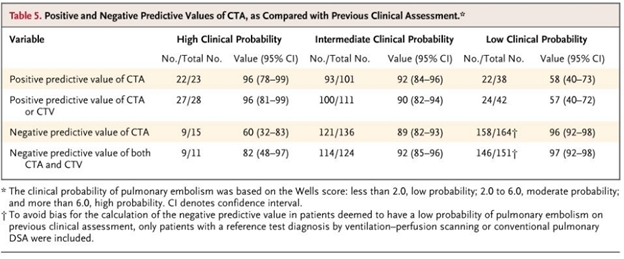
6/ CTA chest remains the method of choice for imaging the pulmonary vasculature in patients with suspected PE. The PIOPED II trial in @NEJM demonstrated a sensitivity 83%, specificity 96% for PE diagnosis using CTA chest and also exhibited the importance of clinical probability. 

7/ Bedside ultrasonography can also be a vital tool as it can provide clinicians with a real-time assessment of the right ventricle. This chart found in the @EuroRespSoc guidelines demonstrates graphically some of the various echocardiogram signs of an acute PE. @gsmartinmd 

8/Risk stratification remains one of the most critically important and challenging steps in the management of patients with PE. A variety of tools have been developed for risk stratification, including the Pulmonary Embolism Severity Indexes. However, VITAL SIGNS remain key! 


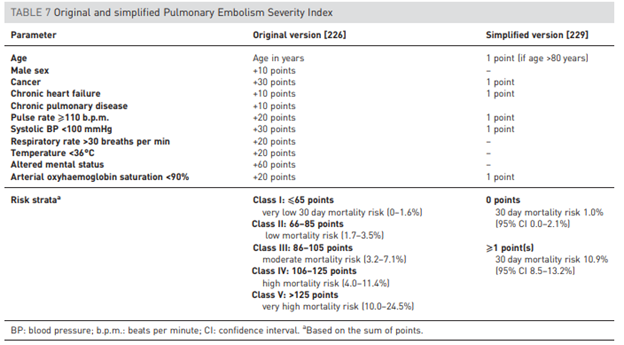

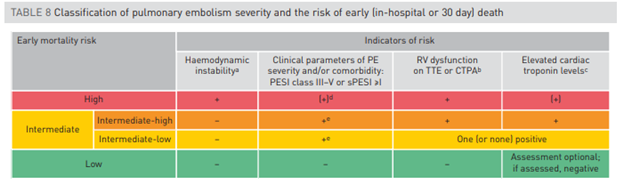
9/ Various biomarkers have been evaluated to help with risk stratification. A meta-analysis showed ⬆️troponin concentrations were associated with ⬆️mortality (OR 5.2). Elevated BNP was also associated with 10% risk of early death @AjayPMD @jackpenner @NateWarnerMD @PulmCrit
10/ This flow chart from @EuroRespSoc guidelines demonstrates appropriate initial management for patients with acute PE based on hemodynamics and risk stratification systems. Of note, even those in the intermediate-high risk category may be candidates for thrombolytics. 
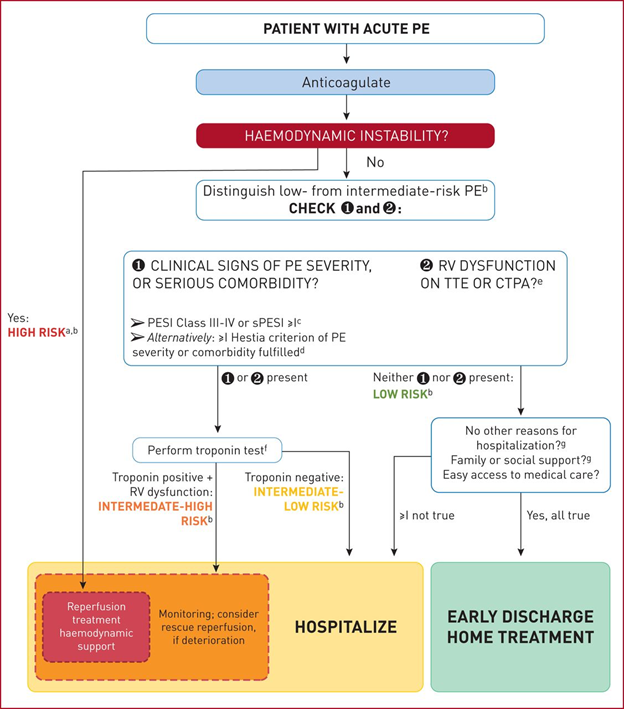
11/ Initial management for patients with hemodynamic instability from acute pulmonary embolism should focus on hemodynamic support and reperfusion therapy. In high risk PE patients, initiate anticoagulation with UFH without delay. 
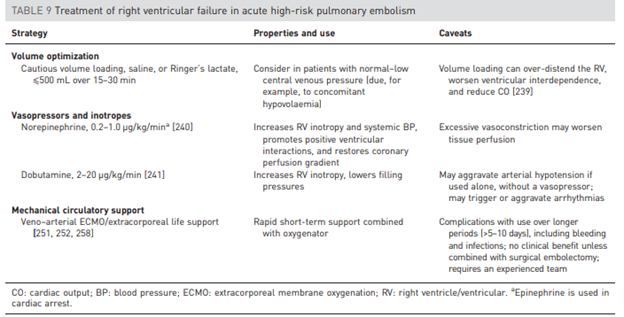
12/ There are various reperfusion strategies: systemic thrombolytics, catheter-directed thrombolytics, surgical embolectomy, and mechanical thrombectomy. @ERitterMD @RabiaQaiser3 @MarkZieglerMD @ReenaHem @TheRealDSrini 






13/ The PEITHO trial (2014) showed that among patients with sub-massive PE (hemodynamic stable with RV strain and ⬆️troponin) being treated with UFH and received systemic thrombolytics there was a ⬇️in all-cause mortality and hemodynamic decompensation at 7 days. 


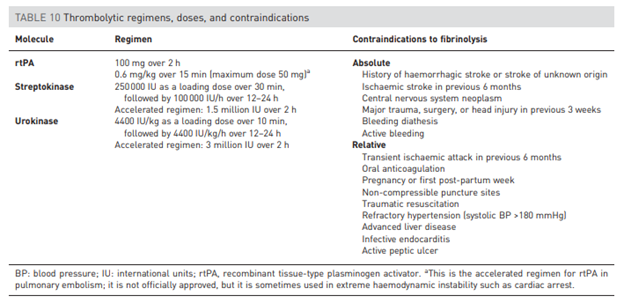
14/ This table provides an overview of the most common thrombolytic regimens with their doses and absolute/relative contraindications. 
15/ Few studies have evaluated catheter-directed thrombolytics. The ULTIMA study (2013) showed catheter directed thrombolytics to be superior to heparin alone in improving RV/LV ratio and recovery of RV systolic function. However, would interpret with caution.
16/ Surgical thrombectomy can be considered in the following situations:
1⃣PE with failure of other interventions
2⃣Absolute contraindication to thrombolysis
3⃣Clot in transit across PFO
1⃣PE with failure of other interventions
2⃣Absolute contraindication to thrombolysis
3⃣Clot in transit across PFO
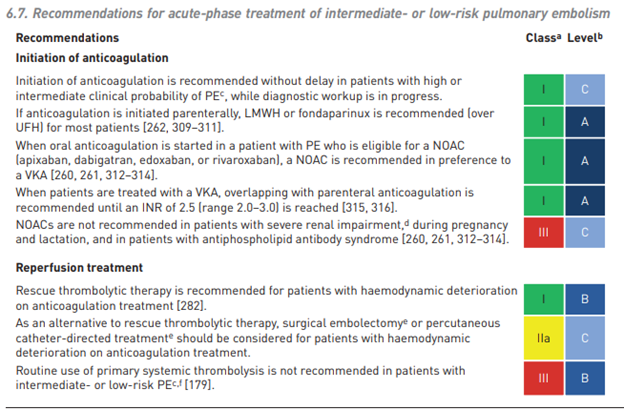
17/ Anticoagulation with preferably LMWH is recommended for acute treatment in those individuals with intermediate or low risk PE. Additionally, don’t forget that NOACs are now preferred to VKA for oral anticoagulation. 
18/ The diagnosis and management of acute pulmonary embolus can be quite overwhelming. Hope this helps! For further reading, check out the 2019 @EuroRespSoc guidelines. Thanks! bit.ly/2Hxa3fv
• • •
Missing some Tweet in this thread? You can try to
force a refresh