1/ Supervisor's 💭
Why isn’t the heparin drip ordered yet? I’ll just order it...
Trainee's 💭
Why am I even here? My supervisor repeats everything I do. Do they even trust me?
How can we balance supervision w/ autonomy?
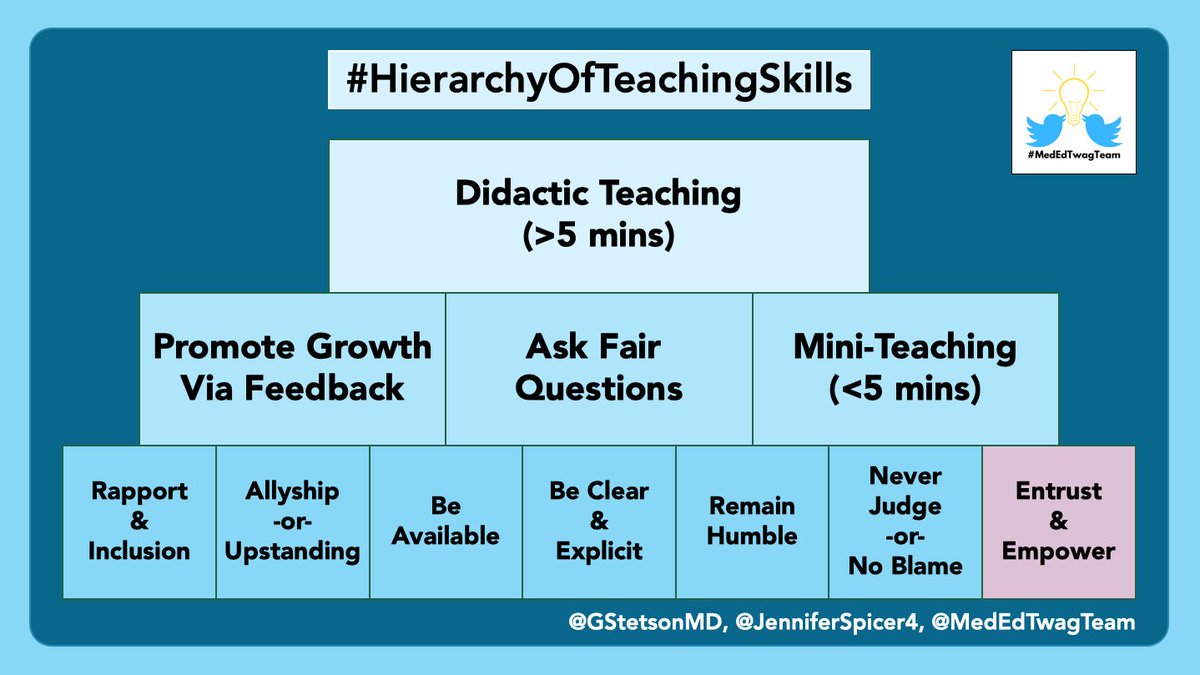
This week’s #MedEdTwagTeam topic: Trust & Empower
#MedEd
Why isn’t the heparin drip ordered yet? I’ll just order it...
Trainee's 💭
Why am I even here? My supervisor repeats everything I do. Do they even trust me?
How can we balance supervision w/ autonomy?
This week’s #MedEdTwagTeam topic: Trust & Empower
#MedEd

2/ This week’s discussion is our final @MedEdTwagTeam thread on foundational #ClinicalTeaching skills.
We discuss entrustment & empowerment, which are key to promoting *appropriate* autonomy.
If you missed @GStetsonMD’s thread last week, check it out:

We discuss entrustment & empowerment, which are key to promoting *appropriate* autonomy.
If you missed @GStetsonMD’s thread last week, check it out:
https://twitter.com/GStetsonMD/status/1308403409649889281
3/ So what are entrustment & empowerment, and why do they matter in #MedEd?
The article below in @AcadMedJournal provides a helpful definition of entrustment:
journals.lww.com/academicmedici…
When supervisors entrust trainees,
it empowers trainees.
It provides them with autonomy.
The article below in @AcadMedJournal provides a helpful definition of entrustment:
journals.lww.com/academicmedici…
When supervisors entrust trainees,
it empowers trainees.
It provides them with autonomy.

4/ And *appropriate* autonomy leads to meaningful work.
Empowerment motivates individuals, as outlined in this @HarvardBiz article.
hbr.org/2018/03/when-e…
But the key is identifying the *appropriate* level of autonomy.
That’s what we will discuss today.
Empowerment motivates individuals, as outlined in this @HarvardBiz article.
hbr.org/2018/03/when-e…
But the key is identifying the *appropriate* level of autonomy.
That’s what we will discuss today.
5/ You may remember this image from @GStetsonMD last week based on Vygotsky’s zones of proximal development.
The key to entrustment & empowerment is:
✅identifying what our learners can do (allowing entrustment)
✅giving them with autonomy for those tasks (providing empowerment)
The key to entrustment & empowerment is:
✅identifying what our learners can do (allowing entrustment)
✅giving them with autonomy for those tasks (providing empowerment)

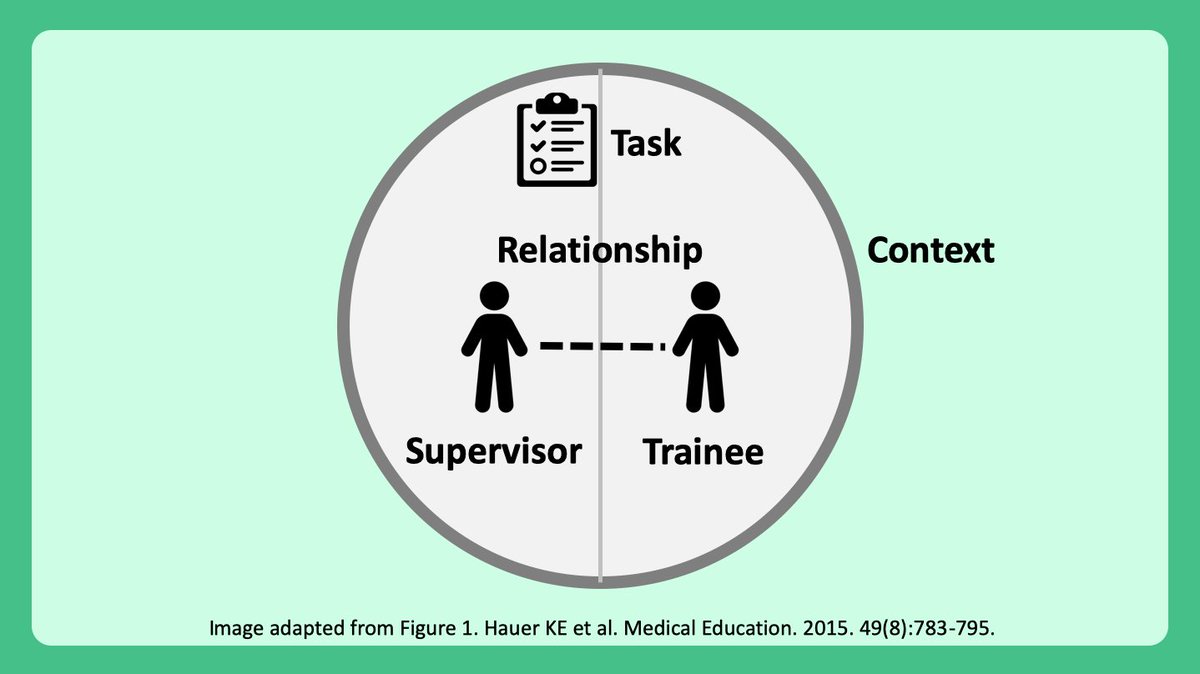
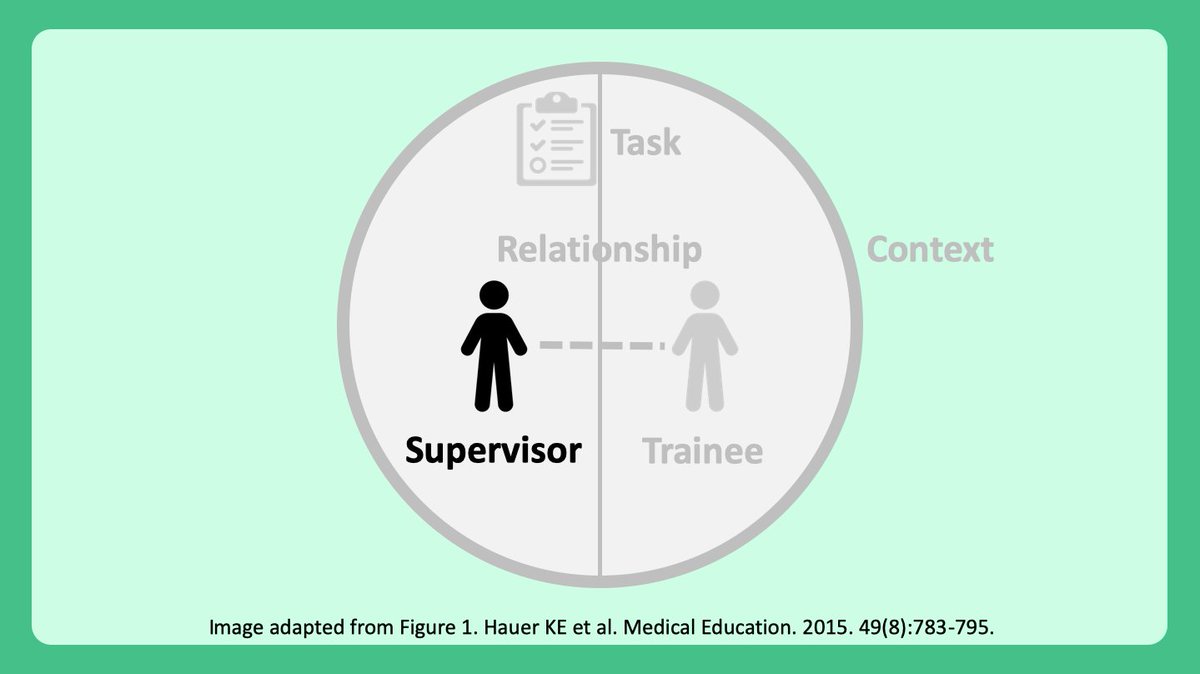
6/ Balancing supervision & oversight w/ learner autonomy & empowerment is complex.
Trust or “entrustment” is essential, which is influenced by 5 factors:
1⃣Supervisor
2⃣Trainee
3⃣Trainee-supervisor relationship
4⃣Task/activity
5⃣Context
Trust or “entrustment” is essential, which is influenced by 5 factors:
1⃣Supervisor
2⃣Trainee
3⃣Trainee-supervisor relationship
4⃣Task/activity
5⃣Context
7/ Before getting going further, I want to emphasize that the “supervisor” can be anyone in a supervisory role:
Intern ➡️ medical student
Resident ➡️ intern
Fellow ➡️ resident
Attending ➡️ team
So let’s discuss some concrete things that all of us can do to entrust & empower.
Intern ➡️ medical student
Resident ➡️ intern
Fellow ➡️ resident
Attending ➡️ team
So let’s discuss some concrete things that all of us can do to entrust & empower.
8/ First, as a supervisor, we need to recognize that many factors influence our ability to trust.
*⃣Clinical experience
*⃣Experience with supervising others
*⃣Familiarity with clinical context/setting
*⃣Clinical experience
*⃣Experience with supervising others
*⃣Familiarity with clinical context/setting
9/ Supervisor experience, in particular, influences trust and supervision based on this qualitative study in @AcadMedJournal by @lesliesheu
journals.lww.com/academicmedici…
In general, early supervisors provide less autonomy than experienced supervisors.
journals.lww.com/academicmedici…
In general, early supervisors provide less autonomy than experienced supervisors.

10/ So as supervisors, what can we do to entrust & empower our learners?
Observe your learners & “diagnose” where their current abilities lie within this framework.
Observe your learners & “diagnose” where their current abilities lie within this framework.

11/ Here are some ways that we as supervisors can assess our learners including:
*⃣Direct patient care activities (e.g. taking a history
*⃣Proxies to patient care (e.g. listening to them present the history)
These assessments provide complementary information.
*⃣Direct patient care activities (e.g. taking a history
*⃣Proxies to patient care (e.g. listening to them present the history)
These assessments provide complementary information.

12/ And residents, remember that you are supervisors too!
All of these same rules apply.
This article in @AcadMedJournal by @lesliesheu specifically highlights how trust develops between residents & interns:
journals.lww.com/academicmedici…
TL;DR:
It’s similar
All of these same rules apply.
This article in @AcadMedJournal by @lesliesheu specifically highlights how trust develops between residents & interns:
journals.lww.com/academicmedici…
TL;DR:
It’s similar
13/ Developing a strong relationship with learners helps.
And many of our prior #MedEdTwagTeam #TuesdayTweetorials provide tips that help build relationships.
Check out all of them here:
twitter.com/i/events/12908…
And many of our prior #MedEdTwagTeam #TuesdayTweetorials provide tips that help build relationships.
Check out all of them here:
twitter.com/i/events/12908…

14/ But what can trainees do to encourage supervisors to trust them?
A number of things including:
*⃣Be honest/truthful
*⃣Be reliable/responsible
*⃣Recognize limitations & ask for help
*⃣Be open to feedback
And yes, clinical knowledge helps. But honestly, that’s less important
A number of things including:
*⃣Be honest/truthful
*⃣Be reliable/responsible
*⃣Recognize limitations & ask for help
*⃣Be open to feedback
And yes, clinical knowledge helps. But honestly, that’s less important

15/ Now lastly, it’s important to emphasize that the task & the context matter.
Here are some factors that impact entrustment:
✅Task: complexity, urgency, and patient risk
✅Context: resources, staffing, culture, hectic circumstances, time of day
Here are some factors that impact entrustment:
✅Task: complexity, urgency, and patient risk
✅Context: resources, staffing, culture, hectic circumstances, time of day

16/ And remember that you want to give your learners the “right” amount of entrustment.
Too little: learners frustrated they aren’t empowered (“Why am I here?”)
Too much: learners frustrated b/c they fail (“I can’t do this”)
Just right: leads to learner satisfaction & meaning
Too little: learners frustrated they aren’t empowered (“Why am I here?”)
Too much: learners frustrated b/c they fail (“I can’t do this”)
Just right: leads to learner satisfaction & meaning

17/ So, in summary, what can we do to entrust & empower out trainees?
We need to:
✅Set clear expectations
✅Observe & evaluate our learners
✅Provide clear feedback
And then consider how these 5 factors influence our entrustment decisions.
We need to:
✅Set clear expectations
✅Observe & evaluate our learners
✅Provide clear feedback
And then consider how these 5 factors influence our entrustment decisions.

18/ This week’s discussion was our final @MedEdTwagTeam thread on the foundational #ClinicalTeaching skills.
Watch out for our future topics:
*⃣Feedback
*⃣Asking questions
*⃣Mini-teaching
Check out the @MedEdTwagTeam to see all of our threads in one place!
Thanks for joining!
Watch out for our future topics:
*⃣Feedback
*⃣Asking questions
*⃣Mini-teaching
Check out the @MedEdTwagTeam to see all of our threads in one place!
Thanks for joining!

@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh