@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty 1/ 35 y/o M presents with fatigue & generalized pruritus x 6weeks. No skin rash, No abdo pain, diarrhea or 🩸 in stool. AST 62 ALT 64 ALP 435 Tbili 1.3. MRI/MRCP: multifocal strictures & areas of dilatation of intra +extra hepatic ducts. What’s the next step?💡 #Back2Basics #B2B
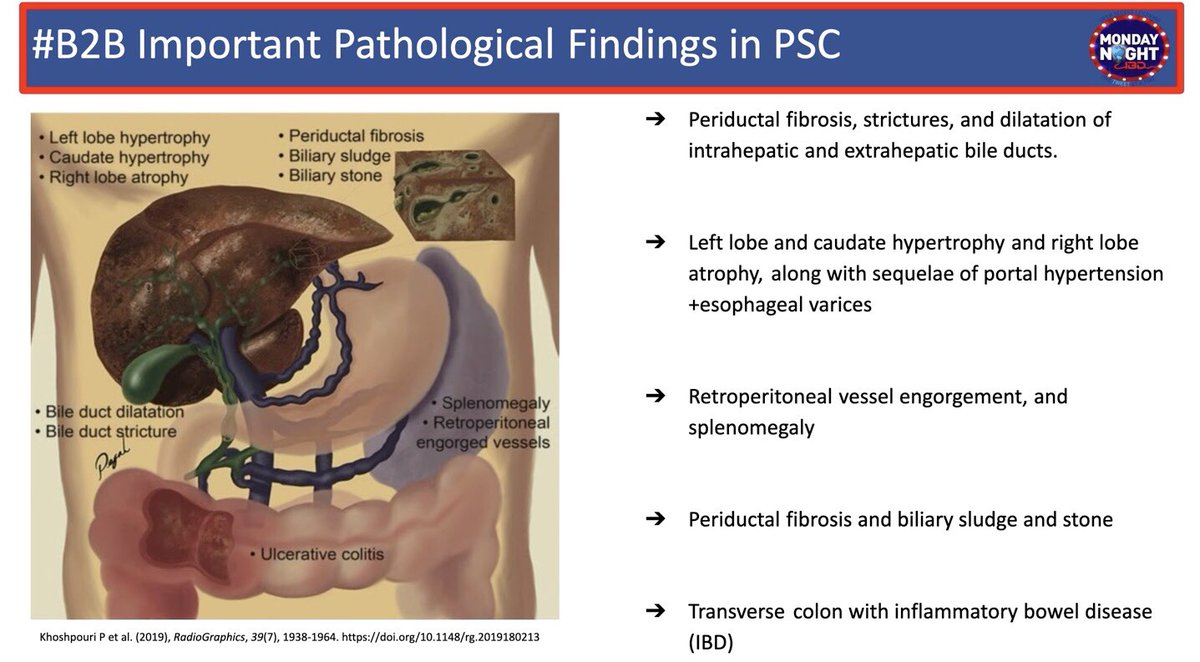
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty 2/ What’s #PSC & phenotypes?
🧩Idiopathic chronic inflam dis. of the biliary tree
🧩90%: Large ducts (LD): "Beads on string appearance” on ERCP/MRCP (pt👆)
🧩5% Small IHD only: nml MRCP, dx by liver bx, slide👇
🧩5% PSC w AIH overlap: abnl MRCP+liver bx w⬆️AST/ALT or IgG

🧩Idiopathic chronic inflam dis. of the biliary tree
🧩90%: Large ducts (LD): "Beads on string appearance” on ERCP/MRCP (pt👆)
🧩5% Small IHD only: nml MRCP, dx by liver bx, slide👇
🧩5% PSC w AIH overlap: abnl MRCP+liver bx w⬆️AST/ALT or IgG

@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty 3/ 💎#B2BPearl #PSC w ⬆️IgG4
📌15% of LD-PSC
📌⬆️IgG4 serum>140mg/dL +/- tissue
💎✅IgG4 at least once w PSC dx
📌Assoc. w AI pancreatitis; other Ig4 dis.
💎⬆️severity of UC, colectomy
📌More rapid progression to cirhhosis
💎Steroid responsive: ️ ⬇️AlPhos, TBili, IgG4
📌15% of LD-PSC
📌⬆️IgG4 serum>140mg/dL +/- tissue
💎✅IgG4 at least once w PSC dx
📌Assoc. w AI pancreatitis; other Ig4 dis.
💎⬆️severity of UC, colectomy
📌More rapid progression to cirhhosis
💎Steroid responsive: ️ ⬇️AlPhos, TBili, IgG4
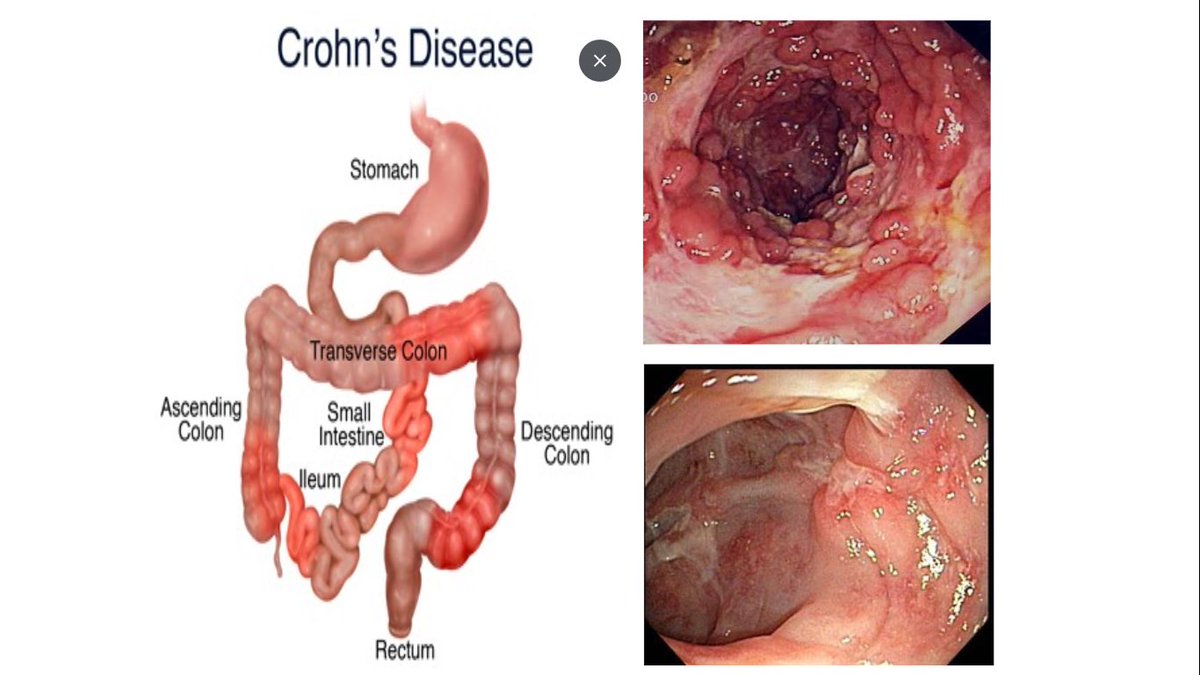
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty 4/📍#PSC and #IBD:
📍2-7% of UC have PSC
📍80% of PSC have IBD: UC>CD
✅C-scope in all new dx PSC w bx even if no GI Sx
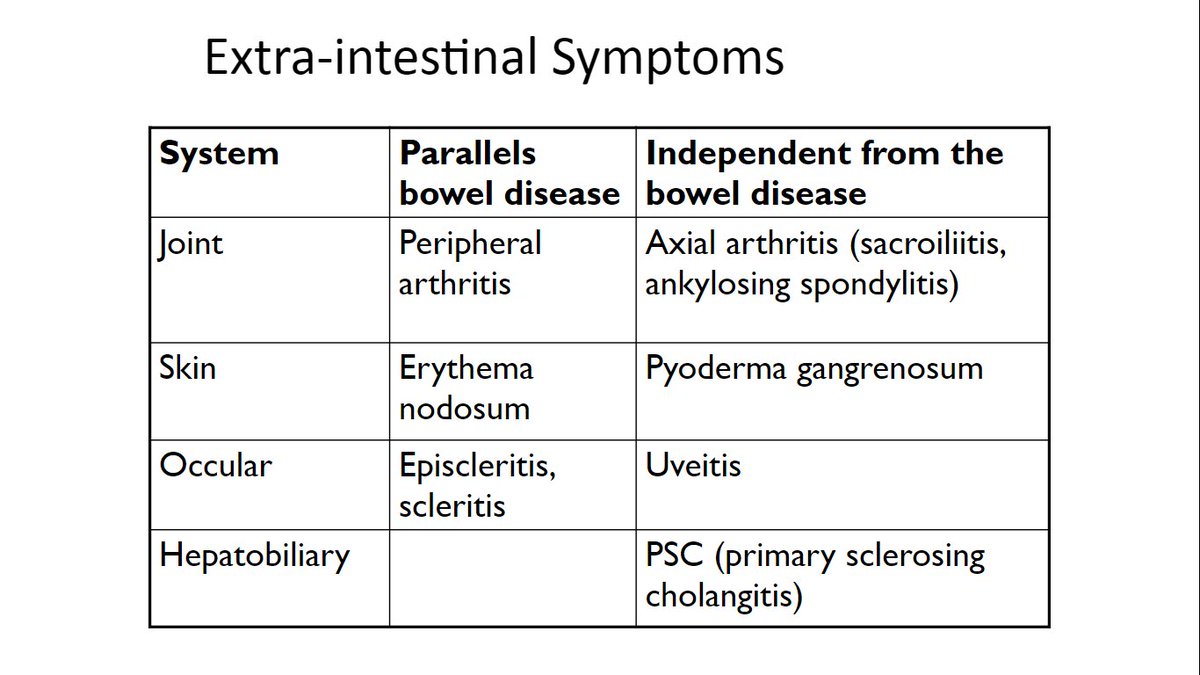
📍MC hepatobiliary EIM
📍Independent of IBD🔥:
->Can be dx before IBD manifest, or after total colectomy for UC
📍M>F
📍3rd-4th decade
@AmCollegeGastro
📍2-7% of UC have PSC
📍80% of PSC have IBD: UC>CD
✅C-scope in all new dx PSC w bx even if no GI Sx
📍MC hepatobiliary EIM
📍Independent of IBD🔥:
->Can be dx before IBD manifest, or after total colectomy for UC
📍M>F
📍3rd-4th decade
@AmCollegeGastro
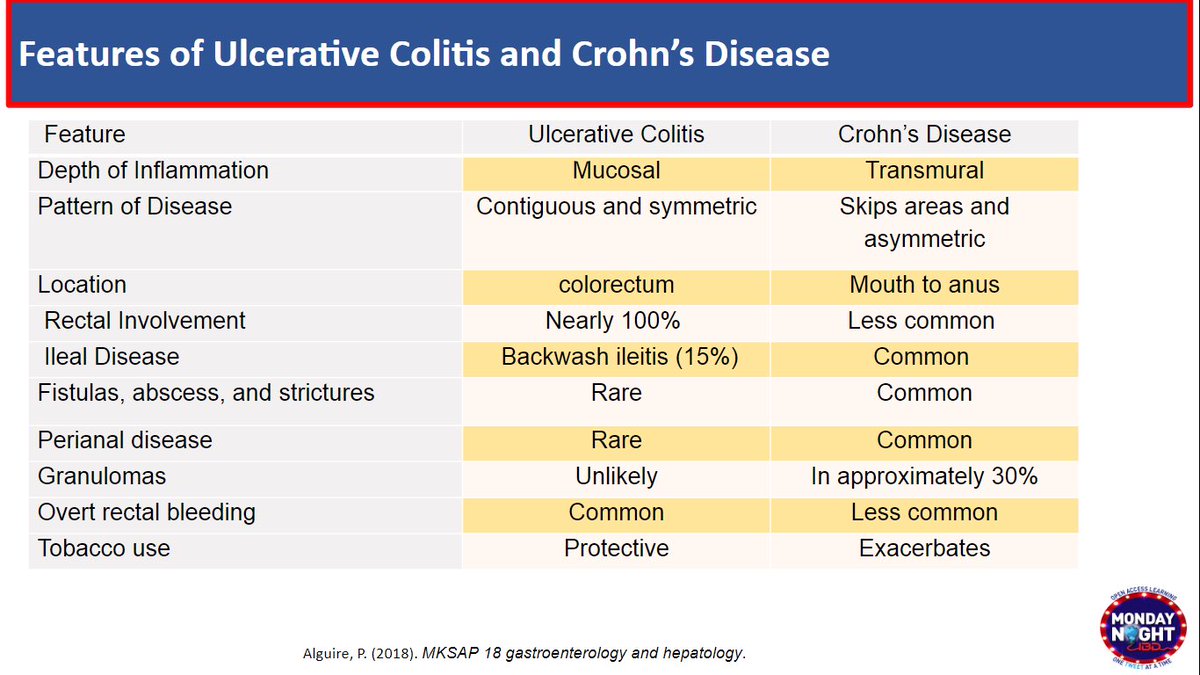
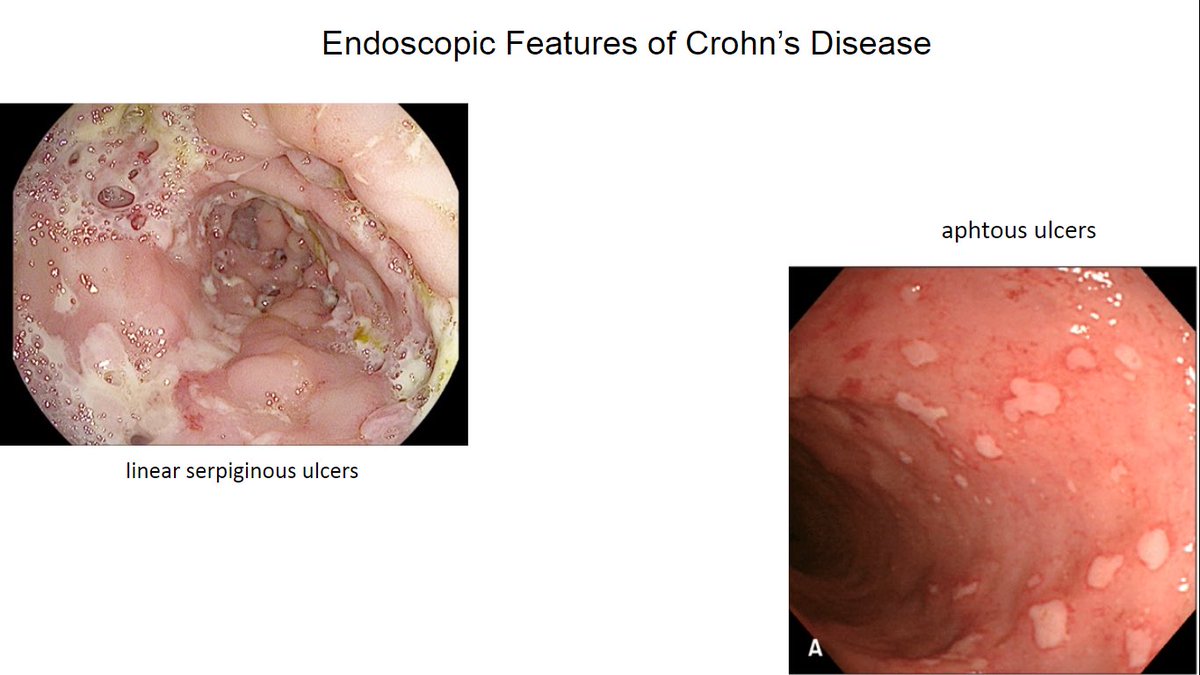
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro 5/💎#B2BPearl PSC-IBD phenotype
📌++MILD Pancolitis
💎Rectal sparing & Backwash ileitis-🚫 Crohns!
💎R disease>Left
💎Post-LT: 🔥can ⬆️or denovo IBD despite IS
📌⬆️ pouchitis post-IPAA (pouch+pre-pouch ileum🔥- 🚫 Crohns!
📌pHTN PSC-IBD:⬆️ risk of stomal &peristomal varices
📌++MILD Pancolitis
💎Rectal sparing & Backwash ileitis-🚫 Crohns!
💎R disease>Left
💎Post-LT: 🔥can ⬆️or denovo IBD despite IS
📌⬆️ pouchitis post-IPAA (pouch+pre-pouch ileum🔥- 🚫 Crohns!
📌pHTN PSC-IBD:⬆️ risk of stomal &peristomal varices

@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro 6/ #PSC Clinical manifestations
📌++ Asymptomatic ⬆️LFTs
💎#B2BPearl : Cholestatic pattern: ⬆️ALP, ⬆️GGT w moderate⬆️AST/ALT
💎Jaundice➡️🤔Cirrhosis🤔malignancy🤔Cholangitis
📌Pruritus, Fatigue
📌RUQ pain+Fever➡️🤔Cholangitis, typically post-ERCP
‼️Important DDx of PSC👇🏼
📌++ Asymptomatic ⬆️LFTs
💎#B2BPearl : Cholestatic pattern: ⬆️ALP, ⬆️GGT w moderate⬆️AST/ALT
💎Jaundice➡️🤔Cirrhosis🤔malignancy🤔Cholangitis
📌Pruritus, Fatigue
📌RUQ pain+Fever➡️🤔Cholangitis, typically post-ERCP
‼️Important DDx of PSC👇🏼

@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro 7/ #PSC diagnosis:
🔑 MRI/MRCP ++ , NOT ERCP
⚠️Pros:
〽️Less 💰 💴 💵
〽️Noninvasive
〽️ 🚫 risk of pancreatitis, cholangitis like ERCP
💎For CholangioCA , HCC surveillance
🔑 MRI/MRCP ++ , NOT ERCP
⚠️Pros:
〽️Less 💰 💴 💵
〽️Noninvasive
〽️ 🚫 risk of pancreatitis, cholangitis like ERCP
💎For CholangioCA , HCC surveillance

@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro 7b/ERCP 👉🏼done for Dx (brushing, bx, fluorescence in-situ hybridization - FISH) or Rx of complications only
🚩r/o CCA when dominant strictures (stenoses < 1.5mm in CBD or <1 mm in hepatic ducts)
🚩Sx relief from stricture: eg.balloon dilation
‼️Stenting ⬆️ risk of cholangitis
🚩r/o CCA when dominant strictures (stenoses < 1.5mm in CBD or <1 mm in hepatic ducts)
🚩Sx relief from stricture: eg.balloon dilation
‼️Stenting ⬆️ risk of cholangitis

@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro 8/ #PSC & ⬆️ risk of CA
🚩 ⬆️ Colon CA/ CCA / GB CA (less common pancreas, HCC)
🚩 ⬆️risk: age>20yo, M>F, IBD presence
💎 #B2BPearl PSC +GB polyps >8 mm👉🏼cholecystectomy / risk of GB CA
🔎HCC in PSC +cirrhosis➡️US/CT/MRI +/- α-fetoprotein q6mo doi.org/10.1016/j.cgh.…
@AGA_CGH
🚩 ⬆️ Colon CA/ CCA / GB CA (less common pancreas, HCC)
🚩 ⬆️risk: age>20yo, M>F, IBD presence
💎 #B2BPearl PSC +GB polyps >8 mm👉🏼cholecystectomy / risk of GB CA
🔎HCC in PSC +cirrhosis➡️US/CT/MRI +/- α-fetoprotein q6mo doi.org/10.1016/j.cgh.…
@AGA_CGH

@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro @AGA_CGH 9/ 🔎CCA in #PSC
🔍 Start at Dx
💎None for age <20yo or small-duct PSC
☑️US/CT/MRI +/- CA19-9 q6-12mo
☑️ If dominant stricture or ⬆️ symptoms/ cholestasis
➡️ERCP w/cytology, Bx, FISH to r/o CCA
💎🚫NO FNA of CA stricture if LT candidate (risk of tumor seeding)
@AGA_CGH
🔍 Start at Dx
💎None for age <20yo or small-duct PSC
☑️US/CT/MRI +/- CA19-9 q6-12mo
☑️ If dominant stricture or ⬆️ symptoms/ cholestasis
➡️ERCP w/cytology, Bx, FISH to r/o CCA
💎🚫NO FNA of CA stricture if LT candidate (risk of tumor seeding)
@AGA_CGH
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro @AGA_CGH 9b/ 🔎ColonCA in #PSC - #IBD
✔️Colonoscopy w/ Bx even in no GI symptoms to assess for associated colitis at time of PSC Dx
✔️💎Annual colon 👁 HDef scope or SDef w chromo, random + targeted bx
💎start at PSC dx ( 🚫wait for 7 yrs of IBD)
✔️Colonoscopy w/ Bx even in no GI symptoms to assess for associated colitis at time of PSC Dx
✔️💎Annual colon 👁 HDef scope or SDef w chromo, random + targeted bx
💎start at PSC dx ( 🚫wait for 7 yrs of IBD)
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro @AGA_CGH 10/ 🔶Indications for LT (definitive Rx)
🔷 Median time for progression of dis from dx until death/LT 10–12 yrs (5-yr survival of 80-85% w/ LT)
🔸Cirrhosis, MELD >15
🔸Recurrent cholangitis, >2 epis. bacteremia or >1 epis. sepsis
🔸CCA <3 cm in diameter, w/o mets, undergoing RCT
🔷 Median time for progression of dis from dx until death/LT 10–12 yrs (5-yr survival of 80-85% w/ LT)
🔸Cirrhosis, MELD >15
🔸Recurrent cholangitis, >2 epis. bacteremia or >1 epis. sepsis
🔸CCA <3 cm in diameter, w/o mets, undergoing RCT
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro @AGA_CGH 11/ #MondayNightIBD #B2B #PSC Recap
🪁 First sign: cholestatic liver enzymes
🪁 Dx: MRCP
🪁 ERCP if dominant strictures, r/o CCA
🪁 CCA surveillance→ US/CT/MRI +/- CA19-9 q6-12mo
🪁 PSC-IBD→ yearly colon surveillance at PSC dx
🪁 Follow w LT regarding timing of LT
🪁 First sign: cholestatic liver enzymes
🪁 Dx: MRCP
🪁 ERCP if dominant strictures, r/o CCA
🪁 CCA surveillance→ US/CT/MRI +/- CA19-9 q6-12mo
🪁 PSC-IBD→ yearly colon surveillance at PSC dx
🪁 Follow w LT regarding timing of LT
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro @AGA_CGH @DrMalSimons @LizzieAbyMD @SusanLouMD @hazhari_md @ptandonGI @HowardTLeeMD @TCotterMD @AdvaniRashmiMD @KapuriaMd @NabaSaeedQ @TrieuMD @JacquelineChuMD @MahamHayatMD @mohammad @VivyTCmd @joshsteinbergMD @javiervg0902 @anil_mythri @Waseem_AhmedMD @KM_Pawlak @AdamKichlerDO
@MondayNightIBD @SobiaMujtabaMD @NabilQuraishi @CholestasisDoc @DCharabaty @AmCollegeGastro @AGA_CGH And of course can’t forget this crowd favorite of our #PSC #IBDAlgorithm by #IBDAlgorithmMaster @joshsteinbergMD 

• • •
Missing some Tweet in this thread? You can try to
force a refresh