The Glasgow Coma Scale is a widespread and important tool for discussing conscious level. After all, "what's the GCS?", barked the stereotypical neurosurgeon at the cowering FY1. But why?!
Well, I can't answer that. But let's think about the GCS in this #tweetorial. #MedEd 1/15
Well, I can't answer that. But let's think about the GCS in this #tweetorial. #MedEd 1/15
The GCS was described by Graham Teasdale and Bryan Jennett in 1974. It consists of 3 categories - best eye-opening (E), best verbal (V) and best motor response (M). 2/15 
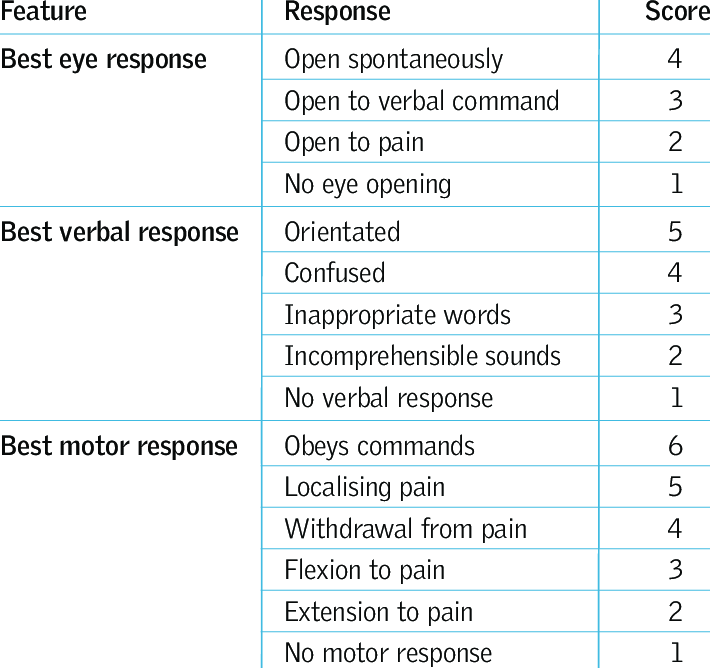
These 3 categories are not related in any way, so a composite value /15 makes little sense. It's not linear - so a drop of 2 from 14/15 to 12/15 is very different to a drop of 2 from 6/15 to 4/15.
For this reason, it should *always* be broken down into its 3 categories. 3/15
For this reason, it should *always* be broken down into its 3 categories. 3/15
In fact, at @INSNeurosurgery where the GCS was devised, you won't hear a number spoken - a handover might be 'he was flexing, no eyes, no verbal'. The GCS just provides a common structure and language for discussing conscious level. 4/15
And ever wondered why the lowest score is 3, with 1 for each category?
The GCS was designed as a data analysis tool for monitoring the depth of coma over time. Computers don't like zero. 5/15
The GCS was designed as a data analysis tool for monitoring the depth of coma over time. Computers don't like zero. 5/15
But it's the M score that neurosurgeons wax lyrical about. Why is this?
There are lots of reasons for deteriorations in E and V - syncope, hypoglycaemia, sepsis, TIA/stroke, seizure, sleep...
But M gives you a linear picture of brain function. Let me show you how. 6/15
There are lots of reasons for deteriorations in E and V - syncope, hypoglycaemia, sepsis, TIA/stroke, seizure, sleep...
But M gives you a linear picture of brain function. Let me show you how. 6/15
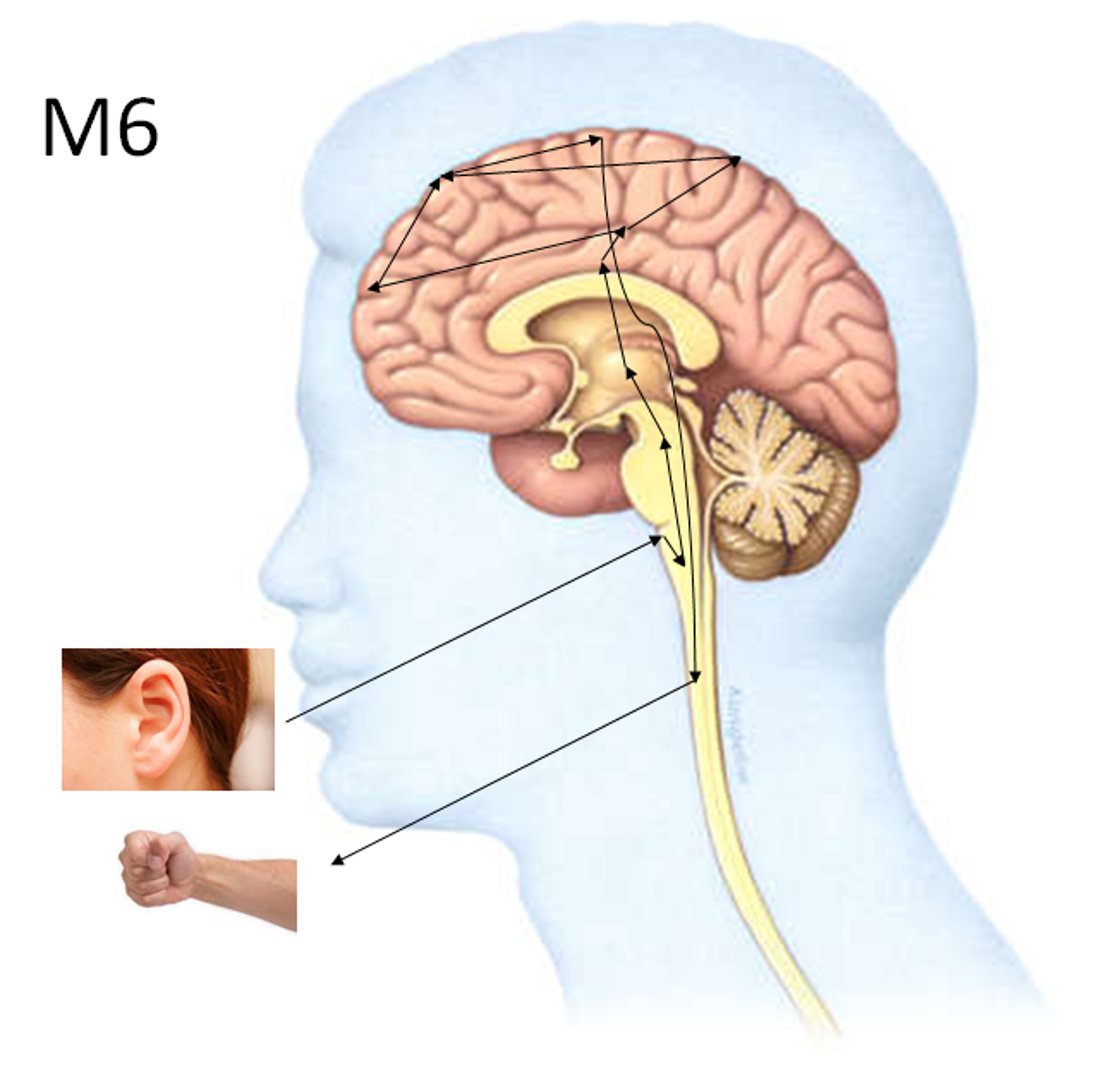
M6. "Squeeze my hand" - a simple command. But it invokes complex polysynaptic brainstem and bilateral cortical auditory processing, parietal 'conscious association' areas, premotor and motor areas for voluntary control. You need your whole brain to obey a command. 7/15 
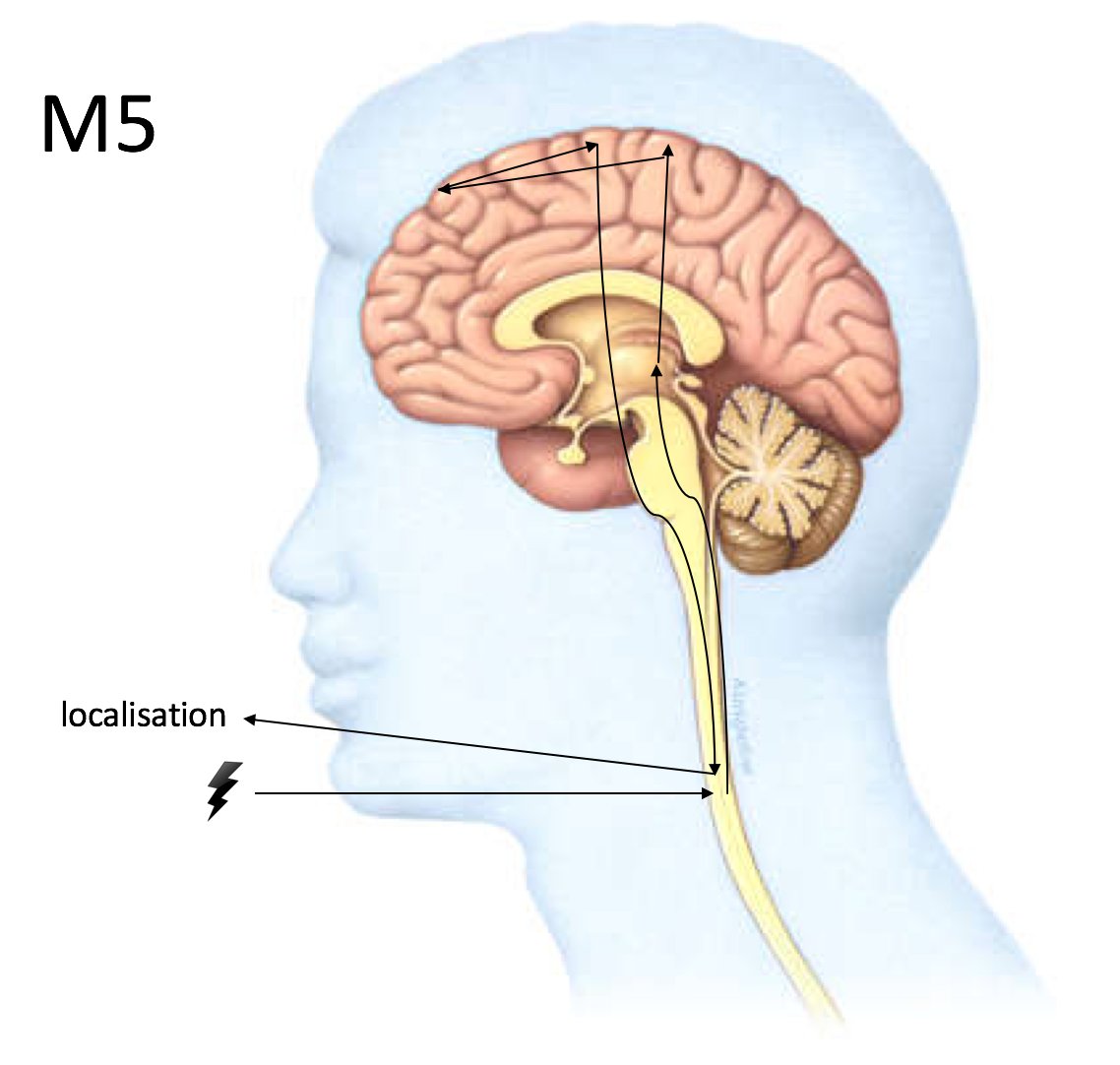
M5. An unconscious response but you can localise your hand reasonably accurately to the site of the painful stimulus. This requires polysynaptic cortical processing through motor planning areas. Most of the cortex, and everything below it, is working. 8/15 
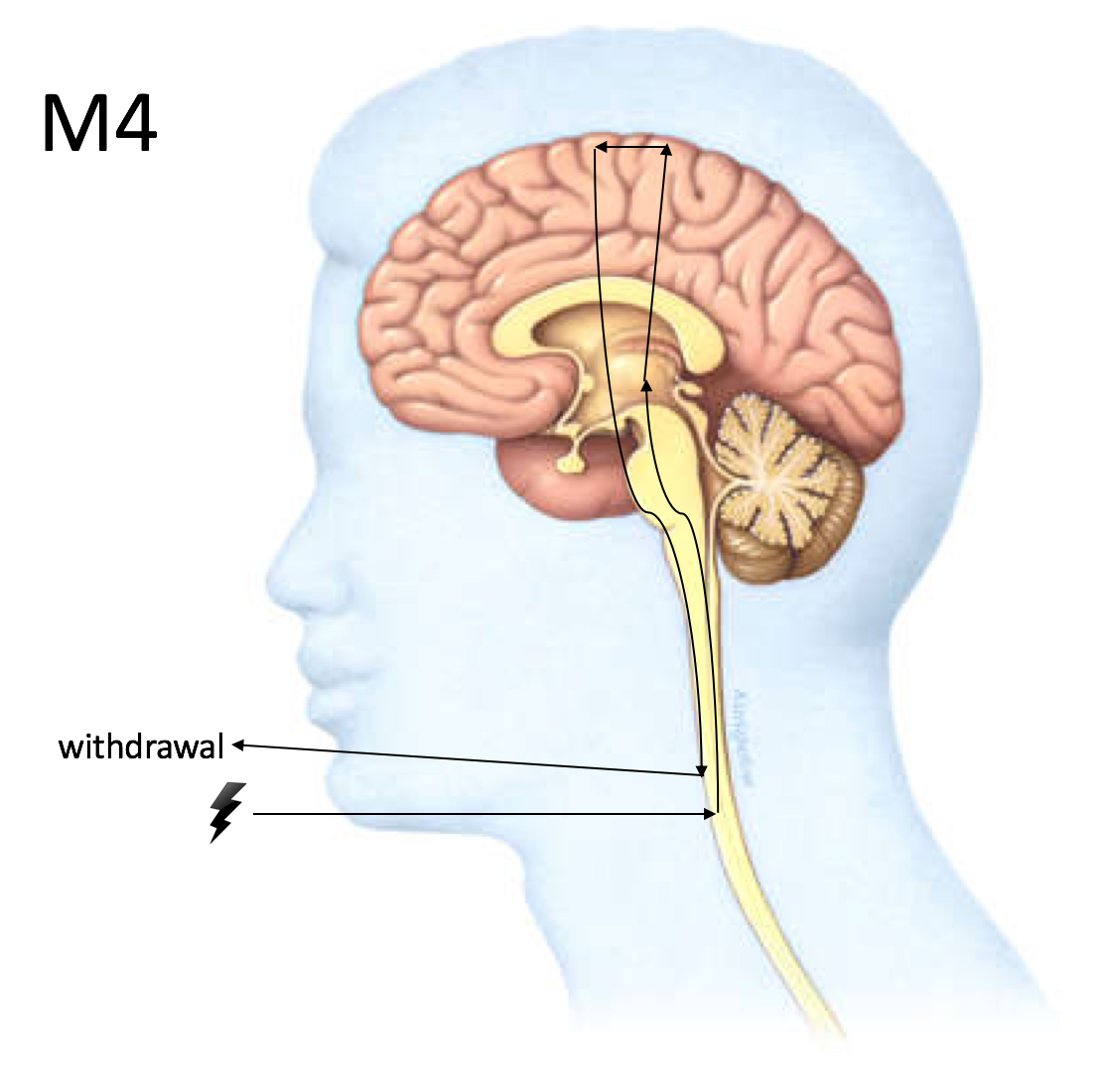
M4. This is 'almost' localising, but the motor planning just isn't there, resulting in more of a general movement in the right direction. It's a simple motor cortex action without any of the refinement of the localising response - but still implies reasonable brain function. 9/15 
M3. What happens when cortical control of movement (corticospinal tract) is out? The more primitive motor tracts take over. The highest, at the midbrain, is the rubrospinal tract. This is the tract that makes you automatically shield your face from looming harm - flexion. 10/15 

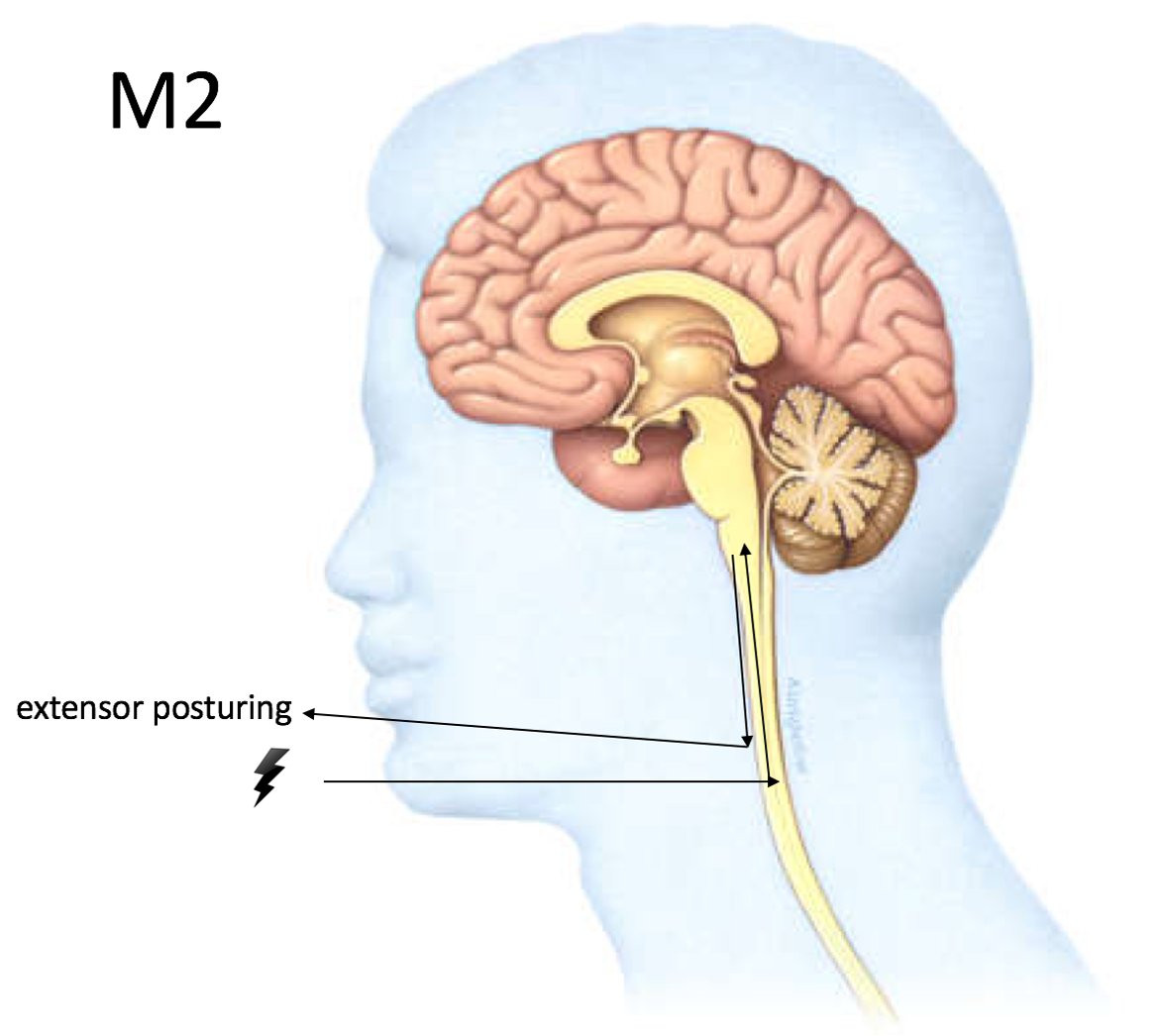
M2. With the midbrain out, next up are vestibulospinal/reticulospinal tracts in the medulla. These evolutionarily ancient tracts are conserved from quadrupeds, in which they produce upright posture - think of a dog, which extends all four limbs and neck to stand upright. 11/15 
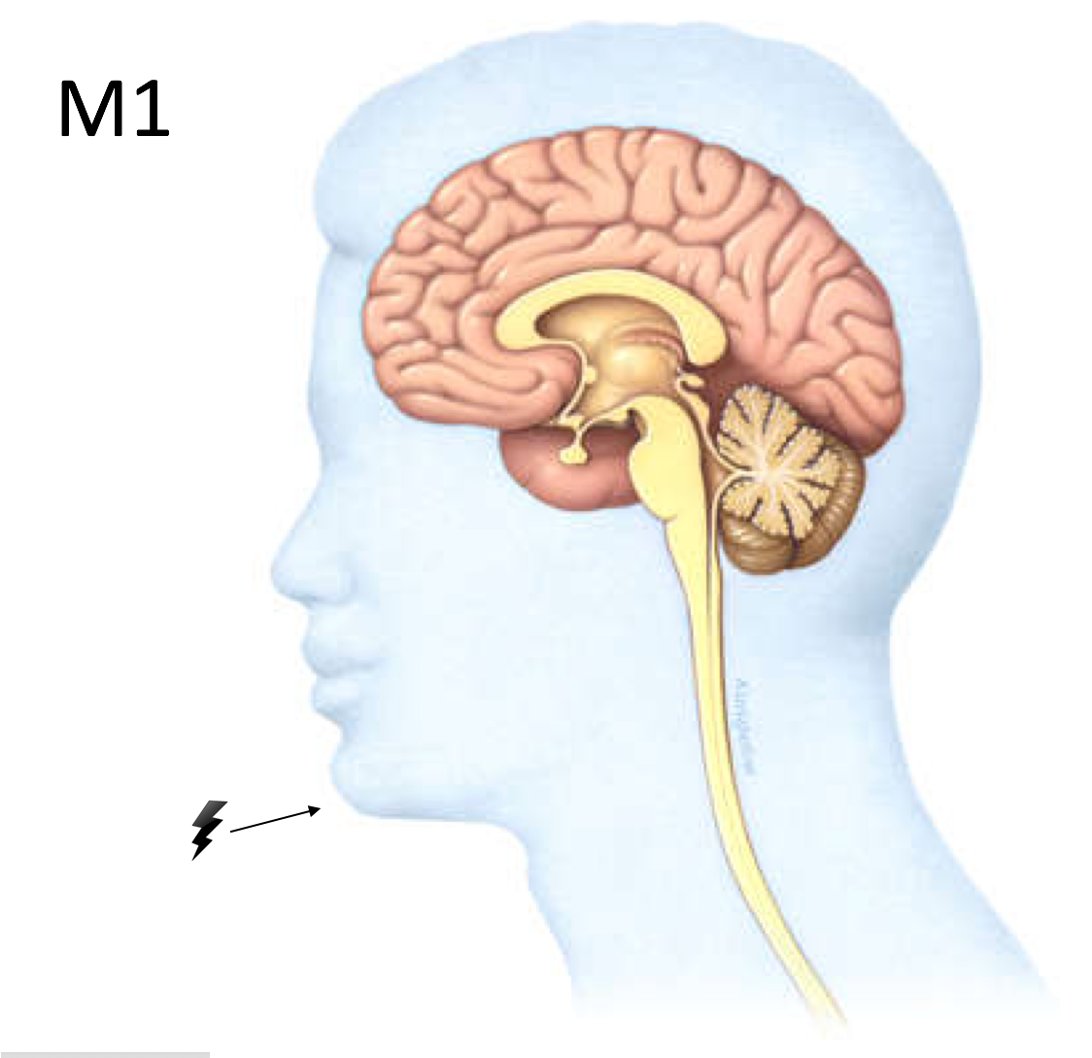
M1. Finally the lowest M score - no response at all. Hopefully you can see from these diagrams that brain function is reflected in the motor score in a way that is structurally quite linear, and this is why it is so useful. 12/15 
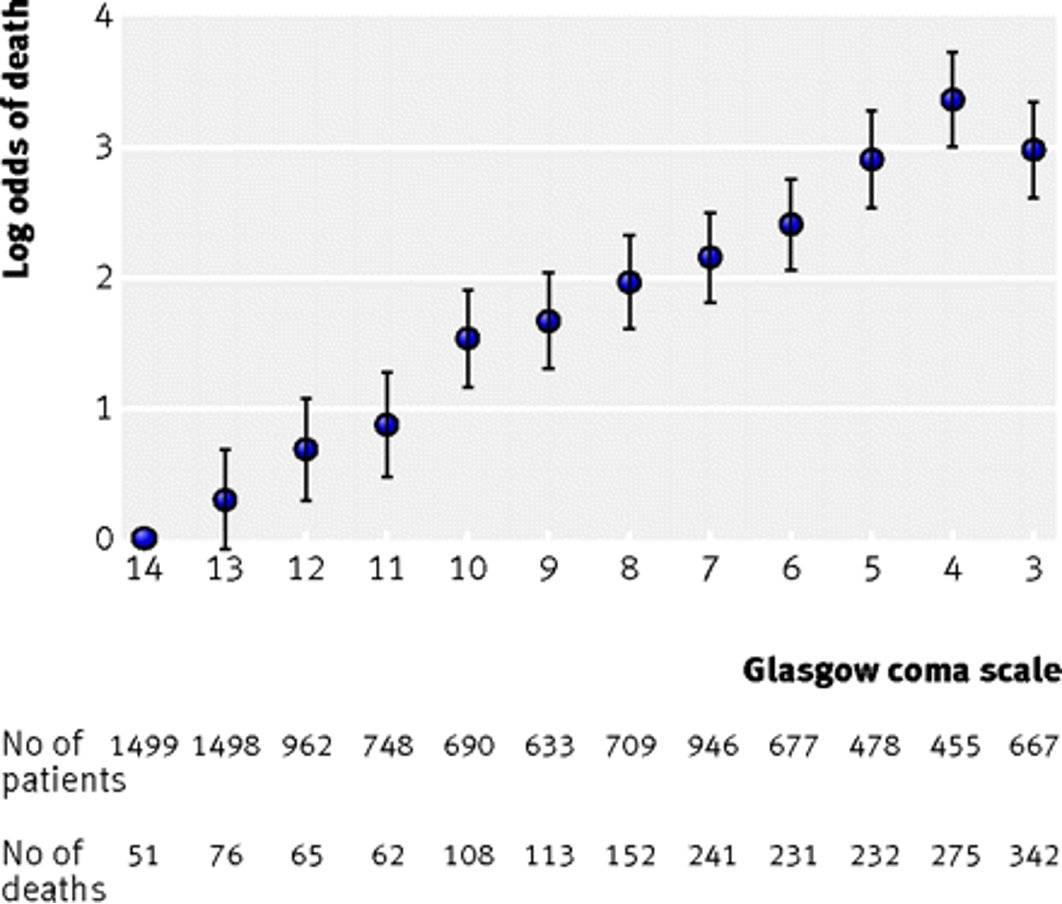
The GCS is linked very closely to prognosis in conditions such as traumatic brain injury and subarachnoid haemorrhage. So getting a handle on the initial breakdown and how this has changed over time can be of crucial importance and really affects treatment by neurosurgeons. 13/15
In fact, prognosis in TBI is linked linearly with initial GCS. The one exception - when it's 4/15.
Why? There are lots of confounding reasons to be GCS 3/15, but extensor posturing (GCS 4/15) implies a devastating structural brain problem. See this data from CRASH. 14/15
Why? There are lots of confounding reasons to be GCS 3/15, but extensor posturing (GCS 4/15) implies a devastating structural brain problem. See this data from CRASH. 14/15
I hope this has made clearer to some the neurological basis for the GCS, and helped to explain why neurosurgeons seem to only care about one thing.
It's because it really matters! Thanks for reading. 15/15
It's because it really matters! Thanks for reading. 15/15
• • •
Missing some Tweet in this thread? You can try to
force a refresh





