1. My talk today at #SHA2020 surgeon session re what #EXCEL really shows. To begin- need to understand importance of endpoints
➡️clinically relevant
➡️related to intervention
➡️relevant to pt
➡️similar prognostic impact in each arm
@SVRaoMD @ajaykirtane @RodrigoBagur @jedicath

➡️clinically relevant
➡️related to intervention
➡️relevant to pt
➡️similar prognostic impact in each arm
@SVRaoMD @ajaykirtane @RodrigoBagur @jedicath


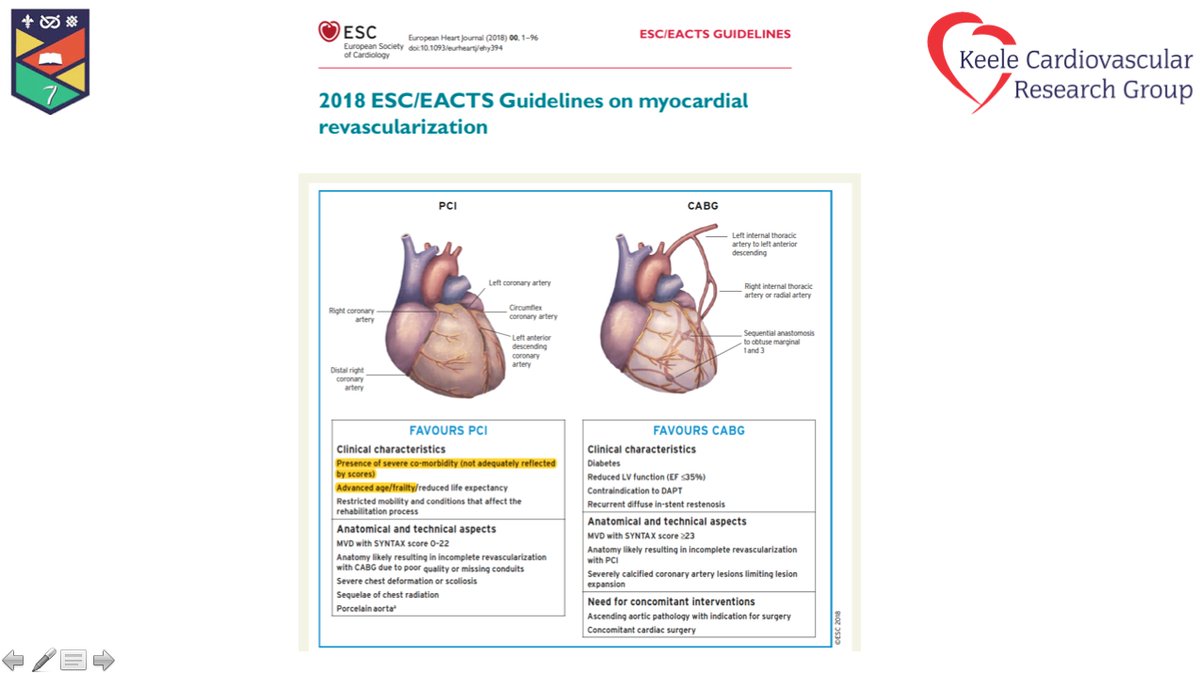
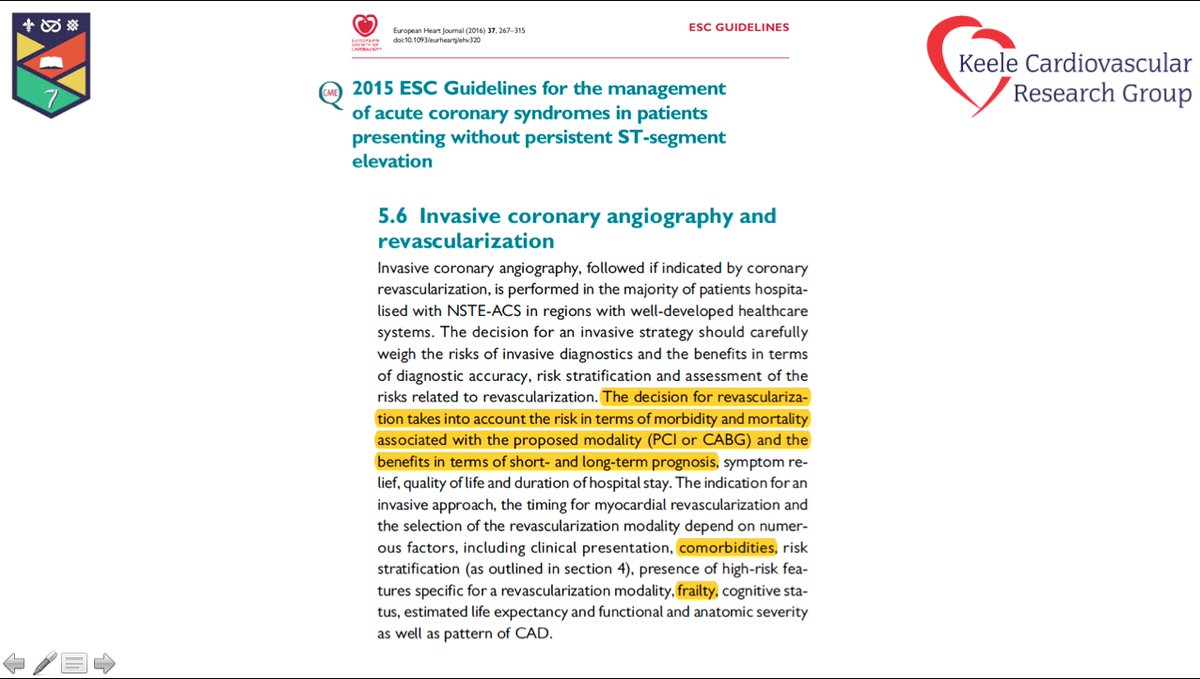
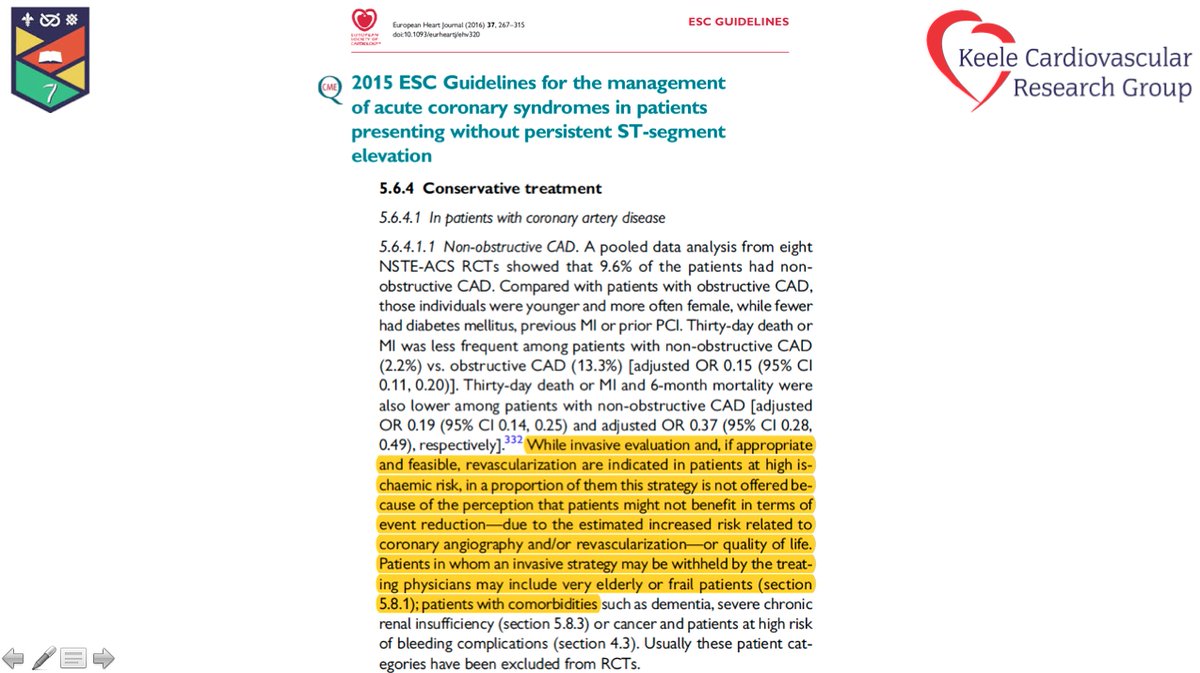
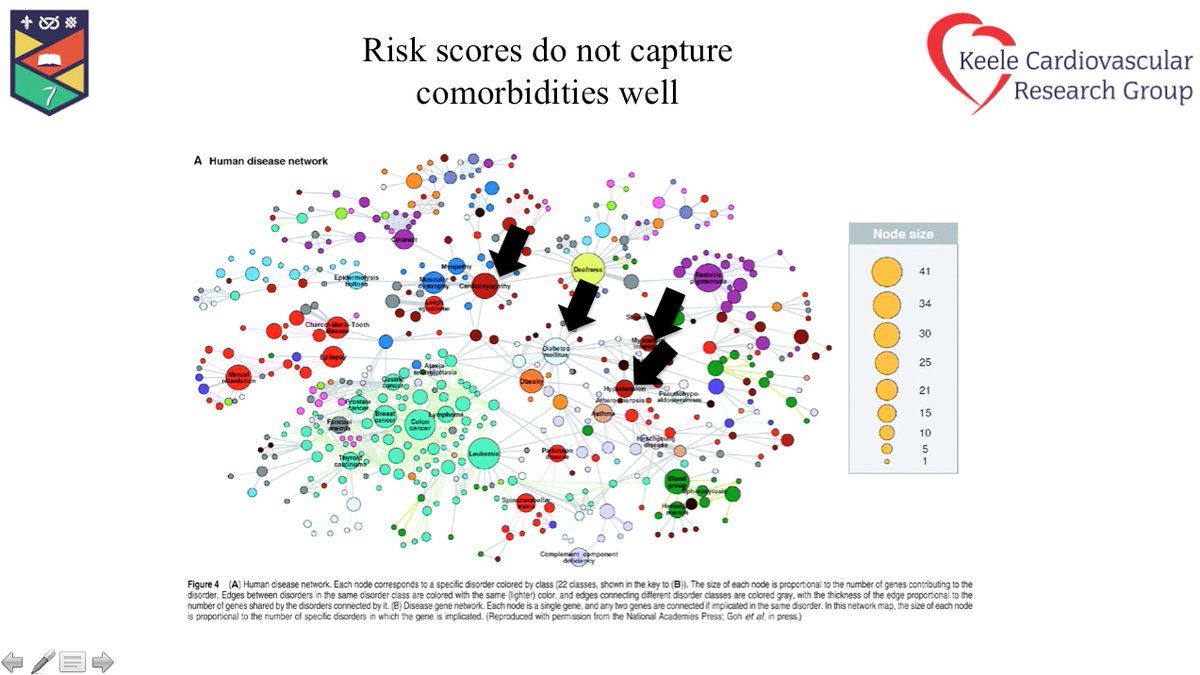
2. A significant proportion of LMS wont be suitable for either surgery / CABG. As heart teams we have to do better in stratifying by extent of disease - 1/4 of pts included in #EXCEL didnt meet inclusion criteria (low/ intermediate risk) @ovidiogarciav @aspergian1 @cardioPCImom 



3. The question of periporcedural AMI definition- depends on how you define re UDMI or protocol definition, will impact whether CABG 2x greater or 1/3 less. Personally i think protocol definition better as prognostic impact of AMI the same then in both arms (see pt 1)- BUT ➡️ 



4. when we look at non-procedural AMI (irrespective of how we define it) in longer terms- outcomes with surgery better ie AMI at 1-5 yrs using #EXCEL trial definition and the longer we follow up pts curves will seperate further @djc795 @Kfarooqi @kamalcardiodoc1 @saraceciliamtz 

5. We have thought that rpt revasc not prognostically significant- hence why not included in primary endpoint. CABG⬇️revasc mainly driven by ⬇️in non-target lesion but TVR. Should we include revasc as primary endpoint in trials? @hvanspall @biljana_parapid @purviparwani ➡️➡️ 

6. Going back to my first slide- yes! Revasc has an important prognostic impact in both total and CV mortality, and the prognostic impact is similar in both CABG and PCI @UjjwalRastogiMD @MohanedEgred @DrMauricioCohen @CESARJERONIMOVS @DrFerNunez @ferdikiem @omendiz 





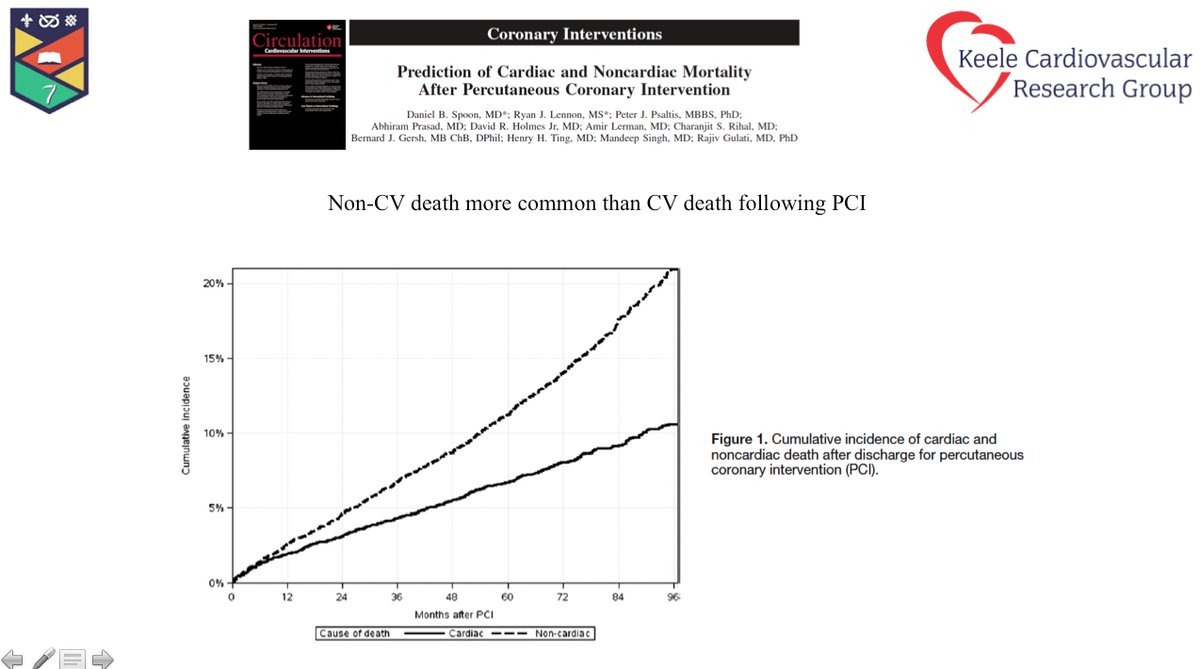
7. Now to the issue of death. ⬆️in death at 5 years- mainly driven by non CV deaths. Should this matter? YES- at the end of the day what matters to a pt is whether they are dead-not how. Taking totality of data at 5yrs though in all RCTs- no differences. @erodcauCCV 

8. 9.9% CABG and 13% PCI mortality at 5 years more than what a healthy 5-year mortality of a 66 (mean age in EXCEL) should be (3-5% depending on male vs female). #EXCEL showed that surgeons and IC not practicing optimal TX ie Imaging for PCI / Total arterial revasc surgery (BIMA) 

9. A few final thoughts pt 1.
➡️Mortality should be primary endpoint in such trials
➡️revasc more important than we thought
➡️ when deciding endpoints consider below
➡️NO PT outside of emergency should have LMS intervention without heart team discussion
➡️Mortality should be primary endpoint in such trials
➡️revasc more important than we thought
➡️ when deciding endpoints consider below
➡️NO PT outside of emergency should have LMS intervention without heart team discussion

10.
➡️ AMI endpoint in EXCEL used appropriate (see tweet above for reasoning)
➡️Guidelines need updating from what we have learnt- Much of this is from #EXCEL
➡️ Guidelines should be informed by indvidual pt meta-analysis from all RCT trials undertaken by independent group.
➡️ AMI endpoint in EXCEL used appropriate (see tweet above for reasoning)
➡️Guidelines need updating from what we have learnt- Much of this is from #EXCEL
➡️ Guidelines should be informed by indvidual pt meta-analysis from all RCT trials undertaken by independent group.
11. ➡️Whilst we can argue about minutae of #EXCEL - the fact that it has been done has provided all of us data that will inform best practice / tx of such pts. shouldn t lose sight of this @GreggWStone @ajaykirtane @ajpeace74 @SVRaoMD @Drroxmehran @Hragy
The End
The End
• • •
Missing some Tweet in this thread? You can try to
force a refresh