CDC's updated webpage on how COVID-19 is spread & prevention tips is now (almost) in line with science!
(WHO please do the same!)
(Hooray! only 10 months into epidemic & when Trump in hospital so maybe isn't paying attention?)
Thread
cdc.gov/coronavirus/20…
(WHO please do the same!)
(Hooray! only 10 months into epidemic & when Trump in hospital so maybe isn't paying attention?)
Thread
cdc.gov/coronavirus/20…
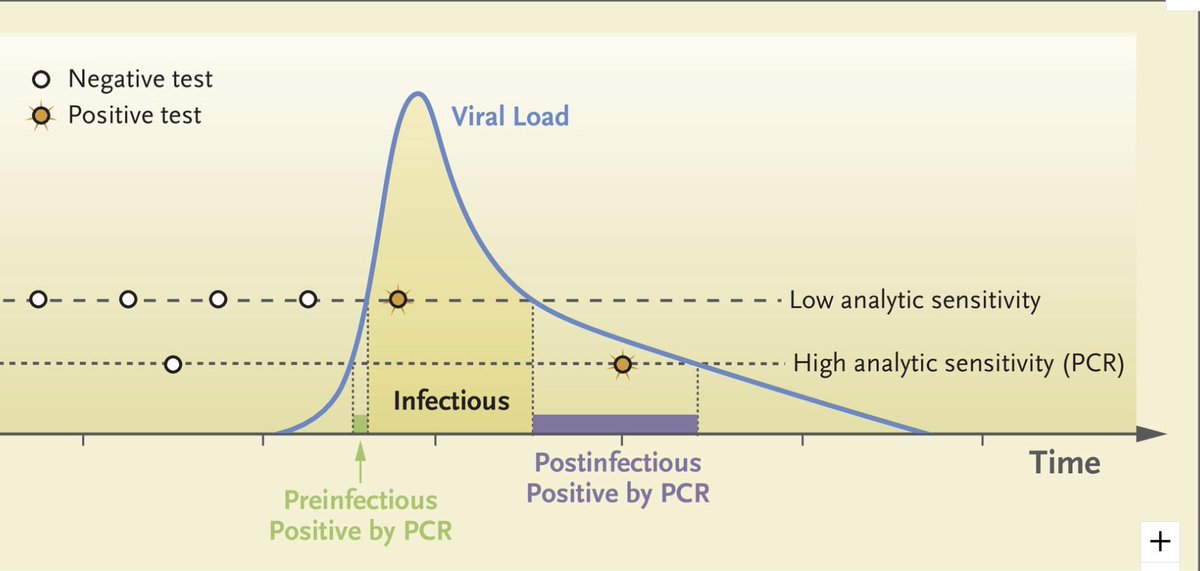
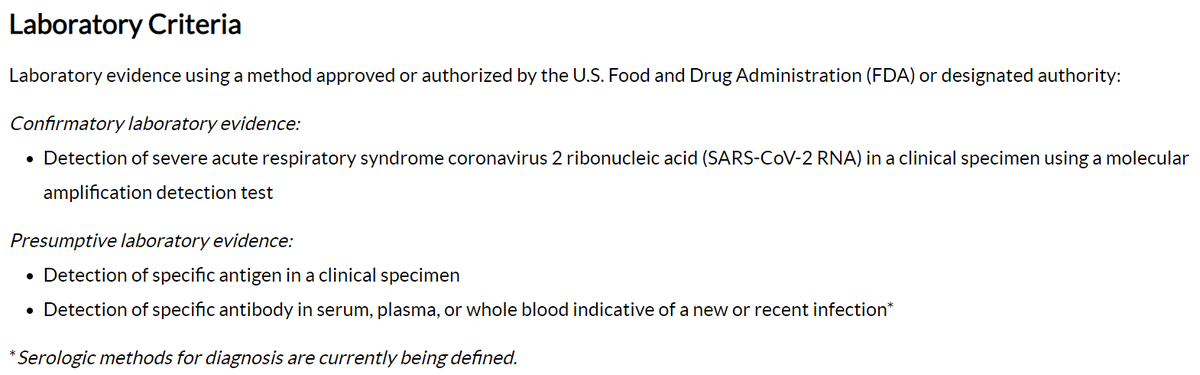
Webpage 1st summarizes dominant mode of transmission which is consistent with epidemiology data: mostly from people w/in 6' of each other & clearly states that people w/out symptoms (pre-symptomatic or asymptomatic) can transmit also! 

2. Website give ranking of how easily SARS-CoV-2/COVID-19 spreads relative to flu and measles.
(I'm not sure this is supported by data. R0 is higher than flu, but might be due to length of infectious period, not higher infectiousness. Anyone know of data to support/refute?)
(I'm not sure this is supported by data. R0 is higher than flu, but might be due to length of infectious period, not higher infectiousness. Anyone know of data to support/refute?)
3. Further details on main mode of spread (w/in 6'). Still focuses on "droplets" but also describes diffusion ("spread apart") of smaller particles. Some bullets aren't especially informative or helpful, but overall, much better. 

4. The big one! Direct acknowledgement that >6' "airborne" spread is possible. But wording is clear in stating that this mode is possible but rare & mostly in enclosed spaces (indoors, in vehicles) w/ poor ventilation. Great! 
5. Clear, big bold text stating that surface transmission is rare. This is huge. Still so many people and places worrying about gloves & cleaning & not indoors/outdoors or ventilation. 

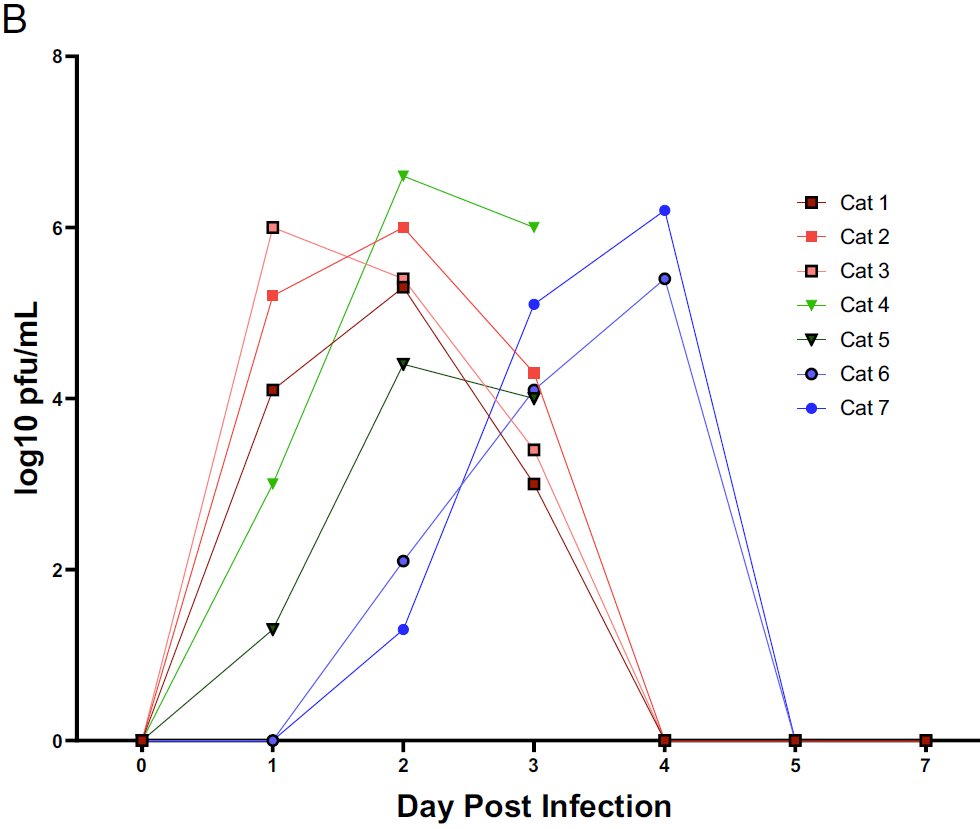
6. A little section about spread b/w humans & animals. Doesn't indicate that spread b/w cats is possible (pnas.org/content/early/…), but I haven't seen any data that this is important epidemiologically, so probably good overall summary. But keep cats indoors (for many reasons)! 

7. Prevention. I would have put this 1st!
Good: Distance & masks are 1st, 2nd
Less good: Ventilation, indoors/outdoors 4th (should be 3rd). Hand washing 3rd, & cleaning surfaces 7th.
Good: Distance & masks are 1st, 2nd
Less good: Ventilation, indoors/outdoors 4th (should be 3rd). Hand washing 3rd, & cleaning surfaces 7th.

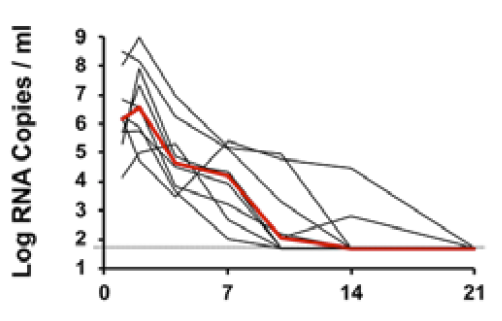
7. cont. Additions Needed: Emphasis to get tested immediately if mild symptoms. Need this for effective contact tracing. Delays of even a few days make a huge difference as we showed in recent paper (
https://twitter.com/DiseaseEcology/status/1304486025599660032).

Overall, a great improvement. I hope individuals, schools, organizations, companies adjust their prevention and risk assessment accordingly. Ventilation/setting (indoors/outdoors) is key (but distance and/or masks still needed outdoors)!
• • •
Missing some Tweet in this thread? You can try to
force a refresh